- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Peripheral venous examination (also known as varicose vein examination) frequently appears in OSCEs. You’ll be expected to pick up the relevant clinical signs of venous disease using your examination skills. This venous examination OSCE guide provides a clear step-by-step approach to examining the venous system.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language: “Today I need to examine the veins in your legs. This will involve me first looking at the veins, then feeling the veins and performing some special tests. You’ll need to take your trousers off for the examination, but you can keep your underwear on.”
Explain the need for a chaperone: “One of the ward staff members will be present throughout the examination, acting as a chaperone, would that be ok?”
Gain consent to proceed with the examination.
Adequately expose the patient’s lower limbs.
Position the patient standing.
Ask the patient if they have any pain before proceeding with the clinical examination.
General inspection
Clinical signs
Inspect the patient from the end of the bed whilst at rest, looking for clinical signs suggestive of underlying pathology:
- Scars: may indicate previous surgical procedures or healed ulcers.
- Ulcers: indicative of venous and/or arterial disease.
Objects and equipment
Look for objects or equipment on or around the patient that may provide useful insights into their medical history and current clinical status:
- Medical equipment: note any compression stockings and wound dressings.
- Mobility aids: items such as wheelchairs and walking aids give an indication of the patient’s current mobility status.
- Vital signs: charts on which vital signs are recorded will give an indication of the patient’s current clinical status and how their physiological parameters have changed over time.
- Prescriptions: prescribing charts or personal prescriptions can provide useful information about the patient’s recent medications.
Leg inspection
With the patient standing (if able) look for signs of venous disease from the front, side and back of the legs.
Surgical scars
Surgical scars may be relevant to the patient’s presentation. It is worth clarifying what operation the patient had by asking the patient and confirming with their medical records if able.
It is important to note that modern venous treatments are now minimally invasive and therefore they’ll be no scars (NICE now recommends minimally invasive surgery for varicose veins as first-line treatment). Traditional treatment in the past did result in a low groin scar on the affected side.
Venous eczema
Venous eczema occurs as a result of venous hypertension causing fluid to collect in the tissues. The stasis of this fluid in the soft tissues results in activation of the innate immune response and subsequent inflammation.
Venous eczema has the following clinical characteristics:
- Itchy red, blistered and crusted plaques; or dry fissured and scaly plaques on one or both lower legs (commonly mistaken for cellulitis).
- Atrophie blanche: star-shaped ivory-white depressed atrophic plaques with red dots within the scar (dilated capillaries) and surrounding hyperpigmentation (due to haemosiderin deposition).
- Orange-brown patches of pigmentation caused by haemosiderin deposition.
- Lipodermatosclerosis (described below).
If you’re not sure if the patient has venous eczema, ask “Is it itchy?”. Varicose eczema is often intensely pruritic and a this is a common indication for intervention.
Lipodermatosclerosis
Lipodermatosclerosis is a form of panniculitis (inflammation of the subcutaneous fat) caused by ongoing activation of the innate immune response in soft tissues (secondary to venous hypertension).
It is an advanced manifestation of chronic venous insufficiency (CVI). Varicose veins are a common cause of CVI with other causes including deep venous incompetence and calf muscle pump failure.
Lipodermatosclerosis has the following clinical characteristics:
- Skin hardening (often referred to as induration)
- Hyperpigmentation
- Erythema
- Swelling
- Inverted champagne bottle appearance
Venous ulcers
Venous ulcers are thought to be caused by the improper functioning of venous valves and typically develop along the medial aspect of the distal leg. A venous ulcer can be defined as a full-thickness defect of the skin that fails to heal spontaneously and is sustained by chronic venous disease.
Venous ulcers present with the following clinical characteristics:
- Large, irregular border with sloping edges
- Shallow depth
- Often located over the medial aspect of the ankle (referred to as the gaiter region).
- Associated with mild pain
Venous ulcers differ significantly from arterial ulcers which are often significantly more painful, smaller in size and deeper with clearly defined borders.
Saphena varix
A saphena varix is a dilation of the saphenous vein at its junction with the femoral vein in the groin. It typically presents as a lump around 2-4cm inferior-lateral to the pubic tubercle. It often has a bluish tinge, is soft to palpate and will vanish when the patient lies down which can help differentiate it from an inguinal hernia.
