- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Musculoskeletal (MSK) X-ray interpretation can occasionally feature in OSCEs and therefore it’s important to practice this skill to develop a structured approach. This guide provides a brief overview of MSK X-ray interpretation, including a structured approach you can apply to most X-rays and examples of relevant pathology.
Confirm details
Always begin by checking the details discussed below.
Patient details
Confirm the patient’s details:
- Full name
- Date of birth (DOB)
- Unique identifier (e.g. hospital number)
Film details
Confirm the details of the radiograph:
- Date and time the film was taken
- The area of the body scanned
- Adequacy of the film:
- Views: it is good practice have a minimum of 2 projections, this is because many fractures are not visible on a single view (‘a single view is no view’)
- Ideally the joint above and below should both be imaged
- Rotation
- Penetration
Previous imaging
Previous images provide a baseline for comparison.
X-ray interpretation (ABCS approach)
The ABCS approach of X-ray interpretation involves assessing the following:
- Alignment and joint space
- Bone texture
- Cortices
- Soft tissues
General points
Don’t forget to review all views, compare both sides and re‐examine any previous imaging.
If you spot one abnormality, do not lose focus until you have reviewed all areas of the image, otherwise, you might miss important pathology.
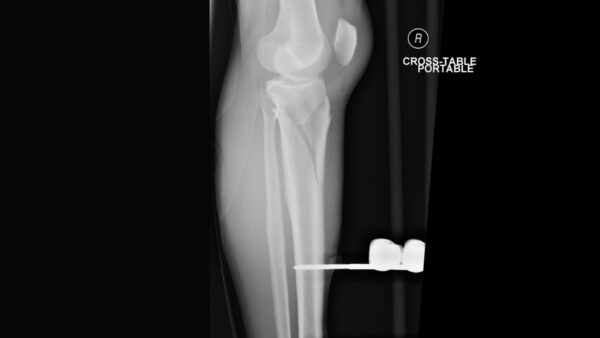
Alignment and joint space
Changes in alignment suggest a fracture, subluxation (partial dislocation) or dislocation.
When describing the displacement, the position of the fragment distal to the fracture site is always described.
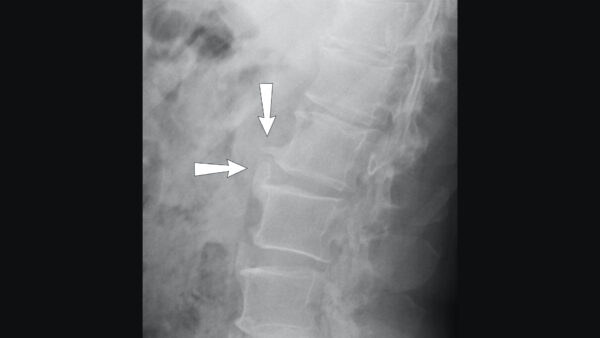
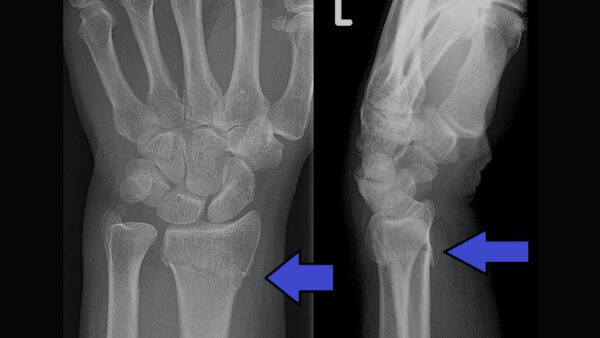
The radiograph below demonstrates why it is important to have more than one view.

Carefully look at the joint space to identify changes such as joint space narrowing due to cartilage loss, cartilage calcification (as in chondrocalcinosis) or new bone formation (e.g. osteophytes). Subchondral sclerosis (increased bone density) is often present along the joint lines in patients with osteoarthritis.
Bone texture
Altered density or disruption in the usual internal matrix of fine white lines (trabeculae) within the substance of the bone and the thick external covering (cortex) may indicate pathology.
Cortices
Trace around the outline of each bone as any step in the cortex may indicate a fracture or other pathology.
Infection and tumours (primary and secondary) are the commonest causes of bony destruction.
