- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The leg is defined anatomically as the portion of the lower limb from the knee joint to the ankle joint.
The muscles of the leg are divided into three compartments: the anterior compartment, the posterior compartment and the lateral compartment. In total, there are 13 separate muscles across these three compartments.
The muscles in the anterior compartment act to dorsiflex and invert the foot, as well as extend the toes. Muscles in the posterior compartment plantarflex the foot, flex the toes and invert the foot. Lateral compartment muscles of the leg act to evert the foot.
Posterior compartment
The muscles in the posterior compartment are arranged into two groups: the superficial group and the deep group.
These two groups are divided by a layer of deep fascia called the transverse intermuscular septum.
As a group these muscles act to plantarflex and invert the foot, as well as flexing the toes. All muscles within the posterior compartment are innervated by the tibial nerve.
Superficial group
The three muscles of the superficial group are gastrocnemius, soleus and plantaris.
The large size of gastrocnemius and soleus form the typical ‘calf’ shape, which is a human trait due to our upright nature. These strong powerful muscles are able to propel the body forward when moving and elevate it upwards on to the toes.
All three of the superficial muscles insert into the calcaneus (heel) via the calcaneal tendon, the most powerful tendon in the body.
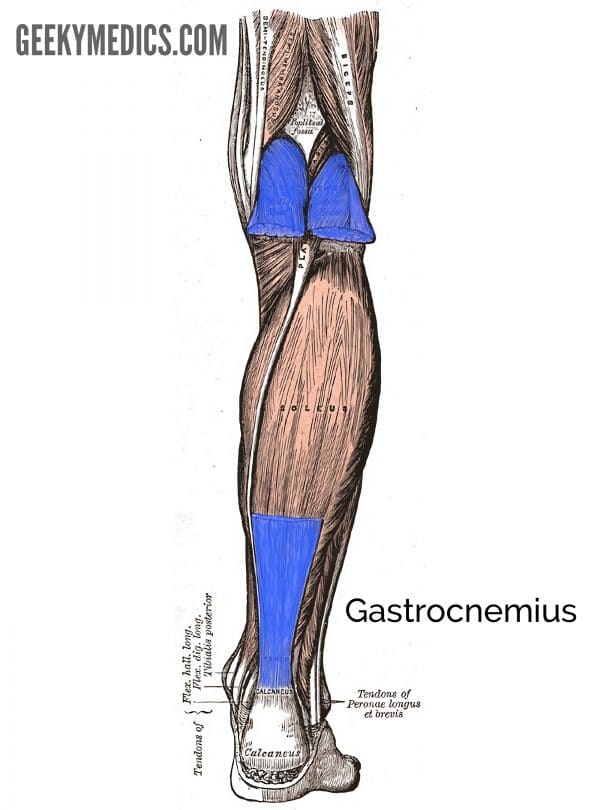
Gastrocnemius
Gastrocnemius is the most superficial muscle within the posterior compartment and originates from its two heads, the medial and lateral head.
These heads form the borders of the lower section of the popliteal fossa, an important anatomical landmark for neurovascular structures. The heads of gastrocnemius combine to form the muscle belly of the characteristic calf shape and distally contribute to the formation of the calcaneal tendon.
The word gastrocnemius has Greek and Latin origin which translates as ‘stomach of the leg’.
Origin:
- Medial head: medial femoral condyle
- Lateral head: lateral femoral condyle
Insertion: posterior surface of the calcaneus (via calcaneal tendon)
Action: plantarflexes foot and flexes knee
Innervation: tibial nerve
Blood supply: sural arteries (branches from the popliteal artery)
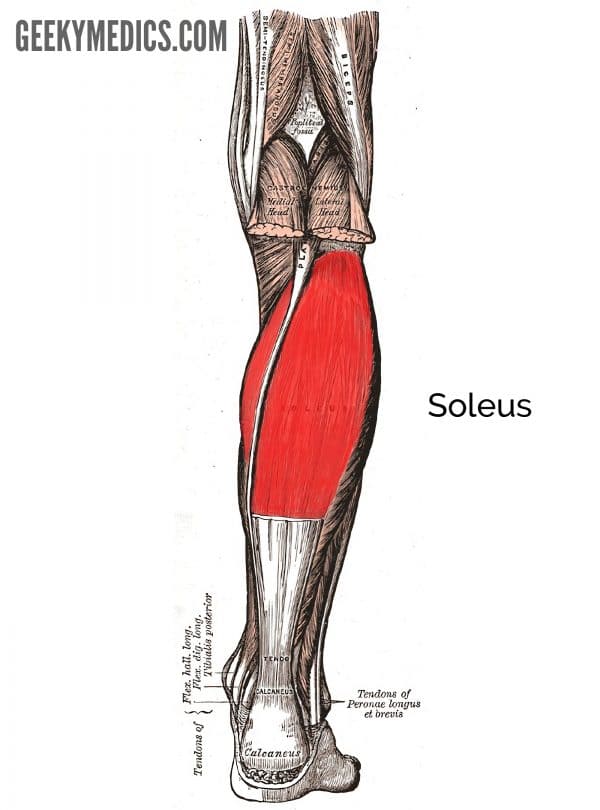
Soleus
Soleus is a large flat muscle located underneath gastrocnemius that received its name for its resemblance to a Sole, a type of flatfish.
