- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Wrist trauma is a common presentation to the emergency department and X-ray is typically the first-line investigation used to identify bony injuries. This guide provides a step-by-step approach to interpreting wrist X-rays and includes examples of the key pathology you may come across.
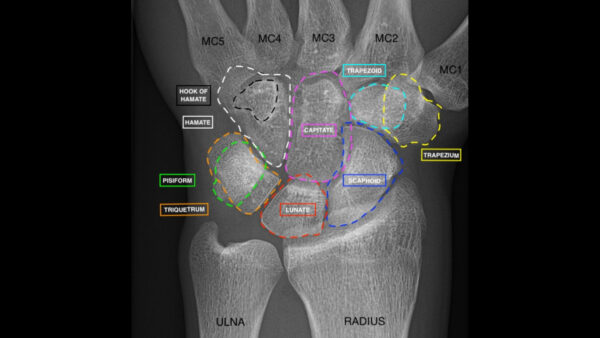
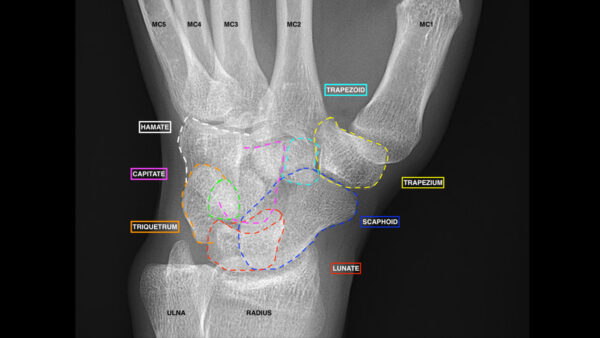
Anatomy
The intricate anatomy of the wrist makes wrist X-ray interpretation a challenging task.
The terms volar and palmar are used interchangeably to describe the palmar surface of the hand while the term dorsal is used to describe the back surface of the hand.
The main bones of the forearm are the ulna (medially, at the side of the little finger) and radius (laterally, at the side of the thumb). The wrist (carpus) is composed of 8 bones as remembered by the mnemonic ‘Some Lovers Try Positions That They Can’t Handle’:
- Scaphoid (proximal row)
- Lunate (proximal row)
- Triquetrum (proximal row)
- Pisiform (proximal row)
- Trapezium (distal row)
- Trapezoid (distal row)
- Capitate (distal row)
- Hamate (distal row)
Further details of the anatomical structure of the hand and wrist can be found in our overview of the bones of the hand.
Confirm the details
Begin by confirming you have the correct patient and the correct radiograph by assessing the following:
- Patient details (name, date of birth, unique identification number)
- Date and time the radiograph was taken
- Whether it is a radiograph of the left or right wrist
If previous radiographs are available, they should also be reviewed to provide a point of reference.
Interpretation
A structured approach to wrist X-ray interpretation is discussed below.
Step 1 – Views & adequacy
Views
There are two standard projections produced when a wrist X-ray is performed:
- Lateral
- Posterior-anterior (PA)
An oblique view may be obtained to provide additional views of the radial side of the wrist.
Ancillary views may be obtained depending on the clinical presentation and potential differential diagnoses.
Adequacy
Check the adequacy of the radiograph, it should include the distal radius and ulna with no overlap between the two bones.
Step 2 – Alignment
Check bony alignment on PA and lateral views.
Postero-anterior (PA) view
A PA view is typically obtained with the patient seated in the following position:
- Shoulder abducted to 90°
- Elbow flexed to 90°
- Forearm pronated
- Hand placed palm down in a neutral position with fingers extended on the X-ray plate
You can confirm that the hand/wrist is in a neutral position by drawing a line through the long axis of the radius, capitate and the third metacarpal (normal axes are within 10° of this line).
To assess alignment:
- Assess the distal radial contour which should appear smooth (any irregularities in the contour may indicate a fracture).
- Inspect the distal radial articular surface’s position; it should cup the carpal bones.