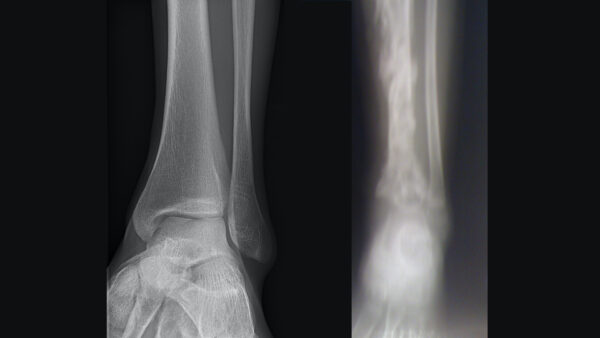
A periosteal reaction is the formation of new bone in response to injury or other stimuli of the periosteum surrounding the bone. It may be the only sign visible to denote a problem with the bone (stress or healing fracture, mild osteomyelitis or tumour).
Soft tissues
Look for any swelling, foreign bodies or effusions. Sometimes soft tissue injuries are easier to visualise and can prompt a closer inspection for bony pathology.
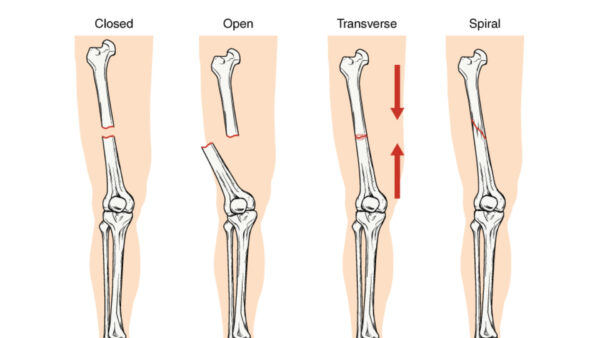
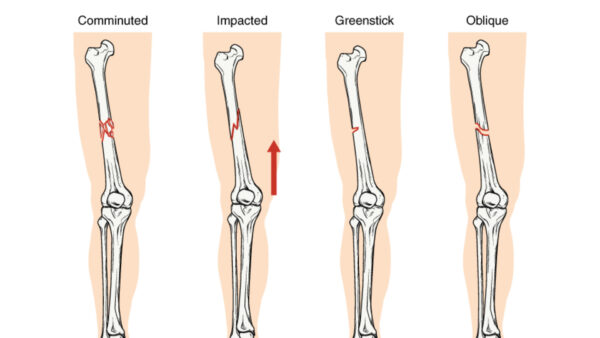
Types of fractures
There are several different types of fracture including:
- Closed fracture
- Open fracture
- Transverse fracture
- Spiral fracture
- Comminuted fracture
- Impacted fracture
- Greenstick fracture
- Oblique fracture
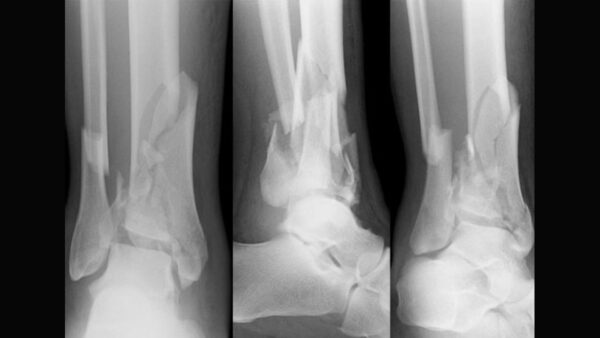
Describing a fracture
Fracture descriptors depend on the class of bone and the direction of the fracture line.
Where is the fracture?
Describe which bone is involved and where the fracture is located (proximal/middle/distal).
State whether there is any involvement of the articular surface (as this may alter management).
What type of fracture?
Complete fracture
A complete fracture involves the fracture extending all the way through the bone.
Types of complete fractures include:
- Transverse: fracture at right angles to the shaft
- Oblique: fracture at an angle to the shaft
- Spiral: caused by twisting injury
- Comminuted: 2 or more bone fragments
- Impacted: fractured bone forced together
Incomplete fracture
Incomplete fractures do not involve the whole cortex (i.e. not all the way through the bone) and most commonly occur in children.
Types of incomplete fractures include:
- Torus/Buckle: a bulge in the cortex
- Bowing: associated bend in the bone shaft
- Greenstick: bending of the shaft with a fracture on the convex surface
- Salter-Harris: involving the growth plate
Open or closed fracture
If a fracture is associated with a puncture of the skin or open wound, this is classed as an open fracture.
If not, then it is termed closed.
This is important to state because of the risk of infection with open fractures.
Is there displacement?
Displacement is described in terms of the distal fragment to the body (e.g. anterior/posterior).