Soleus has three origin points, one of which being the tendinous arch of soleus which spans between the tibia and fibula. This tendinous arch is where the popliteal artery exits the popliteal fossa to enter the deep region of the posterior compartment of the leg, immediately dividing into the anterior tibial and posterior tibial arteries.
Origin: soleal line and medial border of tibia; posterior fibular head; and tendinous arch between tibial and fibular attachments
Insertion: posterior surface of the calcaneus (via calcaneal tendon)
Action: plantarflexes foot
Innervation: tibial nerve
Blood supply: posterior tibial, fibular and sural arteries (branches from the popliteal artery)
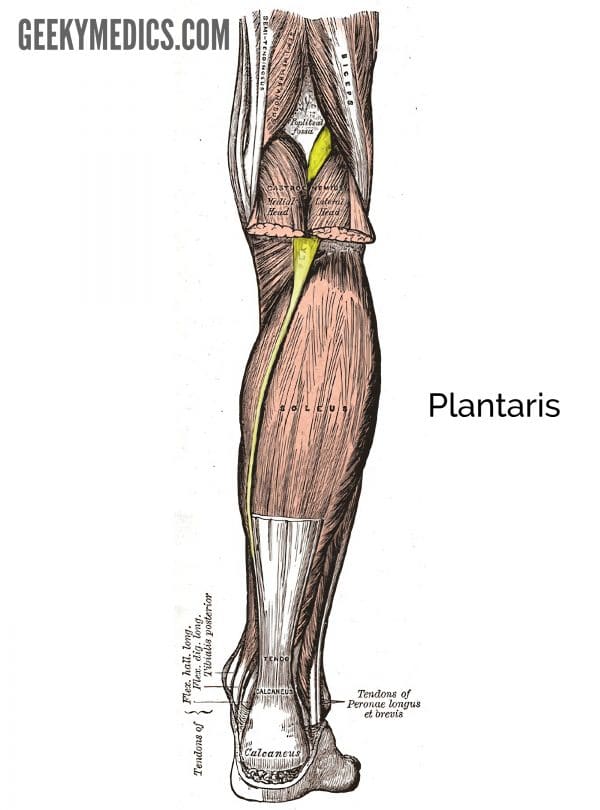
Plantaris
Plantaris is a small muscle with a short belly and a long tendon which joins the calcaneal tendon distally. Its involvement in foot plantarflexion or knee flexion is insignificant and as a result, the plantaris tendon can be removed for grafting (e.g. to perform a tendon repair in hand surgery) without causing disability.
The muscle is also absent in approximately 10% of people.
Origin: inferior part of the lateral supracondylar line of femur and oblique popliteal ligament of knee
Insertion: posterior surface of the calcaneus (via calcaneal tendon)
Action: plantarflexes foot and flexes knee
Innervation: tibial nerve
Blood supply: sural arteries (branches from the popliteal artery)
Deep group
There are four muscles which make up the deep group of the posterior compartment: popliteus, flexor digitorum longus, flexor hallucis longus and posterior tibialis. Popliteus is the only muscle to act on the knee whereas the others act on the foot and toes.