- Measure radial inclination; this is the angle of the distal radius surface with respect to a line perpendicular to the shaft (normal range is 21-25°). A greater than 25° radial inclination may suggest the presence of a fracture.
- Measure the radial length (a.k.a radial height); the distance between two lines drawn perpendicular to the long axis of the radius from the apex of the radial styloid and the level of the ulnar aspect of the articular surface (normal range 8-14mm). Loss of radial length/height may indicate the presence of an impacted radial fracture.
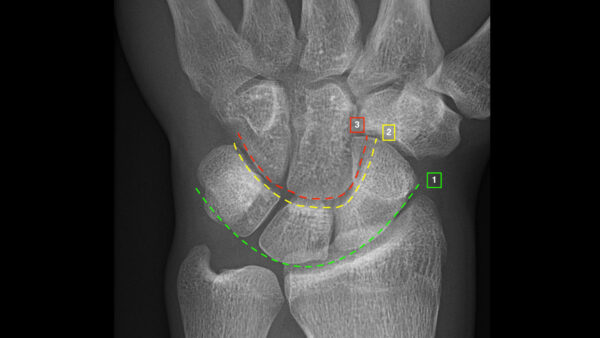
- Assess Gilula’s/carpal arcs; disruption to any of the arcs may suggest an underlying fracture or ligamentous injury (see Figure 2).
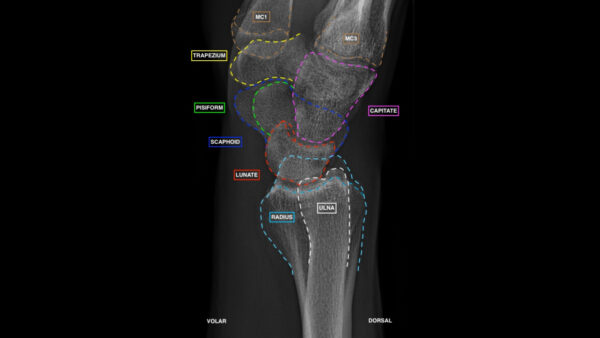
Lateral view
Lateral views of the wrist are technically challenging to interpret due to overlying bony structures.
This view is obtained by positioning the patient as follows:
- pronated wrist (ulnar side of the fifth digit facing down onto the X-ray plate)
- thumb facing upwards
Normal findings:
- The long axis of the radius, lunate, capitate and the third metacarpal bone should align.
- The palmar/volar cortex of the pisiform bone should lie between the scaphoid and capitate bones.
- The radial surfaces should appear smooth.
- There should be a volar tilt of between 10°- 25°.
The volar tilt (palmar tilt) is a measurement made on the lateral view. This is the angle between a line along the distal radial articular surfaces and a line perpendicular to the longitudinal axis of the radial shaft. The average volar tilt is approximately 11° and can range from 2°-20°.1
Tip: the lunate can be identified by its moon-shaped appearance and the scaphoid and capitate can be identified by their association.
Oblique view
An oblique view is obtained by pronating the hand 45° from the position used for a lateral view.
It provides additional views of:
- the radial side of the wrist
- radiocarpal joint
- scaphoid
- scaphotrapeziotrapezoidal joints
Ancillary views
Ancillary views can be obtained if required to confirm a diagnosis.
Examples of ancillary views include:
- Dynamic PA and lateral images
- Clenched fist images
- Carpal tunnel views
A scaphoid series can be requested if there is clinical suspicion of a scaphoid fracture, this involves imaging the scaphoid in at least three directions; PA, lateral, oblique and/or angled PA view.
Step 3 – Bones
Assess the cortical margin and trabecular pattern of all bones:
- Radius: assess the visible portion of bone to ensure no distal or proximal fractures
- Ulna: inspect the ulnar styloid to ensure the cortex is intact, if not, avulsion may be indicative of other abnormalities such as a distal radial fracture
- Carpal bones: pay careful attention to the proximal row and the scaphoid bone as it is the most frequently injured and consequently has an increased risk of avascular necrosis
- Metacarpals: whilst X-rays are not as sensitive as dual-energy X-ray absorptiometry (DEXA), a thinning of the cortex (<25% of the whole thickness of metacarpal) of tubular bones can signify osteoporosis
An overview of common fracture types is included later in this article.
