- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Conjunctivitis refers to inflammation of the conjunctiva, the external layer covering the outer surface of the globe and the inner surface of the eyelids.1 It is an extremely common condition and accounts for more than 1% of GP consultations in the UK.
Symptoms can include a red-eye, chemosis (swelling of the conjunctiva) and epiphora (watering eyes), which is associated with discharge.2
The diagnosis of conjunctivitis is usually clinical but further investigations may be required to rule out other causes of a red eye (e.g. acute angle-closure glaucoma or scleritis).
Conjunctivitis can be classified into infectious and non-infectious conjunctivitis.2
This article will cover the different types of conjunctivitis and how to distinguish them in clinical practice. For more information on other causes of red-eye, see the Geeky Medics guides to painless red-eye and painful red-eye.
Infectious conjunctivitis
Various micro-organisms can cause infectious conjunctivitis. The most common causes of infectious conjunctivitis are viruses and bacteria, though fungi can rarely be causative organisms.
Viral conjunctivitis
Aetiology
Most cases of viral conjunctivitis are caused by adenovirus, with herpes viruses also contributing to a smaller proportion.2
Other less frequent causes include measles, mumps and rubella, though these have decreased due to vaccination. Enterovirus and coxsackievirus can cause a rare type of viral conjunctivitis, known as acute haemorrhagic viral conjunctivitis.3
Risk factors
Viral conjunctivitis is extremely infectious and therefore, direct contact with contaminated skin or objects can lead to the spreading of infection.2
Clinical features
Viral conjunctivitis tends to affect both eyes and presents with profuse watery discharge (Figure 1) and occasionally, tender preauricular lymphadenopathy. It is often associated with a concurrent upper respiratory tract infection.1
Adenoviral conjunctivitis can cause two presentations in a patient, depending on its serotype:3
- Pharyngoconjunctival fever: as the name suggests, patients present with pharyngitis, conjunctivitis and fever (serotypes 3, 4 and 7).
- Epidemic keratoconjunctivitis: more severe, associated with corneal involvement and photophobia (serotypes 8, 19 and 37).

Investigations
Investigations are rarely required as the diagnosis of viral conjunctivitis can be made from the history and examination of the patient.
In unusual or treatment-resistant cases, swabs may be taken to aid with diagnosis.3
Management
Viral conjunctivitis tends to be self-limiting and rarely requires treatment. It is important to adopt simple hygiene measures to prevent spread (e.g. washing hands regularly and avoiding sharing linen).4
Complications
Viral conjunctivitis is unlikely to cause any complications and the prognosis for patients is excellent.
Key points
- Viral conjunctivitis is a common presentation that usually affects both eyes with profuse watery discharge
- The main cause is adenovirus, which typically causes a concomitant upper respiratory tract infection
- Management of adenovirus conjunctivitis is supportive though it is important to advise on hygiene measures to stop the spread of infection
Bacterial conjunctivitis
Aetiology
Causative organisms of bacterial conjunctivitis include Staphylococcus, Streptococcus and Haemophilus.6
Other important causes include Chlamydia trachomatis, with serotypes D-K being responsible for conjunctivitis. In neonates, Neisseria gonorrhoea can cause a particularly exudative form of conjunctivitis (ophthalmia neonatorum), because of infection from the mother’s birth canal.6
Both bacteria are also causes of reactive arthritis, which classically presents as a triad of arthritis, conjunctivitis and urethritis.7
Risk factors
Like viral conjunctivitis, one of the main risk factors is contact with contaminated skin and objects. In cases of chlamydia or gonorrhoea, unprotected sexual intercourse amongst young people is a key risk factor.2
Clinical features
Bacterial conjunctivitis tends to affect only one eye but can be bilateral in the minority of cases.6 It tends to develop quite rapidly with very inflamed conjunctiva and a sticky purulent discharge (Figure 2).
Gonococcal infections are associated with a very profuse discharge. Due to the discharge, patients with bacterial conjunctivitis will often state that their eyelids stick together on waking.2,6
Unlike other bacteria, chlamydial conjunctivitis tends to be associated with follicles and pre-auricular lymphadenopathy.

Investigations
Bacterial conjunctivitis can be diagnosed without investigations. Conjunctival scrapes are occasionally used in patients with a high risk of atypical organisms, for example, immunosuppressed, post-corneal transplant and sexually active young people.
Management
For most cases of bacterial conjunctivitis, the treatment is supportive and antibiotic drops (e.g. chloramphenicol) are used rarely. In cases secondary to chlamydia or gonorrhoea, treatment is usually systemic antibiotics such as azithromycin.6
Complications
Unlike viral conjunctivitis, bacterial conjunctivitis carries a higher risk of complications. Certain bacteria such as Neisseria have a propensity to invade the cornea, which can lead to keratitis and endophthalmitis.2 These conditions can subsequently cause reduced vision or blindness if not treated promptly.
Key points
- Bacterial conjunctivitis tends to be unilateral and develop rapidly
- Though a large majority of cases are self-limiting, involvement of certain bacteria can lead to severe complications
- Management of bacterial conjunctivitis is supportive with antibiotics being reserved for severe or atypical cases
Non-infectious conjunctivitis
Non-infectious causes of conjunctivitis include allergy, chemicals and irritants.
