- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
The British Association of Urological Surgeons defines erectile dysfunction (ED) as “an inability to obtain or maintain an erection sufficient for penetration and for the satisfaction of both sexual partners.”1 Frequently termed impotence, the global prevalence of ED is estimated to be between 13.1% and 71.2%.2 Measurements vary by continent; however, in all cases, increasing age is a risk factor for acquiring the condition.2 Untreated, ED can lead to an increased risk of cardiovascular (CV) disease while similarly, a finding of ED may be a red herring for a patient’s undiagnosed CV disease (50% of patients with ED have atherosclerosis).3 However, patients may be hesitant to discuss ED concerns with a healthcare provider (HCP) due to embarrassment or misconceptions about the condition.4,5 Therefore, it is essential for HCPs to remain vigilant about screening those with suspected ED, for timely intervention to prevent future health consequences.6
Anatomy of the penis
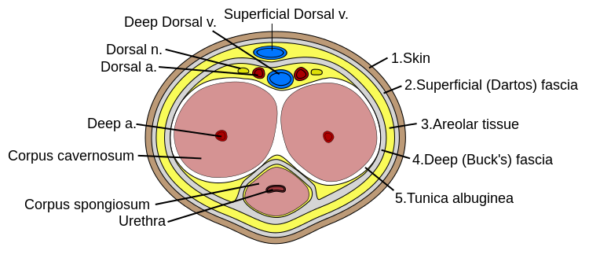
The penis is an organ of the male reproductive system, with associated musculature, blood supply, drainage and innervation (Figure 1). From proximal to distal, the penis is structured into the root, the main body and the glans/tip of the penis. Anchored at the root, are three bodies of erectile tissues: right and left corpus cavernosa and central corpus spongiosum. These tissues span the entire length of the penis and fill with blood upon sexual arousal. Four muscles work in tandem with this process to maintain erection and empty the urethra: bulbospongiosus (x2) and ischiocavernosus (x2). Surrounding the erectile tissues and muscles are three layers of fascial coverings, Dartos fascia, Buck’s fascia and Tunica albuginea, which serve to protect and support internal structures.
The penis is supplied by the dorsal penile artery, the deep penile artery and the bulbourethral artery, all which are derived from the internal pudendal artery. Venous drainage is via the superficial and deep dorsal veins to the superficial external pudendal vein and prostatic venous plexus, respectively. All penile innervation comes from S2-S4 spinal cord segments. Sympathetic penile innervation is provided by the pudendal nerve, which gives off the dorsal nerve of the penis, whereas parasympathetic innervation is from the prostatic nerve plexus which gives rise to the cavernous nerves.
Causes of ED
The cause of ED is frequently multifactorial, with mixed organic and psychogenic origins.8 For simplicity, it is best to broadly categorize the aetiology of ED into the following categories:
- Vascular: hypertension, atherosclerosis, hyperlipidemia, smoking
- Neurological: Parkinson’s disease, multiple sclerosis, stroke, spinal cord injury, peripheral neuropathy
- Hormonal: hypogonadism, hyperprolactinaemia, thyroid disease, Cushing’s disease
- Drug-induced: antihypertensives, beta-blockers, diuretics, antidepressants, antipsychotics, anticonvulsants, recreational drugs
- Systemic disease: diabetes mellitus, renal failure
- Structural: pelvic trauma, penile trauma, Peyronie’s disease
- Psychogenic: depression, anxiety, performance anxiety, schizophrenia
Note: Ascertaining whether a patient is having normal or impaired nocturnal erections will help to distinguish between organic vs. psychogenic causes of ED.
Clinical features
In cases of suspected ED, a thorough history and examination is necessary in order to ascertain the underlying cause of dysfunction.11,12 This will serve to inform management strategies for the patient. Clinical assessment of ED is frequently carried out by primary care providers, with referral to urology warranted for refractory, complex or uncertain cases. Chiefly, both history and examination should be undertaken in a private, safe environment, where patients are able to feel comfortable discussing their sexual history.
History
Patients with suspected ED will primarily complain of difficulties initiating or sustaining an erection. Further details surrounding these issues should be explored:
- Onset of sexual dysfunction (i.e. short, gradual)
- Duration of sexual dysfunction (i.e. lifetime or acquired)
- Difficulties with arousal
- Rigidity of erections
- Duration of sexual stimulation
- Difficulties with ejaculation
- Difficulties with orgasm
- Presence/absence of morning erections
The International Index of Erectile Function (IIEF-5) is an objective 5-item questionnaire frequently used by urologists to assess the severity of a patient’s ED. The tool asks patients to consider the following five questions on a scale of one to five over the last 6 months:13
- How do you rate your confidence that you could get and keep an erection?