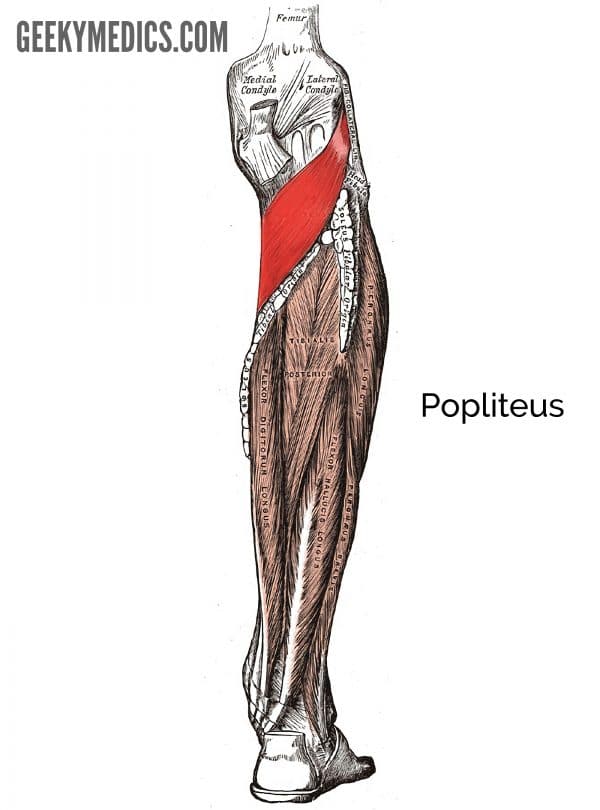
Popliteus
Popliteus is a flat triangular-shaped muscle that forms part of the floor of the popliteal fossa. The main function of popliteus is to unlock the knee. It does this by rotating the femur laterally 5o to release the knee from its locked position allowing flexion to occur.
Origin: lateral femoral condyle and lateral meniscus
Insertion: posterior surface of the proximal tibia
Action: unlocks the knee joint by laterally rotating the femur on the fixed tibia as well as stabilising the knee joint
Innervation: tibial nerve
Blood supply: genicular branches from the popliteal artery
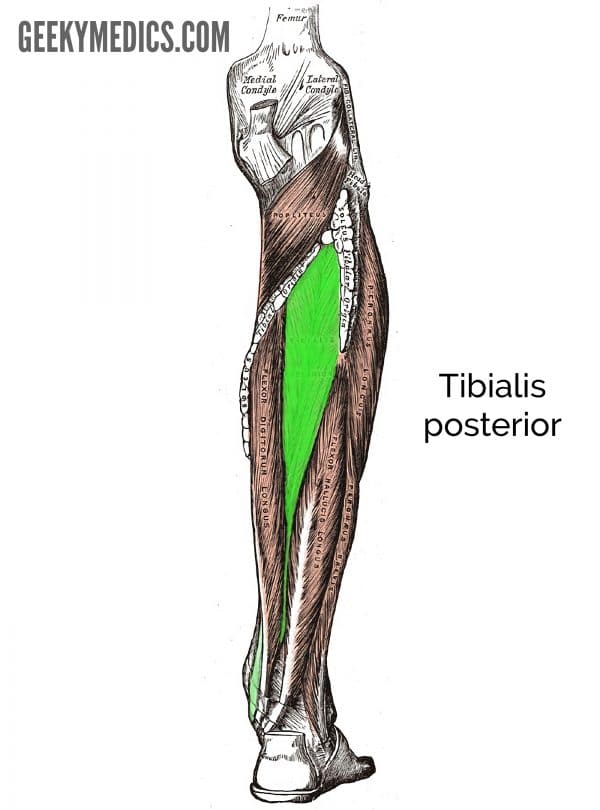
Tibialis posterior
Located between flexor digitorum longus and flexor hallucis longus, tibialis posterior is the deepest muscle in the posterior compartment. Whilst this muscle is involved with inversion and plantarflexion of the foot, its main function is to support the medial arch of the foot.
To test tibialis posterior, invert the foot against resistance in slight plantarflexion. If normal, the tendon should be visible and can be palpated posterior to the medial malleolus.
Origin: interosseous membrane and posterior surfaces of the tibia and fibula
Insertion: tuberosity of navicular and adjacent region of the medial cuneiform
Action: inversion and plantarflexion of the foot. Supports the medial arch of the foot during walking.
