- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Spine examination frequently appears in OSCEs and you’ll be expected to identify the relevant clinical signs using your examination skills. This spine examination OSCE guide provides a clear step-by-step approach to examining the spine, with an included video demonstration. Musculoskeletal examinations can be broken down into four key components: look, feel, move and special tests. This structure can be helpful as an aide-memoire if you begin to feel like you’ve lost your way during an OSCE.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language.
Gain consent to proceed with the examination.
Adequately expose the patient’s upper body and provide a blanket to cover the patient when not being examined.
Position the patient standing for initial inspection of the spine.
Ask the patient if they have any pain before proceeding with the clinical examination.
Look
General inspection
Clinical signs
Perform a brief general inspection of the patient, looking for clinical signs suggestive of underlying pathology:
- Body habitus: obesity is a significant risk factor for joint pathology due to increased mechanical load (e.g. osteoarthritis).
- Scars: may provide clues regarding previous spinal surgery.
- Wasting of muscles: suggestive of disuse atrophy secondary to joint pathology.
Objects or equipment
Look for objects or equipment on or around the patient that may provide useful insights into their medical history and current clinical status:
- Aids and adaptations: examples include walking aids and wheelchairs.
- Prescriptions: prescribing charts or personal prescriptions can provide useful information about the patient’s recent medications (e.g. analgesia).
Closer inspection of the spine
Ask the patient to stand and turn in 90° increments as you inspect the spine from each angle for evidence of pathology.
Anterior inspection
Inspect the anterior aspect of the spine, noting any abnormalities:
- Scars: note the location of the scar as this may provide clues as to the patient’s previous surgical history or suggest previous trauma (e.g. anterior neck scar due to anterior cervical discectomy).
- Posture: note any asymmetry which may indicate joint pathology or scoliosis.
- Asymmetry of the shoulder girdle: may be caused by scoliosis, arthritis, fractures or dislocation.
- Pelvic tilt: lateral pelvic tilt can be caused by scoliosis, leg length discrepancy or hip abductor weakness.
Lateral inspection
Inspect the lateral aspect of the spine, noting any abnormalities:
- Cervical lordosis: hyperlordosis is associated with chronic degenerative joint disease (e.g. osteoarthritis).
- Thoracic kyphosis: the normal amount of thoracic kyphosis is typically between 20-45º. Hyperkyphosis is associated with Scheuermann’s disease (congenital wedging of the vertebrae).
- Lumbar lordosis: loss of normal lumbar lordosis is associated with sacroiliac joint disease (e.g. ankylosing spondylitis).
Posterior inspection
Inspect the patient from the behind noting any abnormalities:
- Spinal alignment: inspect for lateral curvature of the spine indicative of scoliosis.
- Iliac crest alignment: misalignment may indicate a leg length discrepancy or hip abductor weakness.
- Muscle wasting: note any wasting of the paraspinal muscles which may indicate chronic spinal pathology and reduced mobility.
- Abnormal hair growth: may indicate underlying bony abnormalities such as spina bifida.
- Bruising: suggestive of recent trauma or surgery.
Gait
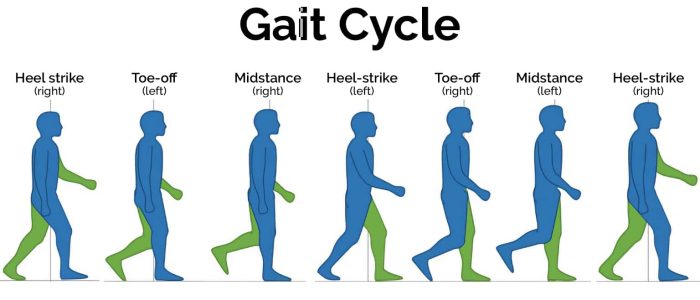
Ask the patient to walk to the end of the examination room and then turn and walk back whilst you observe their gait paying attention to:
- Gait cycle: note any abnormalities of the gait cycle (e.g. abnormalities in toe-off or heel strike).
- Range of movement: often reduced in the context of chronic joint pathology (e.g. osteoarthritis, inflammatory arthritis).
- Limping: may suggest joint pain (i.e. antalgic gait) or weakness.
- Leg length: note any discrepancy which may be the cause or the result of joint pathology.
- Turning: patients with joint disease may turn slowly due to restrictions in joint range of movement or instability.