Step 4 – Articulation
Assess for abnormal articular joint spaces.
Intercarpal joint spaces should be 1-2mm, increased or decreased joint space is indicative of pathology.
Step 5 – Soft tissue
Assess soft tissue structures to ensure no overt abnormalities.
Common injuries
Retrospective studies have shown that wrist trauma accounts for 1.5% of emergency department presentations.2
A fall onto an outstretched hand (FOOSH) is the most common mechanism of injury.
Common pathologies
Distal radius
There are different classifications of distal radial fractures:
- Fernandez (based on mechanism of injury)
- Frykman (based on joint involvement)
- Melone (subdivides intra-articular fractures)
- AO distal radius classification
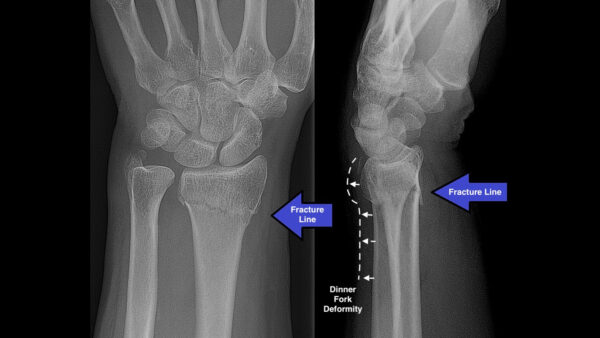
Colles fracture
A Colles fracture is an extra-articular bowing fracture usually caused by a FOOSH whilst in dorsiflexion.
It is the most common type of wrist fracture and it has a bimodal distribution (young athletes and the elderly).
Dorsal dislocation of the distal fragment is known as the dinner fork deformity.
Colles fractures are associated with:
- Radial shortening
- Avulsion of the ulnar styloid process
- Carpal bone fractures/misalignment
On X-ray, the degree of dorsal angulation and the degree of displacement should be noted.
The medial joint line should be observed to ensure that the radioulnar joint is preserved.
Smith fracture
Smith fractures are generally caused by falling onto the dorsal surface of a wrist in palmar flexion (as a result they are sometimes referred to as a ‘reverse Colles fracture’).
Smith fractures are less common than Colles fractures, but they also have a bimodal distribution typically affecting the young and elderly females.
Palmar angulation of the distal fragment is typically observed. Fractures can be extra-articular (outside the joint), juxta-articular (besides the joint) or intra-articular (within the joint).

Barton fracture
Barton fractures are intra-articular shear fractures of the distal radius.
The fractures can be either dorsal (standard Barton fracture) or volar (reverse Barton fracture) depending on where the oblique fracture line lies.
Barton fractures are usually associated with subluxation/dislocation of the radiocarpal joint.

Distal radioulnar joint dislocation
If the joint space between the distal radius and ulna is greater than 2mm as seen on the PA film, a distal radioulnar dislocation should be suspected. A lateral view can assist in the diagnosis.
Carpal bones
Scaphoid fractures
Scaphoid fractures account for 60-70% of all carpal bone fractures and are most common in young active patients after a FOOSH.3
Scaphoid fractures are commonly missed on radiographs, therefore, a scaphoid series should be carried out to comprehensively assess the scaphoid bone.
Scaphoid fractures are typically categorised by their location (e.g. proximal, middle or distal), but can also be categorised based on the axes of the fracture (e.g. transverse, oblique/horizontal or vertical).
The following should be assessed when viewing the carpal bones on an X-ray:
- Cortical disruption: an interruption in the continuity of the radiopaque (white) outermost layer of bone (>1mm may indicate instability)
- Intra-articular involvement: involvement of the joint surface
- Angulation or displacement of the fracture: notable displacement of fracture fragments
- Scapholunate interval: increased or decreased space between the scaphoid and lunate bone
- Lunate dislocation
- Other associated fractures (e.g. Colles fracture)
- Signs of avascular necrosis (older injuries/fractures): appears as increased density (radiopacity) due to decreased blood supply
- Soft tissue injury (e.g. scaphoid fat pad sign – the scaphoid fat pad is a small triangular or linear radiolucent area of fat to the radial side of the scaphoid bone. If the fat pad is displaced or obliterated then this is known as a positive fat pad sign.
