- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
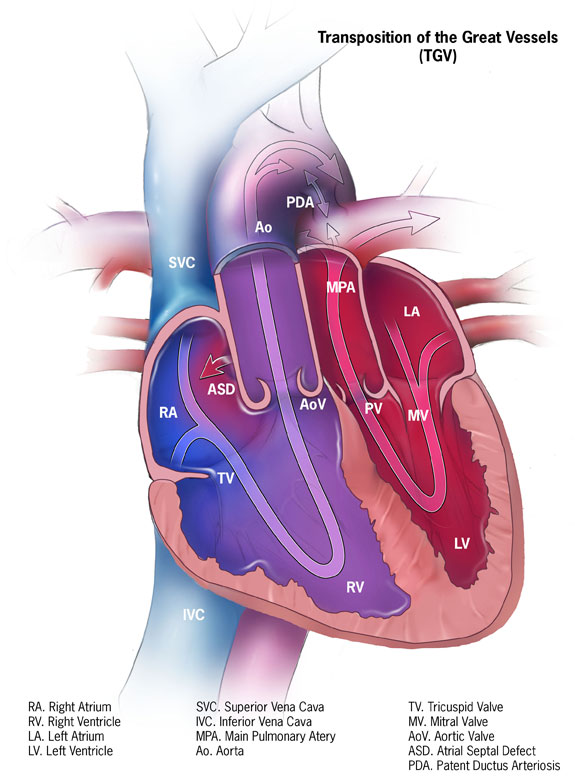
Transposition of the great arteries (TGA) is a congenital heart condition where the attachments of the pulmonary trunk and the aorta to the heart are swapped (“transposed”).
TGA accounts for about 3% of all congenital heart disease and 20% of all cyanotic heart disease.
Aetiology
The aorta arises from the right ventricle, and the pulmonary artery arises from the left ventricle. This results in two separate circulations that do not mix: the left side of the heart travels through the pulmonary system, and the right side travels through the systemic system.
This does not cause a problem during pregnancy as gas and nutrient exchange occurs in the placenta, and blood does not flow to the lungs. Immediately after birth, the condition is life-threatening, and the baby will become cyanosed.
Immediate survival is dependent on a shunt existing between the two separate circulations. This allows blood to become oxygenated in the lungs as it flows around the body. This shunt can be present as a patent ductus arteriosus, ventricular septal defect or atrial septal defect.
There are two types of TGA:
- Dextro transposition of the great arteries (D-TGA), also called complete TGA: this is the most common form of TGA. The aorta is found on the right of the pulmonary artery. Commonly, D-TGA needs to be repaired within a year of life.
- Levo transposition of the great arteries (L-TGA), also called congenitally corrected transposition: the aorta is found on the left of the pulmonary artery. Without any other heart defects present, this may not need repair early in life.
Risk factors
Risk factors for transposition of the great arteries include:
- Pregnancy-related health concerns (e.g. alcoholism, smoking, rubella and uncontrolled diabetes)
- Family history of congenital heart disease
TGA is commonly accompanied by other cardiac conditions, including a ventricular septal defect, coarctation of the aorta and pulmonary stenosis.
Clinical features
The clinical presentation of TGA occurs during the neonatal period, when the ductus arteriosus begins to close physiologically (days 2-3).
History
In neonates, clinical features of TGA include:
- Poor feeding
- Sweating during feeds
- Poor weight gain
- Tachypnoea and respiratory distress
Clinical examination
In a neonate, commonly, the only clinical sign of coarctation is weak femoral pulses. Other signs on clinical examination in infancy include:
- Cyanosis
- Tachycardia
- Loud S2 heart sound
- A murmur can be present depending on the shunt
Differential diagnoses
Differential diagnoses to consider include other cyanotic congenital heart diseases:
- Tricuspid atresia (Ebstein’s anomaly)
- Double-outlet right ventricle
- Pulmonary atresia
- Tetralogy of Fallot
- Truncus arteriosus
Investigations
TGA is commonly diagnosed during pregnancy at antenatal ultrasound scans. This diagnosis requires close monitoring during pregnancy, and arrangements regarding birth planning must be made so that the woman gives birth in a hospital where the condition can be safely and appropriately managed after birth.