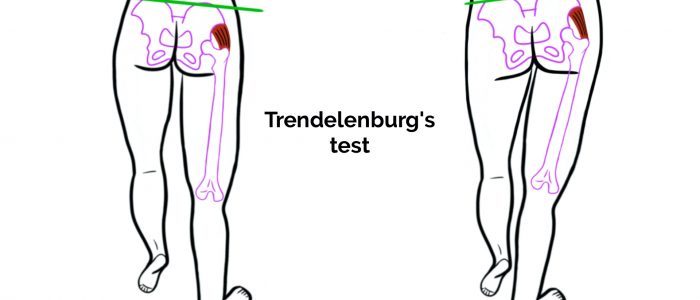
- Trendelenburg’s gait: an abnormal gait caused by unilateral weakness of the hip abductor muscles secondary to a superior gluteal nerve lesion or L5 radiculopathy.
- Waddling gait: an abnormal gait caused by bilateral weakness of the hip abductor muscles, typically associated with myopathies (e.g. muscular dystrophy).
- Assess the patient’s footwear: unequal sole wearing is suggestive of an abnormal gait.
Gait cycle
The gait cycle has six phases:
- Heel-strike: initial contact of the heel with the floor.
- Foot flat: weight is transferred onto this leg.
- Mid-stance: the weight is aligned and balanced on this leg.
- Heel-off: the heel lifts off the floor as the foot rises but the toes remain in contact with the floor.
- Toe-off: as the foot continues to rise the toes lift off the floor.
- Swing: the foot swings forward and comes back into contact with the floor with a heel strike (and the gait cycle repeats).

Feel
Palpate the spinal processes and sacroiliac joints, assessing their alignment and noting any tenderness.
Palpate the paraspinal muscles noting any tenderness or muscular spasms.
Move
For each of the movements described below, assess active movement and if abnormalities are identified repeat the movements passively.
Active movement refers to a movement performed independently by the patient. Ask the patient to carry out a sequence of active movements to assess joint function. As the patient performs each movement, note any restrictions in the range of the joint’s movement and also look for signs of discomfort. It’s important to clearly explain and demonstrate each movement you expect the patient to perform to aid understanding.
Passive movement refers to a movement of the patient, controlled by the examiner. This involves the patient relaxing and allowing you to move the joint freely to assess the full range of joint movement. It’s important to feel for crepitus as you move the joint (which can be associated with osteoarthritis) and observe any discomfort or restriction in the joint’s range of movement. If abnormalities are noted on active movements (e.g. restricted range of movement), assess joint movements passively.
Cervical spine
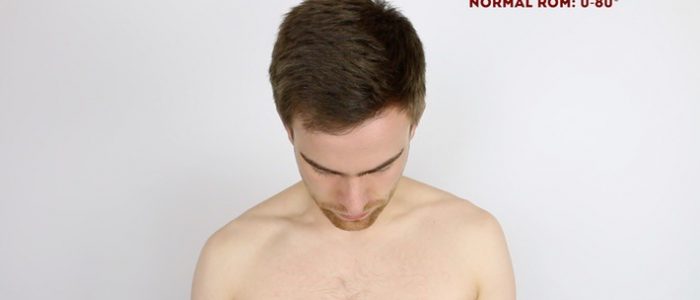
Flexion of the cervical spine
Normal range of movement: 0°- 80°
Instructions: Ask the patient to touch their chin to their chest.
Extension of the cervical spine
Normal range of movement: 0°- 50°
Instructions: Ask the patient to look up at the ceiling.
Lateral flexion of the cervical spine
Normal range of movement: 0°- 45°
Instructions: Ask the patient to touch their ear to their shoulder on each side.
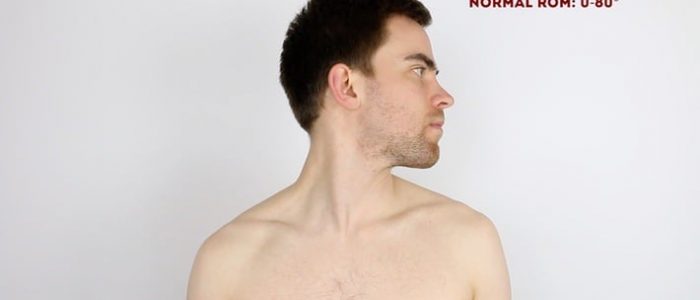
Rotation of the cervical spine
Normal range of movement: 0°- 80°
Instructions: Ask the patient to turn their head to the left and the right.
Lumbar spine
Flexion of the lumbar spine
Instructions: Ask the patient to touch their toes whilst keeping their legs straight.