Innervation: tibial nerve
Blood supply: posterior tibial artery
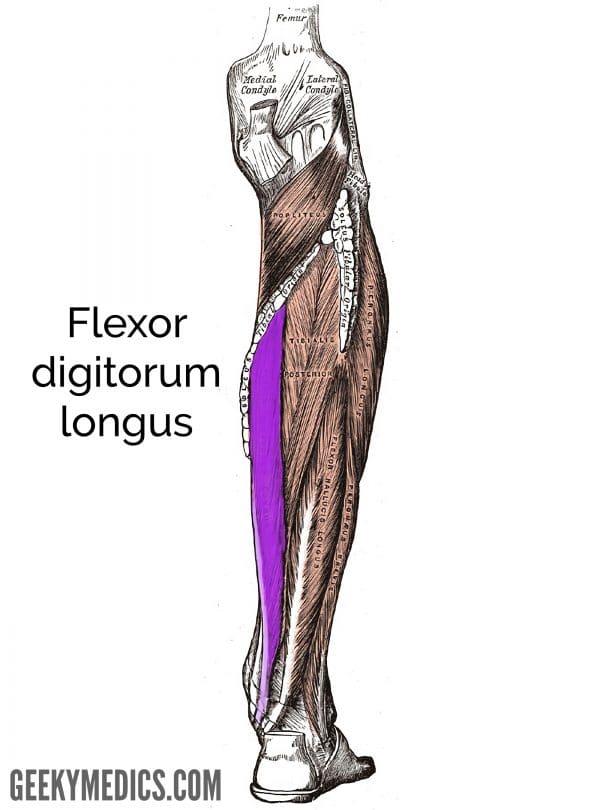
Flexor digitorum longus
Flexor digitorum longus begins on the medial side of the posterior compartment and descends down the leg where its tendon enters the sole of foot to insert on the distal phalanges of the lateral four toes. The muscle is involved with gripping the ground during walking by flexing the lateral four toes.
Origin: medial side of the posterior surface of the tibia
Insertion: bases of distal phalanges of lateral four toes
Action: flexes lateral four toes
Innervation: tibial nerve
Blood supply: posterior tibial artery
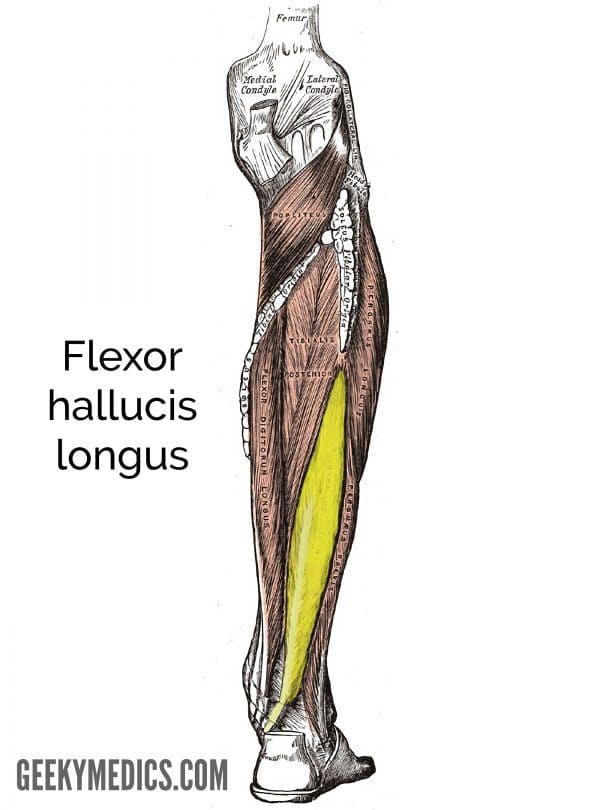
Flexor hallucis longus
Flexor hallucis longus’ main role is to flex the great toe. It originates on the lateral side of the posterior compartment and its tendon curves under the talus bone in the foot to insert into the distal phalanx of the great toe.
Origin: posterior surface of the fibula and interosseous membrane
Insertion: base of distal phalanx of the great toe
Action: flexes the great toe
Innervation: tibial nerve
Blood supply: posterior tibial and fibular artery
Clinical relevance: Ruptured Achilles tendon
A ruptured Achilles tendon typically occurs during a forceful ‘push off’ motion when the foot is in plantarflexion and is sometimes accompanied by an audible snap. There is immediate pain in the calf and sudden dorsiflexion of the previously plantarflexed foot. Due to shortening of gastrocnemius and soleus a lump can be felt in the calf and in a completely ruptured tendon, a gap may be palpable just proximal to the calcaneal attachment. A history of calcaneal tendonitis and use of quinolone antibiotics (e.g. ciprofloxacin) can predispose the tendon to rupture.
Simmond’s test is a useful method of testing for Achilles tendon rupture. The patient lies prone on the examination couch with their feet hanging over the edge and the examiner squeezes the calf muscles and whilst observing for plantarflexion of the foot. The absence of plantarflexion (a normal response) is indicative of Achilles tendon rupture.