Arterial disease
Arterial disease is important to be aware of when assessing and treating problems of the venous system. One of the common treatment options for varicose veins is compression therapy (with compression stockings or bandages). If a patient has a significant degree of arterial disease they may not be suitable for compression therapy due to the risk of secondary ischaemia. Likewise, if the patient has venous ulcers, the first step in management is to ensure there is adequate arterial supply before trying to treat superficial venous disease.
Clinical signs of peripheral arterial disease include:
- Peripheral pallor
- Peripheral cyanosis: bluish discolouration of the skin associated with low SpO2 in the affected tissues.
- Reduced temperature
- Gangrene: tissue necrosis secondary to inadequate perfusion. Typical appearances include a change in skin colour (e.g. red, black) and breakdown of the associated tissue.
- Hair loss: associated with PVD due to chronic impairment of tissue perfusion.
- Arterial ulcers: typically small, well-defined, deep ulcers that are very painful. These ulcers most commonly develop in the most peripheral regions of a limb (e.g. the ends of digits).
Varicose veins
Varicose veins appear as tortuous dilated superficial veins. The location of the varicose vein can help inform you as to which part of the venous system is likely to be affected.
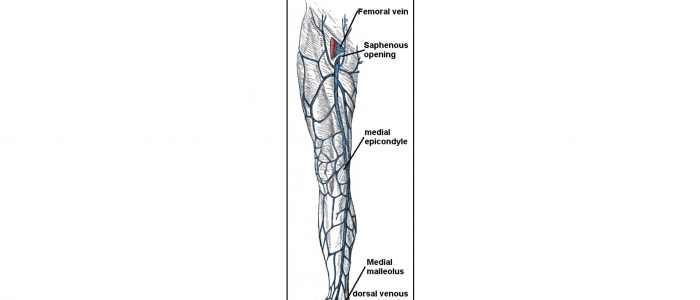
Great saphenous vein
The great saphenous vein originates at the merging of the dorsal vein of the big toe with the dorsal venous arch of the foot. After passing in front of the medial malleolus (where it often can be visualized and palpated), it runs up the medial side of the leg (classically known as the trouser seam). At the knee, it runs over the posterior border of the medial epicondyle of the femur bone. In the proximal anterior thigh 3-4 centimetres inferolateral to the pubic tubercle, the great saphenous vein dives down deep through the cribriform fascia of the saphenous opening to join the femoral vein. ¹
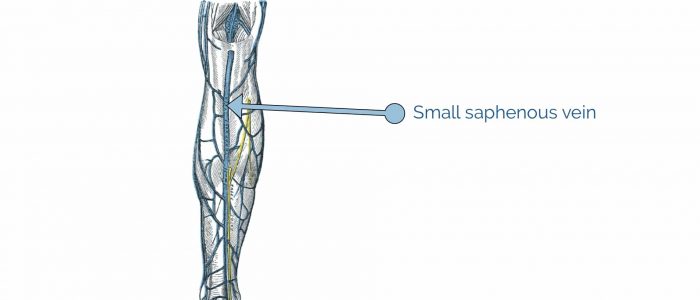
Small saphenous vein
The small saphenous vein originates at the merging of the dorsal vein of the fifth digit with the dorsal venous arch of the foot. From its origin, it courses around the lateral aspect of the foot (inferior and posterior to the lateral malleolus) and runs along the posterior aspect of the leg, where it passes between the heads of the gastrocnemius muscle. The small saphenous vein drains into the popliteal vein, at or above the level of the knee joint.² The saphenopopliteal junction (SPJ) is anatomically more variable in position compared to the saphenofemoral junction (SFJ).
Summary
In summary, the great saphenous vein runs all the way up the medial side of the leg and the small saphenous vein drains the lateral side of the lower leg. Varicose veins on the buttocks and around the genitals are suggestive of pathology affecting the venous system within the pelvis.
Assess varicosities
Temperature
Assess the temperature of any varicosities:
- Place the back of your hand along the varicosities to assess their temperature.
- Increased temperature is indicative of inflammation (e.g. phlebitis).
Palpation
Palpate any visible varicosities:
- Palpate the entire length of each varicosity and ask the patient to let you know if they experience any pain.
- Overlying erythema in the distribution of the vessel and tenderness on palpation is indicative of phlebitis.
