- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Being able to share information in a clear and concise way is an essential skill in all fields of medicine. This can range from simple explanations, such as why a blood test may be needed, to more complex situations, such as explaining a new diagnosis. Often, sharing information with a patient occurs naturally during a consultation. However, providing clinical information may also be the primary focus of an appointment, and in these situations, it is crucial to have a structured format in order to communicate more effectively.
This guide provides a step-by-step approach to explaining a diagnosis of glaucoma. You should also read our overview of how to effectively communicate information to patients.
Structuring your explanation
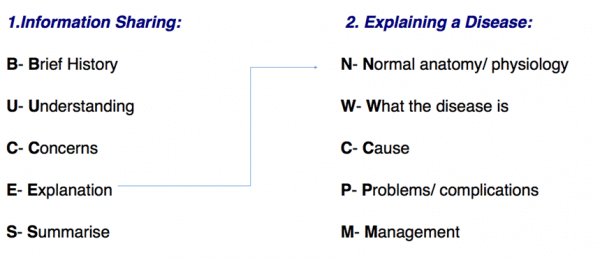
Explaining a diagnosis requires structure and adequate background knowledge of the disease. Whether the information being shared is about a procedure, a new drug or a disease, the BUCES structure (shown below) can be used.
Opening the consultation
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
BUCES can be used to remember how to structure a consultation in which providing information is the primary focus. Before explaining the various aspects of a disease, it is fundamental to have a common starting point with your patient. This helps to establish rapport and creates an open environment in which the patient can raise concerns, ask questions and gain a better understanding of their problem. After introducing yourself, it is important to take a brief history (this is the first part of the BUCES structure):
- What has brought the patient in to see you today?
- What are their symptoms, if any?
- Are there any risk factors that can be identified? (e.g. age, diabetes, cardiovascular disease, family history, being short-sighted)
For example, a patient may have recently had an eye test and were told they have ‘high pressures in their eye’, which is most often the case.
Tip: Practice taking concise histories to get the timing right. In OSCE stations, timing is crucial and you do not want to spend all your time taking a history when you are meant to be explaining a diagnosis! A rough guide would be to keep the introduction and brief history between 1-2 minutes maximum.
What does the patient understand?
Following a brief history, it is important to gauge the patient’s knowledge of their condition. Some patients may have a family member with glaucoma and therefore have a good understanding of what the condition entails. Other patients may have heard of glaucoma but only have a vague understanding of the important details.
Due to these reasons, it is important to start with open questioning. Good examples include:
- “Are you aware of the results of your recent eye test?”
- “What do you know about glaucoma?”
- “What has been explained to you about glaucoma so far?”
Open questioning should help you to determine what the patient currently understands, allowing you to tailor your explanation at an appropriate level.
At this stage, primarily focus on listening to the patient. It may also be helpful to give positive feedback as the patient talks (i.e. should a patient demonstrate some understanding, reinforce this knowledge with encouraging words and non-verbal communication such as nodding).
Checking the patient’s understanding should not be solely confined to this point of the consultation but should be done throughout by repeatedly ‘chunking and checking’.
Tip: Try using phrases such as: “Just to check that I am explaining glaucoma clearly, can you repeat back to me what you understand so far?”. This is far better than only saying “What do you understand so far?” as the onus is placed upon the quality of your explanation rather than there being an issue with the patient’s ability to understand.
What are the patient’s concerns?
The patient’s concerns should never be overlooked. A diagnosis of glaucoma can be significant and provoke a variety of worries. Asking the patient if they have any concerns before beginning your explanation allows you to specifically tailor what is most relevant to the patient, placing them at the centre of the explanation. The “ICE” (ideas, concerns and expectations) format, can provide a useful structure for exploring this area further.
ICE
Ideas:
- What does the patient think is causing their vision changes?
- What is their understanding of the diagnosis?
Concerns:
- What are the patient’s concerns regarding their symptoms and diagnosis?
Expectations:
- What is the patient hoping to get out of the consultation today?
Explanation
After determining the patient’s current level of understanding and concerns, you should be able to explain their condition clearly. Glaucoma and the various types can be confusing to medical students and doctors, let alone patients. Avoid medical jargon so as not to confuse your patient.
You should begin by signposting what you are going to explain to give the patient an idea of what to expect.
“I’m going to begin by talking about how the eyes work and then move on to discuss what glaucoma is and some of the risk factors. We’ll then discuss how we can manage it together and I’ll speak about some complications you need to be aware of.”
Tip: Use the mnemonic “Normally We Can Probably Manage” to help you remember the structure of explaining a disease.
Normal anatomy and physiology
“Your eyes produce a watery fluid called aqueous humour which is needed to provide nutrients and oxygen to the tissues within the eye. It also maintains the eye’s normal pressure and shape. This fluid is produced at the back of the eye, travels to the front and leaves via a sieve-like drainage system.”
What is primary open-angle glaucoma?
“Glaucoma is an eye condition where the optic nerve, which connects the eye to the brain, becomes damaged. It’s usually caused by fluid building up in the front of the eye, which increases the pressure in the eye. If not diagnosed, or if left untreated, this can lead to loss of vision.”
