- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Learning to differentiate between shockable and non-shockable rhythms is a key skill in managing a cardiac arrest as it informs which part of the advanced life support (ALS) algorithm to follow.
In this article, we will look at the characteristic features of the four cardiac arrest rhythms as they appear on a defibrillator rhythm strip.
Shockable rhythms
The two shockable rhythms in cardiac arrest are pulseless ventricular tachycardia (pVT) and ventricular fibrillation (VF).
Shockable rhythms are associated with the best prognosis in cardiac arrest. High-quality CPR and prompt defibrillation are key to improving survival rates.
Ischaemic heart disease and acute coronary syndromes are the most common causes of VF and pVT arrests.
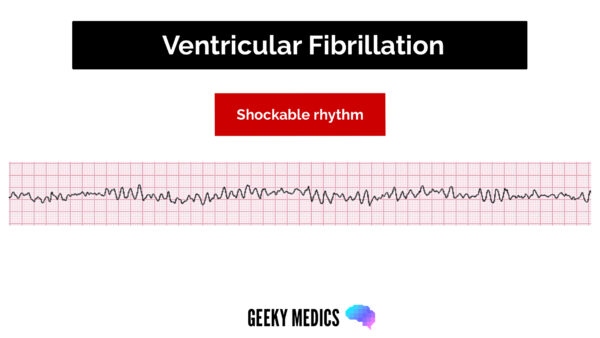
Ventricular fibrillation
Ventricular fibrillation appears on a rhythm strip as chaotic and disorganised electrical activity with no identifiable QRS complexes. VF is initially coarse and will progress to fine VF and eventually asystole if prompt defibrillation is not performed.
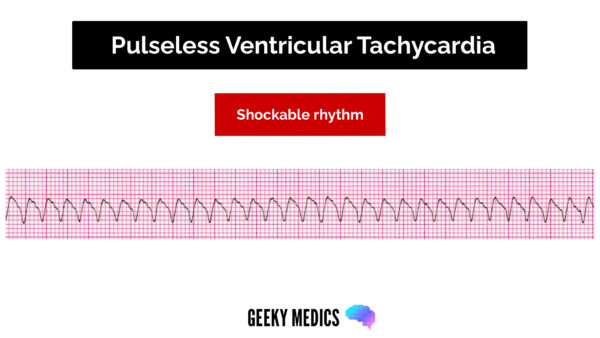
Ventricular tachycardia
Ventricular tachycardia appears on a rhythm strip as a regular broad complex tachycardia, typically between 100-300 bpm.
It is important to check for a pulse when this rhythm is seen. VT with a pulse is managed according to the ALS tachycardia algorithm.
VT can be monomorphic or polymorphic depending on the morphology of the QRS complexes. Torsade de pointes is a subtype of polymorphic VT where the axis of electrical activity rotates in a sinusoidal pattern. Torsade de pointes is associated with a long QT interval, and these patients often have low potassium and/or magnesium levels, which require replacement.
Non-shockable rhythms
The two non-shockable cardiac arrest rhythms are pulseless electrical activity (PEA) and asystole. These are associated with the worst prognosis in cardiac arrest.
High-quality CPR with minimal interruptions and administration of 1mg of IV/IO adrenaline (10ml of 1:10,000) as soon as access is obtained is key to improving survival rates.
Patients with PEA or asystole are unlikely to survive unless a reversible cause of cardiac arrest is identified and treated.
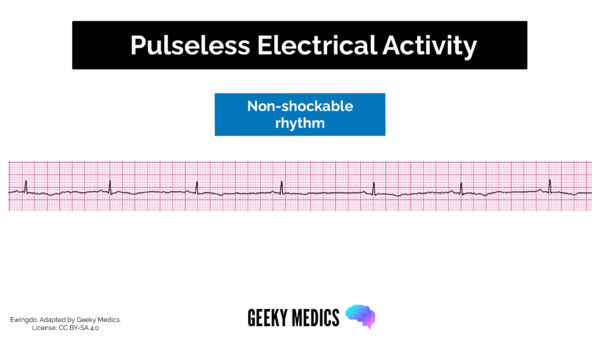
Pulseless electrical activity
Pulseless electrical activity is defined as the absence of a pulse in a patient with electrical activity that would normally be expected to produce a cardiac output (except VT).
Causes of PEA include severe fluid depletion or blood loss, cardiac tamponade, massive pulmonary embolism and tension pneumothorax.
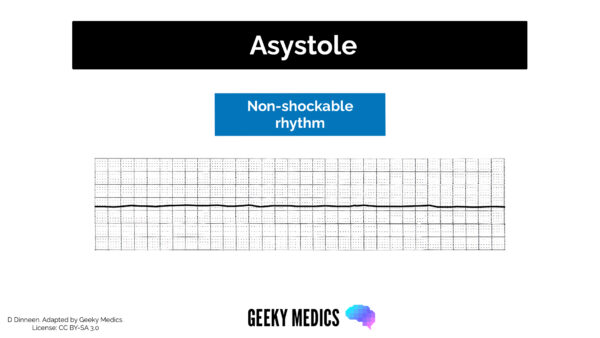
Asystole
Asystole describes the absence of electrical activity on the rhythm strip. This is rarely a completely flat line, as slight undulations are usually seen with additional interference from ventilation and chest compressions.
If a completely flat line is seen, ensure the monitoring is attached correctly.
Look out for regular P waves. Ventricular standstill with regular P waves may benefit from cardiac pacing.
Cardiac arrest rhythm recognition
One way of rapidly distinguishing between the different rhythms in cardiac arrest is to ask yourself a series of questions.
This method will not tease out complexities such as the difference between a VT and SVT with aberrancy (SVT with a bundle branch block pattern). However, it will help you rapidly determine which part of the ALS algorithm you should follow during cardiac arrest.
Is there a pulse?
No – cardiac arrest confirmed
Is there any electrical activity?
No – this is asystole
Is there coordinated electrical activity normally expected to produce a cardiac output (except VT)?
Yes – this is pulseless electrical activity (PEA)
Is there a regular broad complex tachycardia with recognisable QRS complexes?
Yes – this is consistent with ventricular tachycardia (VT)
Is there chaotic and disorganised electrical activity?
Yes – this is consistent with ventricular fibrillation (VF)
Top priorities in cardiac arrest management
- Prompt identification of cardiac arrest
- High quality CPR with minimal interruptions
- Early defibrillation in shockable rhythms (pVT and VF)
- Identify and treat any reversible causes of cardiac arrest (4Hs and 4Ts)
References
- Resuscitation Council (UK). Adult Advanced Life Support guidelines. Available from: [LINK]