- A tender and hard (“cord-like”) varicosity is indicative of thrombophlebitis (thrombosis with associated inflammation).
Phlebitis
Phlebitis is the term used to describe inflammation of a vein. Phlebitis most commonly occurs in superficial veins and is typically caused by trauma and/or infection (e.g. secondary to insertion of an intravenous cannula). In a small number of cases, it is caused by systemic inflammatory disorders such as lupus.
Further assessment of the lower limb
Pitting oedema
Assess for pitting oedema in the limb:
- Apply some pressure with a fingertip above the medial malleolus for a few seconds and then remove to see if an indentation has been left behind (e.g. known as pitting oedema).
- Continue to move upwards along the leg, repeating this process until you establish at what level oedema extends to.
- Pitting oedema is most commonly caused by heart failure and its presence can impact the integrity of the skin, complicating the management of venous disease.
Lower limb pulses
Palpate the pulses in the lower limbs to assess the arterial blood supply of each leg.
When assessing the pulses of the lower limbs work proximal to distal – this allows you to assess and compare arterial inflow into each leg. If pulses are not palpable, a Doppler can be used to assess blood flow through a vessel.
Femoral pulse
Palpate the femoral pulse:
- The femoral pulse can be palpated at the mid-inguinal point, which is located halfway between the anterior superior iliac spine and the pubic symphysis.
- Check that the pulse is present and assess the pulse volume.
Popliteal pulse
Palpate the popliteal pulse:
- The popliteal pulse can be palpated in the inferior region of the popliteal fossa.
- With the patient lying on the bed, ask them to relax their legs and place your thumbs on the tibial tuberosity.
- Passively flex the patient’s knee to 30º as you curl your fingers into the popliteal fossa. This should allow you to feel the pulse, as you compress the popliteal artery against the tibia.
- This pulse is often difficult to palpate, so don’t pretend you can feel it if you can’t. The popliteal artery is one of the deepest structures within the fossa, so the examiner will understand if you are unable to locate the artery.
Posterior tibial pulse
Palpate the posterior tibial pulse:
- The posterior tibial pulse can be located posterior to the medial malleolus of the tibia.
- Palpate the pulse to confirm its presence and then compare pulse strength between the feet.
Dorsalis pedis pulse
Palpate the dorsalis pedis pulse:
- The dorsalis pedis pulse can be located over the dorsum of the foot, lateral to the extensor hallucis longus tendon, over the second and third cuneiform bones.
- Palpate the pulse to confirm its presence and then compare pulse strength between the feet.
Percussion (tap test)
The tap test provides a crude assessment of lower limb venous valve competency. It is rarely performed in modern clinical practice, but it is worth understanding what the test involves.
To perform the tap test:
1. Place one finger, with a small amount of pressure, onto the saphenofemoral junction (SFJ) which is located 4cm inferior-lateral to the pubic tubercle.
2. Tap the varicose vein you are assessing, which should be located lower down the leg.
3. If your finger over the SFJ detects a thrill, this suggests that there is continuity of the vein due to incompetent venous valves (normally the venous valves should prevent the thrill transmitting along the entirety of the vessel).
Auscultation
Again, auscultation is rarely performed in modern clinical practice and has largely been replaced by modern venous duplex scanning.
Auscultation involves placing the bell of the stethoscope over the identified varicosity and then listening for a bruit. A bruit indicates turbulent blood flow which may suggest an underlying arteriovenous malformation.
Other special tests
Handheld Doppler and venous duplex scanning
Please note that in modern practice all patients under consideration of varicose vein treatment will undergo a venous duplex scan of the entire superficial venous system to:
- Confirm the origin of the incompetence (e.g. SFJ, SPJ).
- Assess whether the veins are suitable for endovenous treatment (radiofrequency or laser ablation) as veins need to relatively straight to permit the passage of the catheters.
- Establish the function of the deep venous system – if the deep veins are incompetent the patient may be relying on the superficial venous system for the return of venous blood thus treating the superficial veins may cause chronic limb swelling.
You should be aware of traditional tests that were performed routinely before the advent of venous duplex scanning, but note they are rarely performed in modern practice.
The most common special test would be the use of a handheld Doppler. As a vascular surgeon, I would be far more interested in whether a candidate could assess the competence of the SFJ with a handheld doppler than perform any of the other outdated old fashioned special tests.