“There are multiple types of glaucoma, the most common being primary open-angle glaucoma. This type develops slowly over many years and is caused by the drainage channels in the eye becoming gradually clogged over time.”
“It’s a bit like a kitchen sink. Normally, if you switch the tap on, water leaves just as quickly via the drain. However, if you leave the tap on but this time you have a clogged drain, the sink gradually fills and will eventually overflow. In your eye, there is nowhere for this extra fluid to go, so the pressure increases within it and damages the nerve at the back of the eye.”
What are the risk factors and symptoms of glaucoma?
“Glaucoma is often picked up at a regular eye appointment when the pressures in your eyes are measured. With open-angle glaucoma, there are usually no early warning symptoms or signs. It is a disease that usually develops slowly and often you are unaware yourself of the sight loss. By the time you are aware of vision loss the disease can be quite advanced and can have progressed to tunnel vision. If left untreated it can ultimately cause blindness.”
“It’s unclear exactly why the drainage network in the eye clogs but there are multiple risk factors for this type of glaucoma, and these include:
- Increasing age
- Being short-sighted (myopic)
- Being of Afro-Caribbean ethnicity
- Smoking
- Having a family history of glaucoma”
Management
Aims of glaucoma management
“The primary aim of treating your glaucoma is to minimise the impact of the condition on your eyesight. If glaucoma is managed appropriately, we would expect it in most cases to have a minimal impact on your quality of life.”
Overview of glaucoma management
The main principles of glaucoma management include:
- Providing the patient with appropriate education to ensure good compliance with their medication and the importance of regular glaucoma checkups
- Checking for contraindications to medications (e.g. beta-blockers), for example, asthma
- Providing information on eye drops including method of application and common side effects
- Providing information management options if medical management (drops) do not work. For example, surgery and/or laser treatment. This would ultimately be discussed and decided upon in a secondary care setting.
Example
“We will discuss the management options for your glaucoma and decide on a suitable treatment plan together.”
“Management typically involves the use of eye drops and therefore ensuring you’re comfortable with when and how to put these in effectively is essential. It’s also important that you’re aware of some of the side effects of these medications and know that drops aren’t the only option. If they aren’t working or you’re unable to use the drops, we can consider a surgical approach (minimally invasive glaucoma surgery or a trabeculectomy).”
For more information on the topical therapies for glaucoma, see the Geeky Medics guide to common eye drops.
Regular check-ups
“Because of the increased risk of damage to your eyes, you will be invited for regular check-ups either at your local eye department or with an optometrist in the community. Here they will measure the pressure in your eyes (a technique known as tonometry) and look at an important part at the back of the eye known as the optic disc. They will also do regular visual field tests (to test ‘all round’ vision), but this won’t necessarily be done at each visit.”
Problems/complications of glaucoma
Outlining potential complications of glaucoma, including acute angle closure glaucoma, is necessary so that the patient can recognise problems early and take appropriate action.
A patient’s ability to drive can also be affected, and this can sometimes significantly impact their independence and ability to work.
This information needs to be delivered in a sensitive manner, whilst ensuring the patient is aware of the importance of treatment adherence and red flags that indicate the need for urgent medical attention.
Acute angle-closure glaucoma
“If you develop sudden intense eye pain and red eye or reduced/ blurred vision, you need to seek medical attention immediately. It could be that you have a sudden form of glaucoma where the drainage system has quickly become blocked, and the pressure has increased very rapidly. It is often accompanied by nausea and vomiting, headaches and seeing haloes around bright lights.”
Progression of glaucoma
“People with glaucoma are at risk of a worsening of their sight and eventually it can be severe enough to significantly affect their quality of life. It is important that you use the drops as and when is advised to reduce the risk of damage to your eyes and therefore blindness.”
Driving
“Because your eyesight gradually worsens with glaucoma and your brain tries to adapt for any loss of vision, you often have little awareness of your blind areas. This could lead to serious events whilst driving. It is therefore important that we make sure you meet the DVLA eyesight requirements, for both the safety of yourself and others.”
Further support for glaucoma
“There are many websites that can provide more information on glaucoma and provide more support. These include Glaucoma UK and the Royal National Institute of Blind People (RNIB)”
Closing the consultation
Summarise the key points back to the patient.
“We have discussed quite a lot today, including what glaucoma is, the symptoms you might experience and how the condition is managed. I realise this is a lot of information to take in and therefore I have a leaflet which summarises everything we’ve discussed. You will require regular checks to ensure your glaucoma continues to be well controlled. It is also important that you seek a review if you notice your vision worsening or have any other concerns.”
Ask the patient if they have any questions or concerns that have not been addressed.
“Is there anything I have explained that you’d like me to go over again?”
“Do you have any other questions before we finish?”
Direct the patient to further information about the condition using websites and leaflets.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Reviewer
Dr Caroline Sheldrick
Editor
Dr Chris Jefferies
References
- NHS. Glaucoma. 2022. Available from: [LINK]
- NICE. Glaucoma: diagnosis and management. 2022. Available from: [LINK]