Displacement can also involve:
- Angulation: changes in the axis of the bone, usually described as dorsal/palmar or varus/valgus or radial/ulnar.
- Translation: movement of the fractured bones away from each other. Described using the width of the bone as context (e.g. translation of 25% of the width of the bone). If translation is further away than the width of the bone, it is said to be ‘off-ended’.
- Rotation: usually difficult to appreciate on an x-ray.
Key points
- By applying a structured approach to musculoskeletal X-ray interpretation you reduce the risk of missing pathology.
- Always begin X-ray interpretation by carefully checking the details of the patient and radiograph.
- The ABCS approach provides a generic framework to assess most types of X-rays (alignment and joint space, bone texture, cortices and soft tissues).
- There are several sub-types of fractures, each associated with different mechanisms of injury and patient factors.
- When assessing a fracture, apply a structured approach paying particular attention to the location, type and displacement of the fracture.
Reviewer
Dr Edward Twimasi
Consultant Radiologist
References
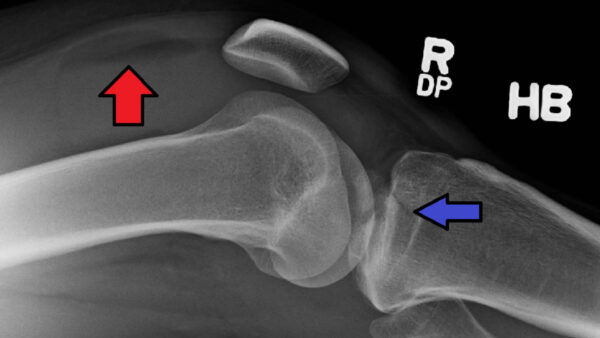
- Hellerhoff. Adapted by Geeky Medics. Joint dislocation of the metacarpophalangeal joint. Licence: [CC BY-SA].
- James Heilman, MD. Adapted by Geeky Medics. Knee X-ray. Licence: [CC BY-SA].
- Mikael Häggström, M.D. Adapted by Geeky Medics. Lumbar spine X-ray. Licence: [CC BY-SA].
- sarindam7. Adapted by Geeky Medics. Osteomyelitis. Licence: [CC BY-SA].
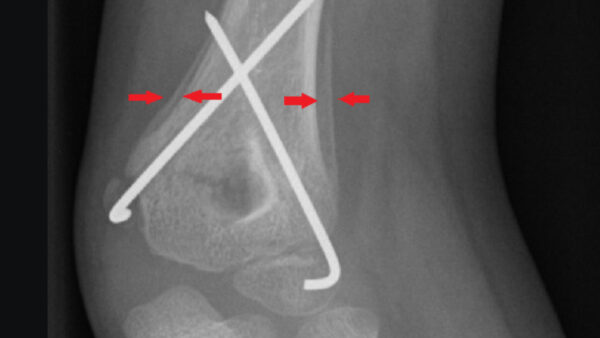
- Mikael Häggström. Adapted by Geeky Medics. Ankle X-ray. Licence: [CC BY-SA].
- Roberto J. Galindo. Adapted by Geeky Medics. Hand fracture. Licence: [CC BY-SA].
- Lindsay Davidson, annotated by Mikael Häggström. Adapted by Geeky Medics. Periosteal reaction. Licence: [CC BY-SA].
- Yousef Samir. Adapted by Geeky Medics. Osteosarcoma. Licence: [CC BY-SA].
- Mikael Häggström. Adapted by Geeky Medics. Knee effusion. Licence: [CC BY-SA].
- James Heilman, MD. Adapted by Geeky Medics. Lipohaemarthrosis. Licence: [CC BY-SA].
- Openstax college. Anatomy & Physiology, Connexions Web site. Adapted by Geeky Medics. Types of fractures. Licence: [CC BY-SA].
- Jane Agnes. Adapted by Geeky Medics. Transverse fracture. Licence: [CC BY-SA].
- Yasuo Kida on Flickr. Adapted by Geeky Medics. Oblique fracture. Licence: [CC BY-SA].
- RSJThompson. Adapted by Geeky Medics. Spiral fracture. Licence: [CC BY-SA].
- Elhehir. Adapted by Geeky Medics. Comminuted fracture. Licence: [CC BY-SA].
- Lucien Monfils. Adapted by Geeky Medics. Colles fracture. Licence: [CC BY-SA].
- Hellerhoff. Adapted by Geeky Medics. Greenstick fracture. Licence: [CC BY-SA].
- James Heilman, MD. Adapted by Geeky Medics. Salter-Harris fracture. Licence: [CC BY-SA].