- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Hand and wrist examination frequently appear in OSCEs and you’ll be expected to identify the relevant clinical signs using your examination skills. This hand and wrist examination OSCE guide provides a clear step-by-step approach to examining the hand and wrist, with an included video demonstration. The hand and wrist examination can be broken down into five key components: look, feel, move, function and special tests. This can be helpful as an aide-memoire if you begin to feel like you’ve lost your way during an OSCE.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language: “Today I’m going to examine the bones of your hands and wrists. The examination will involve me first looking at the hands, then feeling the joints and finally asking you to do some movements.”
Gain consent to proceed with the examination.
Adequately expose the patient’s hands, wrist and elbows.
Position the patient seated with their hands on a pillow.
Ask the patient if they have any pain before proceeding with the clinical examination.
Look
General inspection
Clinical signs
Perform a brief general inspection of the patient, looking for signs suggestive of underlying pathology:
- Scars: may provide clues regarding previous upper limb surgery.
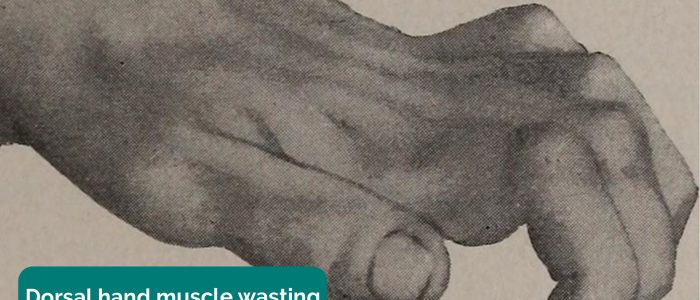
- Wasting of muscles: suggestive of disuse atrophy secondary to joint pathology or a lower motor neuron lesion.
Objects or equipment
Look for objects or equipment on or around the patient that may provide useful insights into their medical history and current clinical status:
- Aids and adaptations: splints are often used to manage hand and wrist pathology.
- Prescriptions: prescribing charts or personal prescriptions can provide useful information about the patient’s recent medications (e.g. analgesia).
Close inspection of the hand
Dorsal aspect of the hand
With the patient’s palms facing down, inspect the dorsum of each hand for signs suggestive of underlying pathology:
- Hand posture: note any abnormalities of hand posture which may indicate underlying pathology (e.g. Dupuytren’s contracture, ulnar deviation secondary to rheumatoid arthritis).
- Scars: inspect for evidence of scars which may indicate previous surgery or trauma.
- Swelling: note any areas of swelling, by comparing the hands and the wrists.
- Skin colour: erythema of the soft tissue may indicate cellulitis or joint sepsis
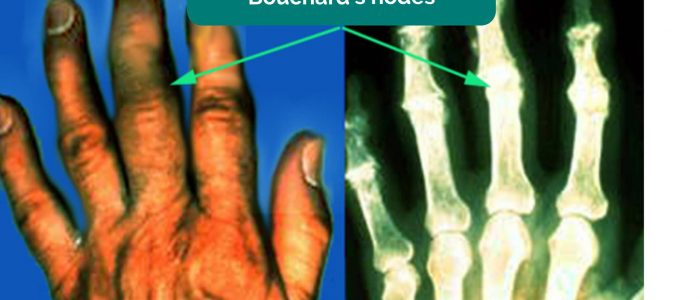
- Bouchard’s nodes: occur at the proximal interphalangeal joints (PIPJ) and are associated with osteoarthritis.
- Heberden’s nodes: occur at the distal interphalangeal joints (DIPJ) and are associated with osteoarthritis.
- Swan neck deformity: occurs at the distal interphalangeal joint (DIPJ) with clinical features including DIPJ flexion with PIPJ hyperextension. Swan neck deformity is typically associated with rheumatoid arthritis.
- Z-thumb: hyperextension of the interphalangeal joint, in addition to fixed flexion and subluxation of the metacarpophalangeal joint (MCPJ). Z-thumb is associated with rheumatoid arthritis.
- Boutonnières deformity: PIPJ flexion with DIPJ hyperextension associated with rheumatoid arthritis.
- Skin thinning or bruising: can be associated with long-term steroid use (e.g. common in patients with active inflammatory arthritis).
