- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Taking an ascitic tap (diagnostic paracentesis) involves using a needle and syringe to take a sample of ascitic fluid from a patient’s abdomen.
This procedure is used to diagnose the cause of ascites and to exclude the presence of spontaneous bacterial peritonitis.
This guide provides a step-by-step approach to performing an ascitic tap in an OSCE setting, it is NOT intended to be used to guide patient care.
Gather equipment
Gather the appropriate equipment to perform an ascitic tap:
- Sterile gloves
- Apron
- Dressings pack
- Sterile surface (nursing trolley which has been appropriately cleaned)
- Syringe (usually 10ml or 20ml)
- Green needle (19G)
- Sharps container
- Chlorhexidine swab (e.g ChloraPrep™)
- Specimen container (usually a white top specimen pot)
- Sterile dressing
Local anaesthetic
Using local anaesthetic when performing an ascitic tap depends on patient choice. Some patients may opt not to have local anaesthetic administered as this involves fewer needles. In an OSCE setting, local anaesthetic should always be offered for an ascitic tap.
If local anaesthetic is being used, additional equipment includes:
- Lidocaine 1% or 2%
- Drawing up needle
- Orange needle (25G)
- Green needle (19G)
- 20ml syringe
Ultrasound (if available)
Ideally, ultrasound is used to confirm the presence of ascites and identify a suitable needle insertion site. However, it is possible to perform this procedure without ultrasound.
Introduction
Wash your hands using alcohol gel. If your hands are visibly soiled, wash them with soap and water.
Don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Explain what the procedure will involve using patient-friendly language: “I need to take a sample of fluid from your abdomen. It will be tested in the lab to find out the cause and whether the fluid is infected. This procedure involves me inserting a needle into your abdomen. It may be a little painful, however, it should not take long. I can administer some local anaesthetic to the area which will reduce the pain when I take the sample. There are a few risks associated with this procedure, these include infection, pain bleeding, and very rarely damage to the surrounding structures in your abdomen.”
Gain consent to proceed with an ascitic tap.
Check if the patient has an allergy to local anaesthetic (if requested) or to the skin preparation agent.
Check for any contraindications
Ask the patient if they have any pain before continuing with the clinical procedure.
Ascitic tap contraindications
Infection overlying the intended needle insertion site is a contraindication to performing an ascitic tap. If an infection is present, select another site on the patient’s abdomen to take the sample.
Other cautions (but not contraindications) include:
- Coagulopathy (INR >2.0)
- Platelets <50
- Pregnancy
- Organomegaly
Confirm ascites and identify insertion site
Position the patient so that they are lying flat.
Perform an abdominal examination to confirm the presence of ascites (shifting dullness).
Whilst confirming ascites, find the optimal location for needle insertion using percussion. This will be the area of the abdomen where the volume of ascites is greatest whilst the patient is lying flat and has the dullest percussion note.
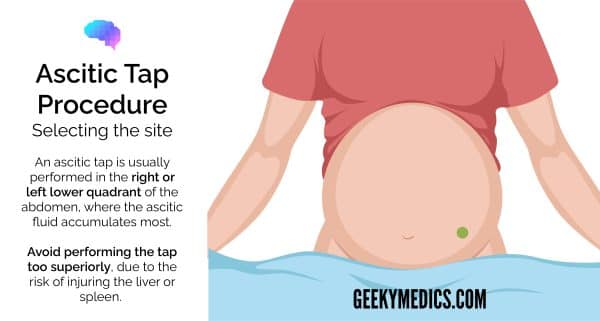
Ascitic tap location
An ascitic tap is usually performed in the right or left lower quadrant of the abdomen, where the ascitic fluid accumulates most. Avoid performing the tap too superiorly, due to the risk of injuring the liver or spleen.
It is important to avoid the inferior epigastric artery which runs within the rectus sheath approximately 4-8cm from the midline.
If available: use ultrasound to assess the location of ascites further and to find the ideal location for needle insertion.
Remove equipment from its packaging and place it onto a sterile surface so that it is easily accessible during the procedure.
Prepare the insertion site
Wash your hands and don sterile gloves and an apron.
Clean the insertion site and the surrounding area thoroughly using chlorhexidine solution and allow it to dry.
Perform the ascitic tap
Local anaesthetic
If the patient wishes to have local anaesthetic, prepare and administer lidocaine subcutaneously using an orange needle (25G) over the planned puncture site (create a bleb). Aspirate to ensure you are not in a blood vessel.
Replace the 25G orange needle with a 19G green needle.
Administer lidocaine deeper into the tissue, aspirating as you go until you get a flashback of ascitic fluid.
Collect a sample of ascitic fluid
Attach a 19G green needle to a 20ml syringe.
Holding the needle perpendicular to the skin, insert the needle into the previously identified location on the patient’s abdomen.
Advance the needle slowly, ensuring you aspirate as you advance.
Advance and aspirate until ascitic fluid is aspirated into the syringe.
Aspirate 20ml of ascitic fluid.
Z-track technique
The Z-track technique is an alternative technique which can be used to reduce leakage of ascitic fluid following paracentesis.
The skin is stretched approximately 2cm before inserting the needle into the epidermis. The skin is held in this position whilst the needle is advanced. The skin is then released after the needle has been removed. This technique creates a non-linear path between the skin and abdominal cavity.

Removal of the needle
Withdraw the needle, disconnect it from the syringe and dispose of the needle in a sharps bin.
Apply a sterile dressing to the area.
Place the aspirated ascitic fluid into appropriate specimen containers.
If unable to aspirate ascitic fluid
Seek senior advice if you are unable to aspirate ascitic fluid. An ultrasound scan may be required (if not already performed) to confirm the presence of ascites and mark the ideal needle insertion point.
To complete the procedure…
Explain to the patient that the procedure is now complete.
Thank the patient for their time.
Document the patient’s details on the specimen containers at the bedside (using either pre-printed or handwritten labels).
Dispose of PPE and other clinical waste into an appropriate clinical waste bin.
Wash your hands.
Document the details of the procedure including:
- Whether local anaesthetic was used
- Volume and colour of ascitic fluid aspirated
- Any immediate post-procedure concerns or complications
Send the ascitic samples to the lab for analysis in an appropriate plastic leak-proof bag with the completed laboratory request form:
- Cytology
- Gram staining
- Microscopy, culture and sensitivity
- Albumin, protein, LDH, glucose, white cell count
For more information on interpreting results, see the Geeky Medics guide to ascitic fluid analysis.
Reviewers
Dr Coral Hollywood
Consultant Gastroenterologist
Dr Richard Makins
Consultant Gastroenterologist