- When you had erections with sexual stimulation, how often were your erections hard enough for penetration?
- During sexual intercourse, how often were you able to maintain your erection after you had penetrated your partner?
- During sexual intercourse, how difficult was it to maintain your erection to completion of intercourse?
- When you attempted sexual intercourse, how often was it satisfactory for you?
Other important areas of the history to cover include:
- Past medical history: previous sexual dysfunction, cardiovascular disease and previous pelvic surgery.
- Medication history: antihypertensives, beta-blockers, diuretics, antidepressants, antipsychotics, and anticonvulsants.
- Psychiatric history: current or previous psychological problems (e.g. depression, anxiety)
- Social history: smoking, alcohol consumption, illicit drug use, diet, exercise
- Sexual history: current sexual partner(s), relationship status, partner’s reaction to ED
It is crucial to explore the patient’s relationships with their sexual partners. If the cause of ED is thought to be psychogenic, the nature of these relationships will allow you to better understand the origins of the dysfunction. Relationship stress has been implicated with sexual dysfunction in men.14
Clinical examination
There are often no clinical signs present in patients with ED, although in some cases male genital examination may reveal structural abnormalities of the penis.
A general clinical examination may identify stigmata of underlying cardiovascular, endocrine or neurological disease which may be responsible for ED.
Investigations
Investigations should be selected based on the clinical judgement of the cause of ED. For instance, patients with vascular risk factors should undergo tests which evaluate cardiovascular risk status.
Blood tests
The following blood tests are used to rule out common underlying organic causes ED:15
- FBC
- LFTs
- U&Es
- TFTs
- Lipid profile
- Fasting glucose and/or HbA1C
- Serum total testosterone: if testosterone is reduced, serum prolactin will then be checked to screen for secondary hypogonadism
Specialised tests
In cases of complex or refractory ED, urologists may choose to perform an additional set of specialised tests:
- Nocturnal penile tumescence testing (NPT): used to distinguish between organic vs. psychogenic ED. The patient wears the NPT device overnight, measuring number, tumescence and rigidity of erections.
- Duplex doppler imaging/angiography: if a vascular cause of ED is suspected.
Management of ED
Increasingly, primary care physicians are managing ED with medical therapies alone.6 However, depending on the cause of ED, surgery may be warranted in specific cases. Both medical and surgical therapies for ED are discussed further below.16
Modification of risk factors
Where applicable, patients should be encouraged to adopt healthy lifestyle behaviours, including smoking cessation, minimal alcohol intake, and weight loss. Many of these risk factors are linked to cardiovascular disease and diabetes, among others, which are known to predispose to ED. Research shows that in many cases, addressing the lifestyle risk factors that predispose to ED, can significantly mitigate or eliminate the disease.17
If a medication is suspected to be the cause of the ED, consider substitution or withdrawal of this substance for 2 weeks and review the effect.
Psychosexual counselling
Patients may be referred for specialist counselling services if the cause of ED is considered to have a psychogenic component (either stand-alone or mixed) and if purely organic causes of ED have been ruled out.
Phosphodiesterase-5 inhibitors
Phosphodiesterase-5 inhibitors (PDE-5 inhibitors). These drugs arrest PDE-5, allowing for the prolongation of cGMP and subsequent relaxation of penile blood vessels (sildenafil, vardenafil, avanafil).
- Consult BNF for appropriate drug dosages (usually 25-100mg). Try drug at full dose prior to switching therapy. Frequency of use may vary with the severity of the patient’s ED.
- It is essential to counsel patients on the appropriate practice of PDE-5 inhibitors – take on an empty stomach 30 minutes prior to intercourse, avoid alcohol and fatty meals as it reduces drug absorption.
- The drug is intended to last for roughly 4 hours (if an erection lasts longer than 4 hours, the patient should seek urgent care for risk of priapism)
- PDE-5 contraindications include concurrent nitrate use. Caution is required when treating patients with cardiovascular or cerebrovascular disease in the previous 6 months (hypo/hypertension).
- PDE-5 side effects include headache, flushing, dizziness, dyspepsia and rhinitis
- Arrange follow-up at 6-8 weeks for review of treatment
- Alprostadil also comes in a topical cream and intraurethral application (MUSE) formulation which can be applied regularly by the patient at home prior to sexual intercourse.
- If a man presents with priapism after use of a PDE-5 inhibitor, defined as an erection lasting greater than 4 hours, urgent hospitalisation is required for further investigation and management.
Hormone treatments
Patients may be referred to an endocrinologist for hormone replacement if a deficiency in reproductive hormones is found on laboratory testing (e.g. low testosterone).
