- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Thyroid eye disease (TED) is an autoimmune condition resulting in inflammation and swelling of the extraocular muscles, fatty tissue and connective tissue within the orbit.
It is the most common cause of unilateral and bilateral exophthalmos in adults and more common in females.1
Aetiology
TED commonly occurs in patients with Graves’ disease but can present in euthyroid or hypothyroid patients. In most patients, eye disease and thyroid issues evolve within 1.5 years of each other.
For more information on Graves’ disease, see the Geeky Medics guide to thyrotoxicosis and hyperthyroidism.
Pathophysiology
Closely correlating with Graves’ disease, patients with TED have been found to have elevated levels of antibodies against thyroid-stimulating hormone (TSH) receptors, which are expressed in orbital fat and connective tissue.
Studies also attribute increased fibroblast activity as well as the accumulation of collagen and hyaluronic acid to the enlargement and fibrosis of the extraocular muscles.2
Risk factors
Risk factors for thyroid eye disease include:
- Smoking
- Previous radioiodine therapy
- Men have more severe disease
Clinical features
History
Typical symptoms of thyroid eye disease include:
- Excessive watering
- ‘Gritty’ sensation
- Photophobia
- Eye pain
Other important symptoms to ask in the history include red eye, blurred vision (due to incomplete eyelid closure) and sensation of pressure.
Patients may also present with systemic signs of thyroid disease, such as pretibial myxoedema, goitre and acropachy.
Clinical examination
Typical clinical findings in thyroid eye disease include:
- Eyelid retraction (Dalrymple’s sign)
- Proptosis
- Lid lag (Von Graefe’s sign)
- Lid oedema
- Diplopia due to restriction of extraocular muscles, most commonly inferior rectus
- Incomplete eyelid closure
In a small portion of patients, the enlarged muscles and fat can press on the optic nerve, resulting in compressive optic neuropathy. Patients report reduced visual acuity, colour vision and contrast sensitivity. If this is not treated urgently, it can be sight-threatening.
While most patients have mild manifestations of TED, optic nerve compressing TED is one of the rare presentations in ophthalmology where urgent intravenous methylprednisolone is required. Hence, it is essential to check the measurement of proptosis and assess optic disc, visual acuity, colour vision and relative afferent pupillary defect at each assessment.3,4

Mnemonic: NO SPECS
The mnemonic ‘NO SPECS’ can be used to recall the features of thyroid eye disease.
- N: No signs or symptoms
- O: Only ocular irritation (dryness, gritty sensation)
- S: Soft tissue involvement (conjunctival oedema or injection)
- P: Proptosis
- E: Extraocular muscle involvement
- C: Corneal exposure and ulceration
- S: Sight loss (due to compressive optic neuropathy)
Investigations
Laboratory investigations
Relevant laboratory investigations include:3
- Thyroid function tests: raised T3 and/or T4 and low TSH levels in patients with hyperthyroidism
- Antibody testing: TSH-receptor antibodies, thyroid-stimulating antibody and TSH-binding inhibitory immunoglobulins and thyroid peroxidase antibodies – may be raised in patients with normal thyroid function tests
Imaging
Several imaging modalities can be used to confirm the diagnosis and exclude alternative diagnoses such as orbital tumour and high myopia (short-sightedness).4
Relevant imaging investigations include:
- Ultrasound scan: detects extraocular muscle enlargement
- CT orbits: useful to detect optic nerve involvement and image orbital bones for surgery planning
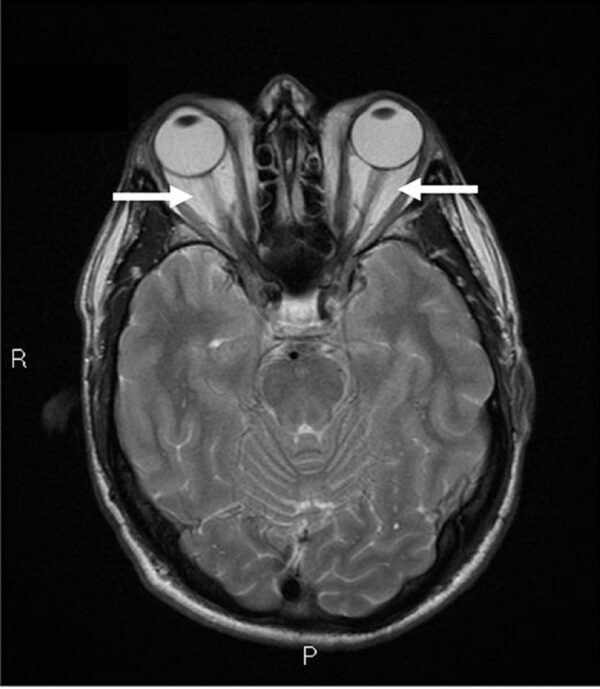
- MRI orbits: an alternative to CT scan with reduced ionisation risk (Figure 2)
Diagnosis
The diagnosis of thyroid eye disease is based on clinical signs, history and specialised tests. There are multiple classification systems for assessing severity, with the European Group on Graves’ Orbitopathy (EUGOGO) classification most used in Europe.
Management
Patients are typically managed with input from both ophthalmology and endocrine specialists.
In patients with hyperthyroidism, thyroid hormone levels should be corrected to achieve euthyroidism.
Smoking cessation advice should be given to reduce the risk of further exacerbations. If patients are reporting symptoms from corneal exposure, artificial tears and tapes can be used to provide relief.
In severe cases, steroids can be used to reduce inflammation and swelling, with IV methylprednisolone as the first line for compressive optic neuropathy. Some patients may require surgery, such as orbital decompression and lid surgery, if there is significant corneal exposure or progressing proptosis.1,3
Complications
Complications of thyroid eye disease include:
- Loss of sight secondary to compressive optic neuropathy
- Globe subluxation: eye ‘popping out’
- Gaze abnormalities
- Raised intraocular pressure leading to glaucoma
Key points
- Thyroid eye disease is an autoimmune disease, most commonly associated with Grave’s disease
- Smoking is the single largest modifiable risk factor
- Dry eye symptoms, eyelid retraction and lid lag are common manifestations
- Thyroid function tests, antibody testing and imaging can aid diagnosis, which is based on clinical history and examination
- The initial management of patients involves thyroid therapy to achieve euthyroidism and smoking cessation
- Patients who develop compressive optic neuropathy require urgent admission and intravenous methylprednisolone treatment
- Surgical management is typically considered for patients with severe corneal disease or worsening proptosis
- Complications can include blindness, globe subluxation and glaucoma
Reviewer
Consultant Ophthalmologist
Editor
Dr Chris Jefferies
References
- Weiler D. Thyroid eye disease: a review. 2016. Available from: [LINK]
- Garrity J and Bahn R. Pathogenesis of Graves Ophthalmopathy: Implications for Prediction, Prevention, and Treatment. 2006. Available from: [LINK]
- EyeWiki. Thyroid Eye Disease. Available from: [LINK]
- Bahn R. Graves’ Ophthalmopathy. 2010. Available from: [LINK]
- CNX OpenStax. OSC Microbio 19 02 exophth. License: [CC BY 4.0]
- Tran H and Reeves G. Graves Ophthalmology MRT 01. License: [CC BY-SA 2.0]