Allergic conjunctivitis
Aetiology
Allergic conjunctivitis is the most common cause of non-infectious conjunctivitis and occurs secondary to a type I hypersensitivity reaction to a particular trigger.9
Risk factors
A personal or family history of atopic conditions, such as asthma and hay fever, increases the risk of allergic conjunctivitis.2
Clinical features
The distinguishing feature of allergic conjunctivitis is the presence of itching. As it is driven by a systemic process, both eyes are usually affected with diffuse redness and watery discharge.2
Examination of the eyelid will reveal papillae, which if large can give a ‘cobblestone’ appearance (Figure 3).
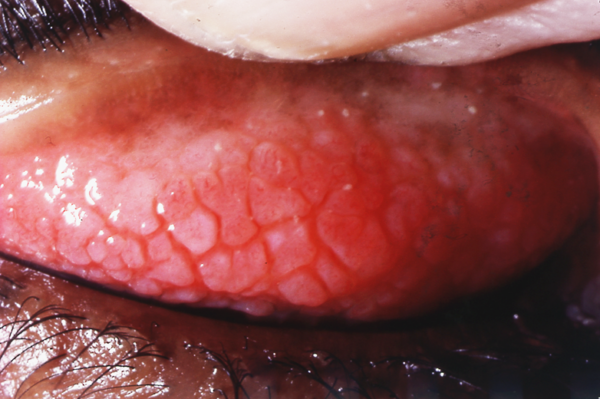
There are multiple subtypes of allergic conjunctivitis:2,10
- Seasonal allergic conjunctivitis: secondary to hay fever, therefore most common in summer months due to the presence of pollen
- Perennial allergic conjunctivitis: caused by allergens such as house dust mite
- Vernal keratoconjunctivitis: most common in young males living in hot dry climates
- Atopic keratoconjunctivitis: most common in middle-aged men
Investigations
A history of atopy or recurring conjunctivitis in response to a trigger or changes to the weather is strongly suggestive of allergy conjunctivitis.
Conjunctival scrapes may be performed and will reveal the presence of eosinophils, typical of a type I hypersensitivity reaction.9
Management
Treatment includes allergen avoidance, topical and oral antihistamine as well as topical mast-cell stabilisers and occasionally, mild steroids.10
Complications
Allergic conjunctivitis does not result in complications. However, the use of steroids in managing flares can increase the risk of herpes infection, glaucoma and cataracts.
Key points
- Allergic conjunctivitis is a common condition with a predominating feature being itching
- Individuals affected by allergic conjunctivitis tend to have strong histories of atopy
- The mainstay of management includes allergen avoidance and antihistamines for symptomatic relief
Chemical and irritant conjunctivitis
Chemical eye injury can also result in conjunctivitis and if severe, inflammation of deeper structures. Alkaline burns tend to cause more significant damage as compounds are lipophilic and cause the saponification of fatty acids. This allows the agent to penetrate structures easily.
In contrast, acids denature and precipitate proteins in the cornea, which in turn forms a barrier and prevents further penetration of the acid.12
Chemical eye injury is an ophthalmic emergency and requires urgent irrigation of the eye to limit the damage.1,12
Irritants such as smoke, dust, fumes and even chlorine in swimming pools can also cause conjunctivitis.1,4
Summary table
Table 1. Summary of the clinical features of conjunctivitis.
|
|
Bacterial | Viral | Allergic | Chlamydial |
|
Laterality |
Unilateral |
Bilateral |
Bilateral |
|
|
Discharge |
Mucopurulent |
Watery |
Watery |
Mucopurulent |
|
Preauricular lymphadenopathy |
No |
Yes |
No |
Occasionally |
|
Lid findings |
Papillae |
Follicles |
Papillae |
Follicle |
Reviewer
Consultant Ophthalmologist
Editor
Dr Chris Jefferies
References
- American Optometric Association. Available from: [LINK]
- EyeWiki. Conjunctivitis. Updated in 2021. Available from: [LINK]
- MSD Manuals. Viral Conjunctivitis. Updated in April 2021. Available from: [LINK]
- MSD Manuals. Overview of Conjunctivitis. Updated in April 2021. Available from: [LINK]
- Marco Mayer. Keratoconjunctivitis epidemica 2. License: [CC BY-SA 4.0]. Available from: [LINK]
- MSD Manuals. Acute Bacterial Conjunctivitis. Updated in April 2021. Available from: [LINK]
- American College of Rheumatology. Reactive Arthritis. Updated in December 2021. Available from: [LINK]
- Tanalai at English Wikipedia. Swollen eye with conjunctivitis. License: [CC BY 3.0]. Available from: [LINK]
- MSD Manuals. Allergic Conjunctivitis. Updated in April 2021. Available from [LINK]
- EyeWiki. Allergic Conjunctivitis. Updated in 2022. Available from: [LINK]
- John D C Anderson. Papillae of vernal conjunctivitis in an 18 year old Afgan male. License: [CC BY-NC 2.0]. Available from: [LINK]
- Singh, P et al. Ocular chemical injuries and their management. Oman J Ophthalmol. 2013; 6(2): 83-86