Depending on the patient, treatment can be surgical or non-surgical. In older or non-athletic people, non-surgical management is often adequate but those with an active lifestyle may require surgical intervention.
Lateral compartment
There are only two muscles in the lateral compartment of the leg: fibularis longus and fibularis brevis. You may also see these muscles referred to as peroneal longus and peroneal brevis.
The word peroneal means “relating to the outer side of the leg” and is used interchangeably with fibular or fibularis. The same occurs for the common fibular nerve or common peroneal nerve. Both muscles evert the foot and are innervated by a branch of the common fibular nerve, the superficial fibular nerve.
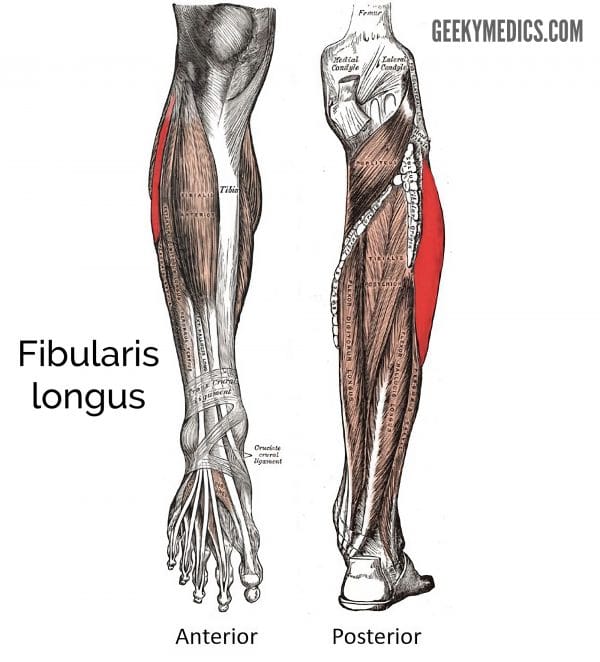
Fibularis longus
Fibularis longus is the longer and more superficial of the two muscles in the lateral compartment, originating from the upper lateral surface and head of the fibula. Its tendon passes posterior to the lateral malleolus and enters the lateral side of the foot crossing under the sole of the foot, attaching to the medial side of the cuneiform and base of the first metatarsal. Together with tibialis anterior and tibialis posterior, they act as a stirrup to support the arches of the foot.
Origin: the head and upper lateral surface of the fibula
Insertion: distal end of medial cuneiform and base of the first metatarsal
Action: eversion and plantarflexion of the foot. Provides support to the lateral and transverse arches of the foot.
Innervation: superficial fibular nerve (a branch of the common fibular nerve)
Blood supply: fibular artery
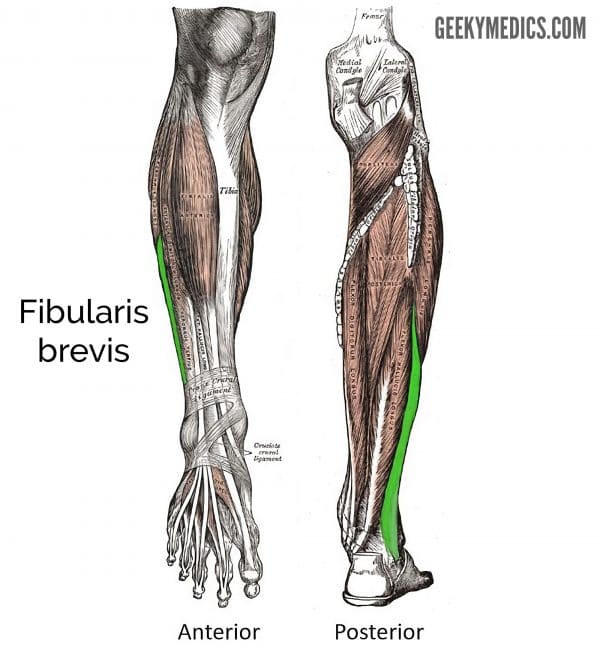
Fibularis brevis
Brevis is the Latin word for ‘short’ and as its name suggests, fibularis brevis is the shorter muscle in the lateral compartment. It lies deep to fibularis longus and originates from the lower two-thirds of the lateral surface of the fibular shaft. Its tendon passes behind the lateral malleolus with the fibularis longus tendon to insert on to a tubercle at the base of the fifth metatarsal.