Trendelenburg test (tourniquet test)
This test is used to locate the site of the incompetent venous valves. If using fingers, it is called the Trendelenburg test, if using a tourniquet instead it’s called the tourniquet test.
One leg should be assessed at a time.
1. Position the patient lying flat on the examination couch.
2. Lift the patient’s leg up (as far as the patient is comfortable with) and empty the superficial veins by milking the leg towards the groin (SFJ).
3. Place a tourniquet over the saphenofemoral junction (SFJ) – this is found approximately 2-3cm below and lateral to the pubic tubercle.
4. Ask the patient to stand and observe for filling of the veins:
- At this point, if the veins have not filled and remain collapsed, it indicates the incompetent venous valve(s) was/were at the level of the SFJ.
- If the veins have filled up again, it indicates the incompetent valve(s) is/are inferior to the SFJ (i.e. perforator veins – veins that drain venous blood from superficial to deep veins within the muscle).
5. Repeat the test with the patient lying down, placing the tourniquet 3cm lower than the previous position. Ask the patient to stand and observe venous filling once again.
6. Repeat this sequence until filling stops and the location of the incompetent venous valves is localised.
Cough impulse test
1. Place your hand over the saphenofemoral junction (2-3cm below and lateral to the pubic tubercle) and ask the patient to cough.
2. If you feel an impulse over the SFJ this indicates a saphena varix (dilatation of the saphenous vein at the SFJ).
Perthe’s test
Perthe’s test is used to distinguish between venous valvular insufficiency in the deep, perforator and superficial venous systems.
1. Apply a tourniquet at the proximal mid-thigh level whilst the patient is standing.
2. Ask the patient to walk around the room (or continually alternate between standing on tip-toes and flat feet) for 5 minutes.
Interpretation
If the varicose veins become less distended, it suggests that there is no deep venous valvular insufficiency, because the calf muscle is able to empty the varicose veins by pumping blood from the superficial venous system to the deep venous system. This result would suggest there is a primary problem with the superficial veins.
If the varicose veins remain distended (or become more distended) it suggests there is also a problem with the deep venous system, preventing the drainage of blood from the superficial varicose veins. In this circumstance, the patient may also experience pain in the leg due to venous hypertension. A potential cause of deep venous obstruction is a deep vein thrombosis.
To complete the examination…
Explain to the patient that the examination is now finished.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Example summary
“Today I examined Mr Smith, a 64-year-old male. On general inspection, the patient appeared comfortable at rest and there were no objects or medical equipment around the bed of relevance.”
“Venous eczema was noted over the distal portion of both lower limbs and a 3 x 3cm shallow ulcer was noted over the medial aspect of the left ankle. There were also several visible varicose veins noted in both legs with no evidence of phlebitis. Pulses were normal throughout in both lower limbs.”
“In summary, these findings are consistent with peripheral venous disease.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
Suggest further assessments and investigations to the examiner:
- Doppler ultrasound: to enable further bedside assessment of incompetent venous valves and the identification of thrombosis.
- Venous duplex scanning: for a comprehensive assessment of lower limb venous drainage.
- Ankle-brachial pressure index (ABPI) measurement: to assess arterial perfusion.
- Peripheral arterial examination: to assess for evidence of arterial disease.
- Abdominal examination: occasionally increased pressure in the abdomen or pelvis (e.g. a large tumour) can occlude venous return from the legs leading to venous hypertension and varicose veins.
Reviewer
Mr Craig Nesbitt (MD, FRCS, MBChB Hons)
Vascular and Endovascular Consultant
References
- James Heilman, MD. Adapted by Geeky Medics. Haemosiderin staining. Licence: [CC BY-SA].
- Prof. Gerd Hoffmann. Adapted by Geeky Medics. Venous eczema. Licence: [CC BY-SA 3.0 de].
- Milorad Dimić M.D. Adapted by Geeky Medics. Venous ulcer. Licence: [CC BY 3.0].
- Jonathan Moore. Adapted by Geeky Medics. Arterial ulcer. Licence: CC BY 3.0.
- Thomas Kriese. Adapted by Geeky Medics. Varicose veins. Licence: [CC BY 2.0].
- Nini00. Adapted by Geeky Medics. Licence: [CC BY-SA 3.0].