Penile prosthesis
Recommended as a surgical treatment for patients who have failed previous trials of management. Prosthetic options are inflatable implants vs. semirigid rods. In inflatable implants, the patient presses a pump which fills a surgically-implanted cylinder with fluid, thereby propelling an erection. Contrastingly, with semirigid rods, the penis remains rigid at all times and patients may choose to manoeuvre the device upwards to conceal their erection in times outwith sexual activity. Penile implants last for 10-15 years. The risks of prothesis are infection, implant malfunction and internal erosion/adhesion.
Prognosis of ED
If an underlying organic cause of ED is identified and reversible, the probability of curing ED is greatly increased. However, if refractory to various treatment modalities, patients with ED are at increased risk for psychiatric co-morbidities such as anxiety and depression. This may further generate relationship and interpersonal struggles, significantly affecting a patient’s quality of life. Moreover, ED is known to be a risk factor in itself for CV disease, therefore if left untreated, could predispose the patient to greater risks of stroke and coronary artery disease.3
Key points
- Erectile dysfunction (ED) is defined as an inability to obtain or maintain an erection sufficient for penetration and for the satisfaction of both sexual partners.
- The cause of ED is frequently multifactorial, with mixed organic and psychogenic origins.
- Patients with suspected ED will primarily complain of difficulties initiating or sustaining an erection.
- Other important areas of the history to cover include past medical history, medication history, psychiatric history, social history and sexual history.
- Investigations for ED include blood tests to rule out underlying causes and then further specialist investigations if appropriate.
- Management can include modification of risk factors, phosphodiesterase-5 inhibitors, psychosexual counselling, hormone therapy and penile prosthesis.
References
- Surgeons BA of U. Erectile dysfunction (impotence) [Internet]. 2019. [cited 2019 Dec 13]. Available from: [LINK]
- Kessler A, Sollie S, Challacombe B, Briggs K, Van Hemelrijck M. The global prevalence of erectile dysfunction: a review. BJU Int. 2019;124(4):587–99.
- Jackson G. Erectile dysfunction and cardiovascular disease. Arab J Urol [Internet]. 2013;11(3):212–6. Available from: [LINK]
- Gülpinar Ö, Haliloǧlu AH, Abdulmajed MI, Boǧa MS, Yaman Ö. Help-seeking interval in erectile dysfunction: Analysis of attitudes, beliefs, and factors affecting treatment-seeking interval in Turkish men with previously untreated erectile dysfunction. J Androl. 2012;33(4):624–8.
- Laumann EO, Glasser DB, Neves RCS, Moreira ED. A population-based survey of sexual activity, sexual problems and associated help-seeking behavior patterns in mature adults in the United States of America. Int J Impot Res. 2009;21(3):171–8.
- Grover SA, Lowensteyn I, Kaouache M, Marchand S, Coupal L, DeCarolis E, et al. The Prevalence of Erectile Dysfunction in the Primary Care Setting. Arch Intern Med. 2006;166(2):213.
- Commons W. File: Penis cross section [Internet]. [cited 2019 Dec 13]. Available from: [LINK]
- Lue TF. Erectile Dysfunction. N Engl J Med. 2000;(Table 1).
- Araujo AB, Durante R, Feldman HA, Goldstein I, Mckinlay JB. The relationship between depressive symptoms and male erectile dysfunction: Cross-sectional results from the Massachusetts male aging study. Psychosom Med. 1998;60(4):458–65.
- De Boer MK, Castelein S, Wiersma D, Schoevers RA, Knegtering H. The facts about sexual (dys)function in schizophrenia: An overview of clinically relevant findings. Schizophr Bull. 2015;41(3):674–86.
- Rosen RC. Evaluation of the patient with erectile dysfunction: History, questionnaires, and physical examination. Endocrine. 2004;23(2–3):107–11.
- Muneer A, Kalsi J, Nazareth I, Arya M. Erectile dysfunction. BMJ [Internet]. 2014;348(January):1–9. Available from: [LINK]
- Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peñ BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11(6):319–26.
- McCabe MP, Connaughton C. Sexual dysfunction and relationship stress: how does this association vary for men and women? Curr Opin Psychol [Internet]. 2017;13:81–4. Available from: [LINK]
- Khera M. Evaluation of Male Sexual Dysfunction [Internet]. UptoDate. 2019 [cited 2019 Dec 13]. Available from: [LINK]
- Society B, Medicine S, Scheme SL, Agency R. Erectile dysfunction QOF indicators QIPP – Options for local implementation. 2019;(August).
- Maiorino MI, Bellastella G, Esposito K. Lifestyle modifications and erectile dysfunction: What can be expected? Asian J Androl. 2015;17(1):5–10.
Reviewer
Nikita Bhatt
Urology Registrar