Bedside investigations
Relevant bedside investigations include:
- Pulse oximetry: hypoxia suggesting possible cyanotic heart disease
- ECG: likely normal at first. Commonly, after a few days, right ventricular hypertrophy is present
Imaging investigations
Relevant imaging investigations include:
- Foetal ultrasounds: abnormal vessels within the heart may be identified at the routine anomaly scan (at approximately 20 weeks gestation). A foetal echocardiogram may then be performed to confirm the diagnosis.
- Chest X-ray: may see classic “egg on a string” appearance and increased vascular lung markings.
- Echocardiogram: determines the nature of the TGA to establish diagnosis and management options and identifies any associated cardiac abnormalities.
Diagnosis
Early diagnosis is important because in TGA, blood flow commonly relies on a patent ductus arteriosus. Two to three days after birth, the ductus arteriosus closes; therefore, if left untreated, the condition worsens rapidly.
Management
If a shunt is present alongside TGA, it provides some time for definitive treatment.
Medical management
Supplemental oxygen may be required if oxygen saturations are low.
All deteriorating ductal-dependent lesions are treated with prostaglandin. Prostaglandin E1 is prescribed to maintain the ductus arteriosus until surgery. This allows blood to flow into the systemic circulation.
Surgical management
Following medical management, surgery is performed to close the ductus arteriosus and correct the coarctation.
Surgical options include balloon atrial septostomy to increase the mixing of the two circulatory systems and arterial switch procedure.
Balloon atrial septostomy
Balloon septostomy involves inserting a catheter through the umbilicus into the foramen ovale and inflating a balloon to form a large atrial septal defect.2
This means that blood on the left side of the heart returning from the lungs can flow to the right side of the heart and out via the aorta to the body. After this, the patent ductus arteriosus is no longer required and so the prostaglandin infusion can be stopped.
Arterial switch procedure
The definitive management is open heart surgery. An “arterial switch” procedure is performed using a cardiopulmonary bypass machine within the first few days of life2. If present, a ventricular septal defect, atrial septal defect, or patent ductus arteriosus can be corrected during this procedure.
Complications
Without treatment, 90% of infants will die within the first year of life.
Complications of TGA include:
- Heart failure
- Complete heart block
- Valvular disease
- Coronary artery disease
Complications can also occur after corrective treatment. These include:
- Arrhythmias
- Pulmonary artery stenosis
- Coronary artery stenosis
- Aortic regurgitation
Key points
- Transposition of the great arteries is occurs when the attachments of the aortic arch and pulmonary artery to the heart are swapped
- The systemic and pulmonary circulation do not mix and so you get deoxygenated blood travelling around the body
- Common symptoms in a neonate include increased work of breathing, poor feeding and poor weight gain
- Common clinical findings in infancy include cyanosis, tachycardia and a loud S2 heart sound
- Foetal ultrasounds, ECG, chest X-ray and an echocardiogram are the primary investigations
- Treatment involves the administration of prostaglandin E1 and oxygen until corrective surgery
- Surgical options include balloon septostomy and arterial switch procedure (open heart surgery)
- Complications can include heart failure, coronary artery disease and valvular disease
Reviewer
Dr Akmal Hussain
Consultant Paediatrician
Editor
Dr Chris Jefferies
References
- Centers for Disease Control and Prevention. License: [Public domain]
- Séguéla PE, Roubertie F, Kreitmann B, Mauriat P, Tafer N, Jalal Z, Thambo JB. Transposition of the great arteries: Rationale for tailored preoperative management. Arch Cardiovasc Dis. February 2017.