- Psoriatic plaques: salmon coloured plaques with a silvery scale. Patients who have psoriasis are at significantly increased risk of developing psoriatic arthritis.
- Muscle wasting: can occur secondary to chronic joint pathology or lower motor neuron lesions (e.g. median nerve damage secondary to carpal tunnel syndrome).
- Splinter haemorrhages: a longitudinal, red-brown haemorrhage under a nail that looks like a wood splinter. Causes include local trauma, infective endocarditis, sepsis, vasculitis and psoriatic nail disease.
- Nail pitting and onycholysis: associated with psoriasis and psoriatic arthritis.
Palmar aspect of the hand
With the patient’s palms facing up, inspect each hand for signs suggestive of underlying pathology:
- Hand posture: note any evidence of abnormal hand posture (e.g. clawed hand secondary to Dupuytren’s contracture).
- Scars: inspect for evidence of scars which may indicate previous surgery or trauma (e.g. carpal tunnel surgery).
- Swelling: note any areas of swelling, by comparing the hands and the wrists.
- Dupuytren’s contracture involves thickening of the palmar fascia, resulting in the development of cords of palmar fascia which eventually cause contracture deformities of the fingers and thumb.
- Thenar/hypothenar wasting: isolated wasting of the thenar eminence is suggestive of median nerve damage (e.g. carpal tunnel syndrome).
- Elbows: inspect for evidence of psoriatic plaques or rheumatoid nodules.
- Janeway lesions: non-tender, haemorrhagic lesions that occur on the thenar and hypothenar eminences of the palms (and soles). Janeway lesions are typically associated with infective endocarditis.
- Osler’s nodes: red-purple, slightly raised, tender lumps, often with a pale centre, typically found on the fingers or toes. They are typically associated with infective endocarditis.
Types of arthritis
Osteoarthritis (OA) is the most common form of arthritis and is characterised by joint pain worsened with activity, localised loss of cartilage, remodelling of adjacent bone and associated inflammation. Typical findings in the hands include swellings at the distal interphalangeal joints (Heberden’s nodes) and proximal interphalangeal joints (Bouchard’s nodes) which represent osteophyte formation. There is often associated crepitus and reduced range of joint movement.
Rheumatoid arthritis (RA) is an autoimmune disease characterised by inflammation of the synovial joints, periarticular tissue destruction and a variety of extra-articular features (e.g. rheumatoid nodules, scleritis, nail fold infarcts and peripheral nerve entrapment). Patients typically experience joint pain (present even at rest), joint swelling and morning joint stiffness. Typical findings in the hands include symmetrical joint inflammation typically affecting the proximal interphalangeal joints, metacarpophalangeal joints and wrist joints. Other features of RA in the hands include muscle wasting, ulnar deviation, swan neck deformity, Boutonnière’s deformity and Z-thumb deformity.
Psoriatic arthritis is an autoimmune disease associated with psoriasis that is characterised by inflammation of the joints and the surrounding tendons. Typical clinical features in the hands include joint swelling, joint pain and dactylitis (swelling of whole digits).
Feel
Palms up
Temperature
Assess and compare the temperature of the joints of the hand and elbow using the back of your hands.
Increased temperature of a joint, particularly if also associated with swelling and tenderness may indicate septic arthritis or inflammatory arthritis.
Radial and ulnar pulse
Palpate the radial and ulnar pulse to confirm adequate blood supply to the hand.
Thenar and hypothenar eminence bulk
Palpate the muscle bulk of the thenar and hypothenar eminences: wasting can be caused by disuse atrophy as well as lower motor neuron lesions (e.g. ulnar and median nerve).
Palmar thickening
Support the patient’s hand and palpate the palm to detect the typical bands of thickened palmar fascia associated with Dupuytren’s contracture.
Median and ulnar nerve sensation
1. Assess median nerve sensation over the thenar eminence and index finger.
2. Assess ulnar nerve sensation over the hypothenar eminence and little finger.
Palms down (dorsum)
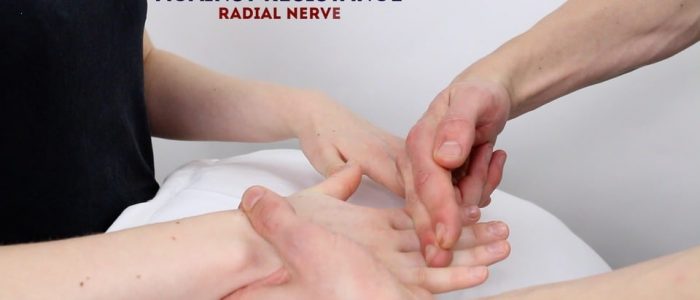
Radial nerve sensation
Assess radial nerve sensation over the first dorsal webspace.