Origin: lateral surface of the shaft of the fibula
Insertion: lateral tubercle at the base of the fifth metatarsal
Action: eversion of the foot
Innervation: superficial fibular nerve (a branch of the common fibular nerve)
Blood supply: fibular artery
Anterior compartment
In the anterior compartment of the leg, there are four muscles: tibialis anterior, extensor hallucis longus, extensor digitorum longus and fibularis tertius.
Some texts may consider extensor digitorum longus and fibularis tertius to be the same muscle and therefore only refer to three muscles in the anterior compartment. However, in this article, we are classing them as separate muscles.
Together the muscles in this compartment act to dorsiflex and invert the foot, and extend the toes. All are innervated by the deep fibular nerve, a branch of the common fibular nerve.
Clinical relevance: Compartment syndrome
Compartment syndrome is a condition in which increased pressure within one of the body’s anatomical compartments results in insufficient blood supply to tissue within that space.
Compartment syndrome often occurs due to muscle swelling. The swelling muscle is confined in a fixed volume compartment and this causes an increase in pressure within the compartment.
Over time the pressure in the compartment surpasses the arterial pressure, resulting in loss of arterial blood supply and secondary tissue ischaemia. Compartment syndrome can be acute or chronic, but it is most commonly due to trauma such as a bone fracture or crush injury.
If left untreated, compartment syndrome will cause irreversible tissue ischaemia which can result in long term muscles contractures (known as Volkmann’s ischaemic contracture) or even the need for amputation.
Typical clinical features of compartment syndrome include:
- Pain (progressive and disproportionate to the original injury/clinical findings)
- Paraesthesia (reduced sensation)
- Paralysis
- Pallor
- Pulselessness
Pain and paraesthesia are early symptoms and should prompt initiation of treatment. If there are reduced or absent pulses, then this suggests severe ischaemic damage.
Immediate treatment involves removing constrictive dressings and raising the limb above the level of the heart. Fasciotomy of the muscle compartments releases pressure and should be performed as soon as possible to minimise the risk of irreversible ischaemia.
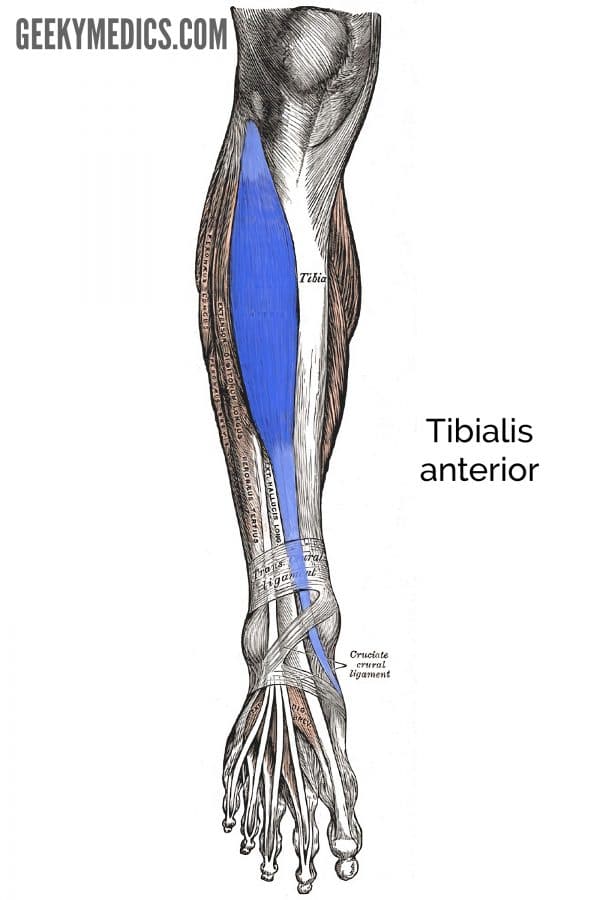
Tibialis anterior
Tibialis anterior (TA) is the most superficial and medial muscle in the anterior compartment of the leg. It is the most powerful dorsiflexor of the foot and during walking provides support for the medial arch of the foot. The function of TA can be assessed by asking a patient to dorsiflex their foot against resistance or stand on their heels. The tendon of a healthy TA should be clearly visible during these movements.