If no fracture is visible, but there is high clinical suspicion of fracture, a repeat scaphoid series should be performed following an interval of approximately one week.

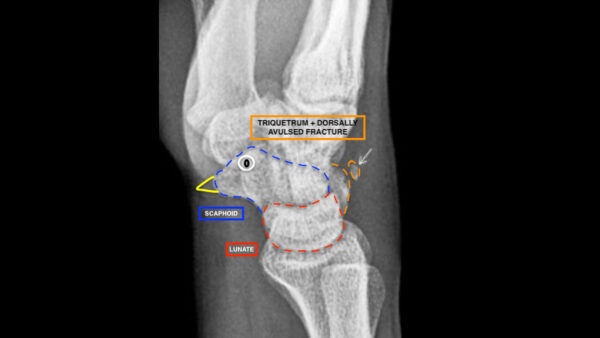
Triquetral fracture
Triquetral fractures are the second most common carpal bone fracture subtype and may be seen in isolation or as part of a complex carpal fracture.
The most common method of injury is FOOSH on the dorsiflexed hand in ulnar deviation causing impingement, shear force or avulsion.
Triquetral fractures are generally easiest to identify on a lateral view and often not visible on a PA view.
A dorsal avulsion fracture is the most common subtype, which has the following features:
- Avulsed piece of bone is seen dorsally to the triquetrum
- Avulsion of the dorsal triquetral ligament (known as the “pooping duck sign”)
Perilunate dislocation
Perilunate dislocation is often confused with lunate dislocation (lunate dislocations are relatively uncommon and can be distinguished by having no articulation with radius or capitate). Perilunate dislocations occur secondary to high impact trauma, typically from falling onto a dorsiflexed wrist.
Perilunate dislocation is best viewed on a lateral view (it is often overlooked on the PA view).
The radio-lunate articulation remains intact, however, the capitate does not articulate and sits dislocated (not in the lunate cup) in the dorsal direction. The radius and capitate remain aligned.
Soft tissue injuries
X-ray is not the optimal imaging modality for assessing soft tissue damage in the wrist. Swelling around an area of bony damage may be visible. Radiographs should be reviewed for signs of injury such as the scaphoid fat pad sign, but MRI is a more suitable modality for the evaluation of soft tissue injuries.
Summary
Wrist radiographs are an important first-line investigation in wrist trauma and a systematic approach to their interpretation is essential.
A failure to identify fractures of the wrist can result in a range of complications including:
- Delayed union
- Non-union
- Avascular necrosis
- Arthritis
- Joint instability
- Chronic pain
References
- Mann Fa, Kang Sw, Gilula La. Normal Palmar Tilt: is Dorsal Tilting Really Normal? Journal of Hand Surgery. 1992;17(3):315-317. doi:10.1016/0266-7681(92)90120-Q
- Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001 Sep;26(5):908-15. doi: 10.1053/jhsu.2001.26322. PMID: 11561245.
- Hayat Z, Varacallo M. Scaphoid Wrist Fracture. [Updated 2021 Apr 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. https://www.ncbi.nlm.nih.gov/books/NBK536907/
Figure references
- Mikael Häggström, M.D. Licence: CC0, via Wikimedia Commons.
- Lucien Monfils, CC BY-SA 3.0 via Wikimedia Commons.
- James Heilman, MD, CC BY-SA 4.0 via Wikimedia Commons.
- Gilo1969, CC BY 3.0 via Wikimedia Commons
- Tyson S, Hatem SF, Easily Missed Fractures of the Upper Extremity, Radiologic Clinics of North America, Volume 53, Issue 4, 2015, Pages 717-736, ISSN 0033-8389, ISBN 9780323391177.