Temperature
Assess and compare the temperature of the joints on the dorsal aspect of the hand (e.g. metacarpophalangeal joints) and elbow using the back of your hands.
Metacarpophalangeal joint squeeze
Gently squeeze across the metacarpophalangeal (MCP) joints and observe for verbal and non-verbal signs of discomfort. Tenderness is suggestive of active inflammatory arthropathy.
Bimanual joint palpation
Bimanually palpate the joints of the hand, assessing and comparing for tenderness, irregularities and warmth:
- Metacarpophalangeal joint (MCPJ)
- Proximal interphalangeal joint (PIPJ)
- Distal interphalangeal joint (DIPJ)
- Carpometacarpal joint (CMCJ) of the thumb (squaring of the joint is associated with OA)
Anatomical snuffbox
Palpate the anatomical snuffbox for tenderness which is suggestive of a scaphoid fracture.
Bimanual wrist palpation
Palpate the wrists for evidence of joint line irregularities or tenderness.
Elbows
Elbow palpation
Palpate the patient’s arm along the ulnar border to the elbow and note any tenderness, rheumatoid nodules or psoriatic plaques.
Scaphoid fracture
The scaphoid is the largest bone in the proximal row of carpal bones and is also the most commonly fractured. It often occurs due to a fall on an outstretched hand. As a result of the poor blood supply to the scaphoid, fractures can be slow to heal and avascular necrosis of the proximal fragment of the scaphoid can occur. Tenderness in the anatomical snuffbox is highly suggestive of a scaphoid fracture.
Move
The joints of the hand and wrist should be assessed and compared.
If the patient is known to have an issue with a particular hand, you should assess the ‘normal’ hand first for comparison.
Active movement
Active movement refers to a movement performed independently by the patient. Ask the patient to carry out a sequence of active movements to assess the function of various joints. As the patient performs each movement, note any restrictions in the range of the joint’s movement and also look for signs of discomfort.
It’s important to clearly explain and demonstrate each movement you expect the patient to perform to aid understanding.
Finger extension
Instructions: “Open your fist and splay your fingers.”
Finger flexion
Instructions: “Make a fist.”
Wrist extension
Normal range of movement: 90º
Instructions: “Put the palms of your hands together and extend your wrists fully.”
Wrist flexion
Normal range of movement: 90º
Instructions: “Put the backs of your hands together and flex your wrists fully.”
Passive movement
Passive movement refers to a movement of the patient, controlled by the examiner. This involves the patient relaxing and allowing you to move the joint freely to assess the full range of joint movement. It’s important to feel for crepitus as you move the joint (which can be associated with osteoarthritis) and observe any discomfort or restriction in the joint’s range of movement.
If abnormalities are noted on active movements (e.g. restricted range of movement), assess joint movements passively.
Ask the patient to fully relax and allow you to move their hand and wrist for them.
Warn them that should they experience any pain they should let you know immediately.
Repeat the above movements passively, feeling for any crepitus during the movement of the joint.
Motor assessment
The following screening test will allow you to quickly assess the motor function of the radial, ulnar and median nerve.
Wrist and finger extension against resistance
Nerve assessed: radial nerve
Muscles assessed: extensors of the wrist and fingers
Instructions:
1. Ask the patient to hold their arms out in front of them with their palms facing downwards –“Hold your arms out in front of you, with your palms facing the ground.”
2. Ask the patient to extend their fingers and wrist joints, keeping their hands in this position whilst you apply resistance – “Extend your fingers out in front of you, cock your wrists back and don’t let me pull them downwards.”
Index finger ABduction against resistance
Nerve assessed: ulnar nerve
Muscles assessed: first dorsal interosseous (FDI)
Instructions:
1. Ask the patient to splay their fingers and stop you from pushing their fingers together – “Splay your fingers outwards and don’t let me push them together.”