Origin: lateral surface of the tibia and adjacent interosseous membrane
Insertion: medial cuneiform and base of the first metatarsal
Action: dorsiflexion and inversion of the foot as well as supporting the medial arch of the foot
Innervation: deep fibular nerve (a terminal branch of the common fibular nerve)
Blood supply: anterior tibial artery
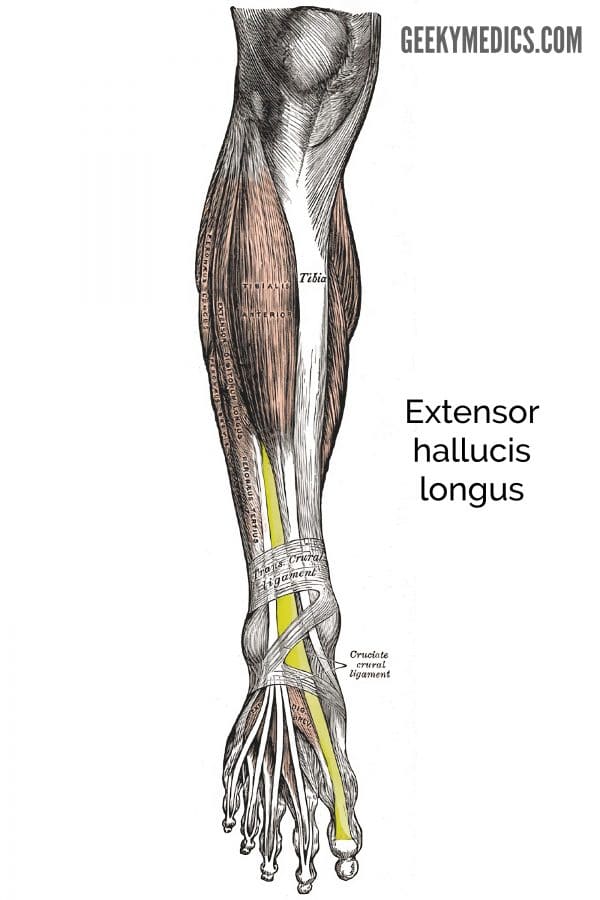
Extensor hallucis longus
Extensor hallucis longus (EHL) is located deeply between tibialis anterior and extensor digitorum longus. It begins at the middle of half of the fibula and interosseous membrane travelling down anteriorly to insert at the distal phalanx of the great toe.
Origin: medial surface of fibula and adjacent surface of the interosseous membrane
Insertion: base of distal phalanx of the great toe
Action: extension of the great toe and dorsiflexion foot
Innervation: deep fibular nerve (a terminal branch of the common fibular nerve)
Blood supply: anterior tibial artery
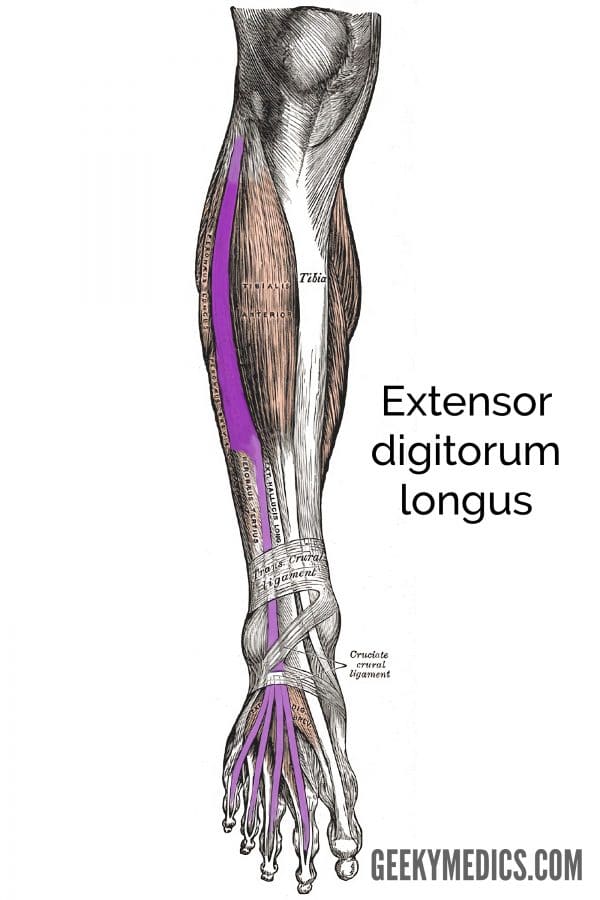
Extensor digitorum longus
The most lateral of the muscles in the anterior compartment, extensor digitorum longus (EDL) originates mainly from the medial surface of the fibula but also from the lateral tibial condyle. The muscle forms its tendon in the lower third of the leg which then later divides into four tendons inserting into the lateral four toes.