Extension of the lumbar spine
Normal range of movement: 10°- 20°
Instructions: Ask the patient to lean back as far as they are comfortably able, whilst you’re positioned close to them for support if required.
Lateral flexion of the lumbar spine
Instructions: Ask the patient to slide their left hand down the outer aspect of their left leg as far as they are able to whilst keeping their legs straight. Then ask them to repeat by sliding their right hand over their right leg.
Thoracic spine
Rotation of the thoracic spine
Instructions: Ask the patient to sit on the side of the clinical examination couch and cross their arms across their chest. Then ask them to turn to the left and the right as far as they are comfortably able to.
Special tests
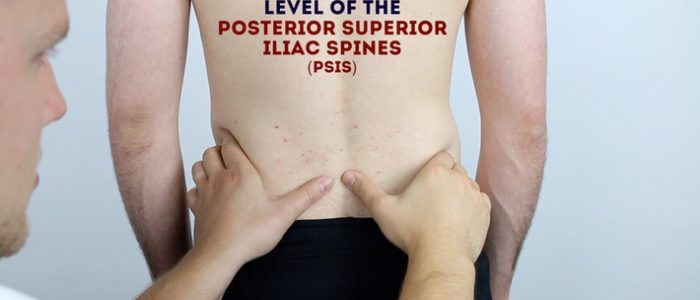
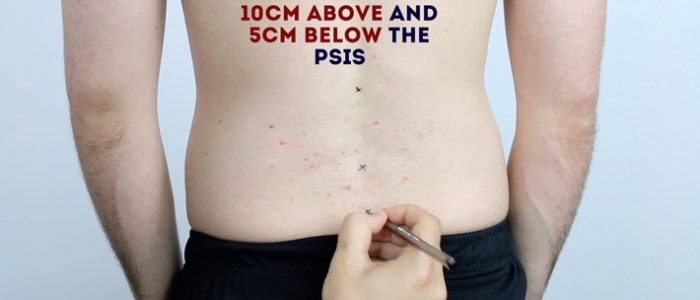
Schober’s test
Schober’s test can be used to identify restricted flexion of the lumbar spine, which may occur in conditions such as ankylosing spondylitis.
Assessment
1. Identify the location of the posterior superior iliac spine (PSIS) on each side.
2. Mark the skin in the midline 5cm below the PSIS.
3. Mark the skin in the midline 10cm above the PSIS.
4. Ask the patient to touch their toes to assess lumbar flexion.
5. Measure the distance between the two lines.
Interpretation
If a patient has normal lumbar flexion the distance between the two marks should increase from the initial 15cm to more than 20cm.
Reduced range of motion is associated with conditions such as ankylosing spondylitis.
Sciatic stretch test (a.k.a. straight leg raise)
The sciatic stretch test is used to identify sciatic nerve irritation.
Assessment
1. Position the patient supine on the clinical examination couch.
2. Holding the patient’s ankle, raise their leg by passively flexing the hip whilst keeping the patient’s knee fully extended.
3. The normal range of movement for passive hip flexion is approximately 80-90º.
4. Once the patient’s hip is flexed, dorsiflex the patient’s foot.
Interpretation
The sciatic stretch test is considered positive if the patient experiences pain in the posterior thigh or buttock region.
A positive test is suggestive of sciatic nerve irritation (e.g. secondary to lumbar disc prolapse).
Femoral nerve stretch test
The femoral nerve stretch test is used to identify femoral nerve irritation.
Assessment
1. Position the patient prone on the clinical examination couch.
2. Flex the patient’s knee to 90º and then extend the hip joint.
3. Finally, plantarflex the patient’s foot.
Interpretation
The femoral nerve test is considered positive if the patient experiences pain in the thigh and/or inguinal region.
To complete the examination…
Explain to the patient that the examination is now finished.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Example summary
“Today I examined Mr Smith, a 32-year-old male. On general inspection, the patient appeared comfortable at rest, with no stigmata of musculoskeletal disease. There were no objects or medical equipment around the bed of relevance.”
“Assessment of the spine revealed normal alignment, with no tenderness on palpation. The range of movement of the cervical, thoracic and lumbar spine was normal.”
“In summary, these findings are consistent with a normal examination of the spine.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
- Neurovascular examination of the upper and lower limbs.
- Examination of the hip and shoulder joints.
- Further imaging if indicated (e.g. X-ray/MRI).
Reviewer
Tejas Yarashi
Consultant Trauma & Orthopaedic Surgeon
References
- Weiss HR. Adapted by Geeky Medics. Scoliosis. Licence: CC BY.