2. Apply resistance to the patient’s index finger using your own index finger to assess abduction.
Thumb ABduction against resistance
Nerve assessed: median nerve
Muscle assessed: abductor pollicis brevis
Instructions: Ask the patient to turn their hand over so their palm is facing upwards and to position their thumb over the midline of the palm. Advise them to keep it in this position whilst you apply downward resistance with your own thumb – “Point your thumbs to the ceiling and don’t let me push them down.”
Function
Assess the patient’s hand function using the fine motor screening tests below.
Power grip
Instructions: “Squeeze my fingers with your hands.”
Pincer grip
Instructions: “Squeeze my finger between your thumb and index finger.”
Pick up a small object
Instructions: “Could you please pick up the coin off the table.”
Special tests
Tinel’s test
Tinel’s test is used to identify median nerve compression and can be useful in the diagnosis of carpal tunnel syndrome.
To perform the test, simply tap over the carpal tunnel with your finger.
Interpretation
If the patient develops tingling in the thumb and radial two and a half fingers this is suggestive of median nerve compression.
Phalen’s test
If the history or examination findings are suggestive of carpal tunnel syndrome, Phalen’s test may be used to further support the diagnosis.
Ask the patient to hold their wrist in maximum forced flexion (pushing the dorsal surfaces of both hands together) for 60 seconds.
Interpretation
If the patient’s symptoms of carpal tunnel syndrome are reproduced then the test is positive (e.g burning, tingling or numb sensation in the thumb, index, middle and ring fingers).
Carpal tunnel syndrome
Carpal tunnel syndrome occurs as a result of compression of the median nerve as it traverses through the wrist via the carpal tunnel. Typical clinical features include pain and paraesthesia in the distribution of the median nerve (index finger, thumb and lateral half of the ring finger). Grip weakness can also develop secondary to wasting of the thenar muscles which receive motor innervation from the median nerve.
To complete the examination…
Explain to the patient that the examination is now finished.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Example summary
“Today I examined Mrs Smith, a 32-year-old female. On general inspection, the patient appeared comfortable at rest, with no stigmata of musculoskeletal disease. There were no objects or medical equipment around the bed of relevance.
“Assessment of the hands and wrists revealed a normal appearance with no tenderness on palpation. The range of movement of the joints in both hands was normal. There was no evidence of weakness or sensory disturbance in the hands. “
“In summary, these findings are consistent with a normal hand and wrist examination.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
- Neurovascular examination of the upper limbs.
- Examination of the elbow joint and shoulder joint.
- Further imaging if indicated (e.g. X-ray and MRI).
Reviewer
Mr Tejas Yarashi
Consultant Trauma & Orthopaedic Surgeon
References
-
James Heilman, MD. Adapted by Geeky Medics. Rheumatoid arthritis chronic changes. Licence: CC BY-SA.
-
David Jones. Adapted by Geeky Medics. Rheumatoid arthritis. Licence: CC BY 2.0.
-
Davplast. Adapted by Geeky Medics. Bouchard’s nodes. Licence: CC BY-SA.
-
Drahreg01. Adapted by Geeky Medics. Heberden’s nodes. Licence: CC BY-SA.
-
Phoenix119. Adapted by Geeky Medics. Swan neck deformity. Licence: CC BY-SA.
-
Alborz Fallah. Adapted by Geeky Medics. Boutonnière deformity. Licence: CC BY-SA.
-
James Heilman, MD. Adapted by Geeky Medics. Psoriasis plaque. Licence: CC BY-SA.
-
Hare, H. A. Adapted by Geeky Medics. Dorsal hand muscle wasting.
-
Splarka. Adapted by Geeky Medics. Splinter haemorrhage.
-
CopperKettle. Adapted by Geeky Medics. Onycholysis. Licence: CC BY-SA.
-
Frank C. Müller. Adapted by Geeky Medics. Dupuytren’s. Licence: CC BY-SA.
-
HenrykGerlach. Adapted by Geeky Medics. Carpal tunnel scars. Licence: CC BY-SA.
-
Starr, M. Allen. Adapted by Geeky Medics. Hypothenar wasting.
- GEMalone. Adapted by Geeky Medics. Ganglion. Licence: CC BY.