Origin: lateral condyle of the tibia and medial surface of the fibula
Insertion: middle and distal phalanges of the lateral four toes
Action: extension of the lateral four toes and dorsiflexion of the foot
Innervation: deep fibular nerve (a terminal branch of the common fibular nerve)
Blood supply: anterior tibial artery
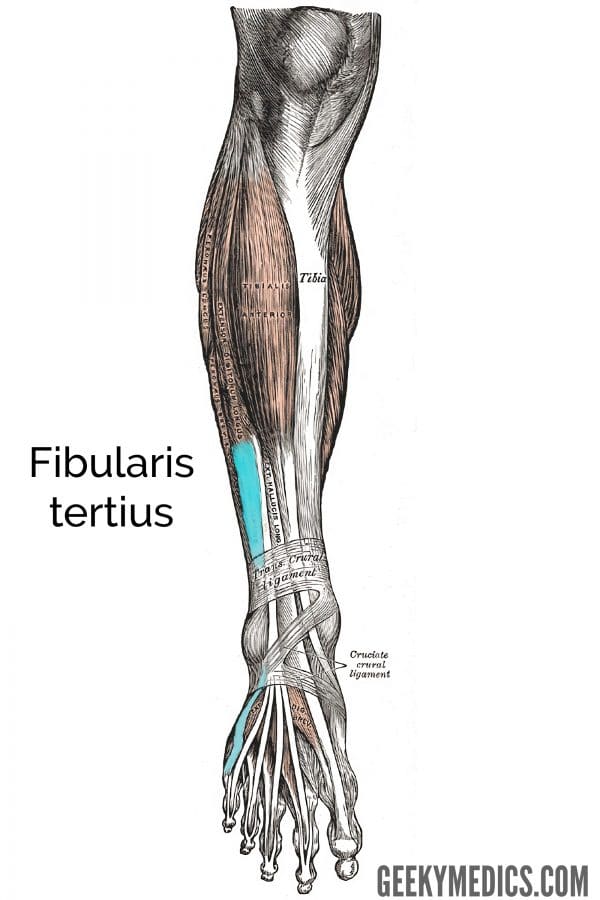
Fibularis tertius
Proximally fibularis tertius (FT) is continuous with EDL and as a result, some texts consider it to be part of the EDL rather than a muscle in its own right. However, distally the tendon of FT is separate from EDL and inserts into the fifth metatarsal as shown in the diagram of the lateral foot below. FT is not always present in all humans.
Origin: medial surface of the fibula
Insertion: the fifth metatarsal
Action: dorsiflexion and eversion of the foot
Innervation: deep fibular nerve (a terminal branch of the common fibular nerve)
Blood supply: anterior tibial artery
Clinical relevance: Injury to the common fibular nerve and foot drop
Foot drop occurs as a result of injury to the common fibular nerve. The common fibular nerve is susceptible to injury because of its superficial location when it passes around the neck of the fibula.
Potential mechanisms of injury include direct trauma, secondary to a knee injury such as a dislocation, or as a result of a proximal fibular fracture.
Damage to the common fibular nerve results in paralysis of all muscles in the anterior and lateral compartments of the leg (the muscles which dorsiflex and evert the foot). Consequently, an inability to dorsiflex the foot results in foot drop.
Patients with foot drop have a characteristic ‘high-stepping’ gait where the foot is lifted abnormally high to avoid dragging the foot across the floor. People with injury to the common fibular nerve may also experience loss of sensation on the anterolateral aspect of the leg and dorsum of the foot.
Key points
- Muscles in the posterior compartment act to plantarflex and invert the foot as well as flexing the toes. All muscles in the posterior compartment are innervated by the tibial nerve.
- Muscles in the lateral compartment act to evert the foot and are innervated by the superficial fibular nerve.
- Muscles in the anterior compartment act to dorsiflex and invert the foot, and extend the toes. The muscles in the anterior compartment are innervated by the deep fibular nerve.
- Injury to the common fibular nerve is one of the most common causes of foot drop.
Editor
Dr Chris Jefferies
References
- Richard L. Drake, A. Wayne Vogyl, Adam W.M. Mitchell. Gray’s Anatomy for Students 4th Elsevier, 2020.
- Keith L. Moore, Arthur F. Dalley, Anne M. R. Agur. Moore Clinically Orientated Anatomy 7th Lippincott Williams & Wilkins, 2013.




