- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The larynx is the most common site for head and neck malignancy with an incidence of 26% in men and 13% in women.
Most laryngeal cancers are squamous cell carcinomas (SCC), however other rarer malignancies can present in the larynx including papillary carcinomas, sarcomas, and melanomas.1
Head and neck malignancy is the eighth most common malignancy worldwide accounting for 3% of all cancer cases.
Symptoms of head and neck malignancy can be insidious (63% of patients are diagnosed at advanced stages).
1 in 10 head and neck SCC patients will have a separate synchronous malignancy (occurrence of a second primary malignancy).2
Aetiology
Anatomy
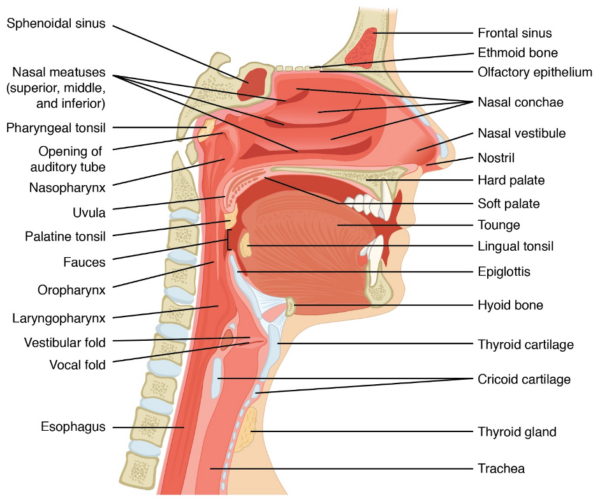
The larynx is located in the anterior neck at the level of C3 to C6. It forms part of the upper aerodigestive tract, with its main functions including phonation and protection of the lower respiratory tract (Figure 1).
Structure of the larynx
Structurally, the larynx is divided into 3 main areas:
- Supraglottis: above the level of the vocal cords
- Glottis: at the level of the vocal cords and the
- Subglottis: below the level of the vocal cords
The supraglottis contains the suprahyoid epiglottis, the infrahyoid epiglottis, the false cords, the aryepiglottic folds and the arytenoids. Malignancy at this site often invades the vallecula and base of the tongue. Lymphatic involvement is common and 55% of patients will have nodal metastases at initial presentation.3
The glottis contains the true vocal cords only. As it is a lymphatic watershed area, nodal metastases are uncommon.
The subglottis includes everything below the level of the vocal cords.
Anatomical borders of the larynx
Anteriorly the larynx is bounded by the:
- Infrahyoid or strap muscles (sternohyoid muscle, sternothyroid muscle, thyrohyoid muscle, omohyoid muscle)
- Thyroid gland
- Parathyroid glands
Laterally the larynx is bounded by the:
- Common carotid artery
- Internal jugular vein
- Vagus nerve
- Recurrent laryngeal nerve
Posteriorly the larynx is bounded by the oesophagus.
Blood supply of the larynx
Arterial blood is supplied via the superior laryngeal artery (a branch of the superior thyroid artery) and the inferior laryngeal artery. Venous drainage is similarly via the superior and inferior laryngeal veins.
Innervation of the larynx
The main nerves supplying the larynx are the superior laryngeal nerve and the recurrent laryngeal nerve.
Superior laryngeal nerve (external branch):
- Cricothyroid muscle
Recurrent laryngeal nerve (inferior branch):
- Posterior cricoarytenoid muscle
- Lateral cricoarytenoid muscle
- Transverse and oblique arytenoid muscles
Lymphatic drainage of the larynx
The lymphatic drainage to the supraglottis is achieved via the pre-epiglottic and upper deep cervical nodes. The vocal cords are a lymphatic watershed area which accounts for the low risk of lymphatic spread. The subglottis drains to lower deep cervical and pretracheal nodes.
Pathophysiology
Repeated exposure of head and neck mucosa to various aerosolised carcinogens (e.g. tobacco smoke) leads to acquired genetic mutations causing a field of cancerisation effect. This occurs when cells within a mucosal area become more susceptible to tumour formation.
A minimum of 4 to 6 mutations are thought to be required for progression to solid tumours.4
The field of cancerisation effect explains the high association of synchronous malignancies (occurrence of a second primary malignancy) in the upper aerodigestive tract.
Risk factors
Risk factors for laryngeal cancer include:6,8
- Smoking: over 80% of head and neck cancers are thought to be caused by tobacco, alcohol or a combination of both.
- Alcohol: whilst alcohol is not directly carcinogenic, it is metabolised by the liver into acetaldehyde which is highly mutagenic.
- Age: the incidence increases with age and it is most common in the 5th and 7th decade of life.
- Poor oral hygiene: this has also been shown to play a contributing factor in the development of head and neck cancers.
- Human papillomavirus (HPV) infection: currently, at least 2.4% of cases of laryngeal malignancy are attributable to HPV infection and this number is likely to rise.
Clinical features
Clinical features can vary depending on the anatomical location of laryngeal cancer.
Glottic tumours are more likely to present with hoarseness and stridor, and patients will therefore present earlier. Tumours at other sites can be silent until they are at a more advanced stage.
Some patients will present with enlarged neck nodes only.
History
Typical symptoms of laryngeal cancer include:
- Hoarseness
- Stridor
- Dysphagia
- Odynophagia
- Voice change
- Referred otalgia
- Haemoptysis
- Neck lump
- Weight loss
Other important areas to cover in the history include:
- Past medical history (e.g. previous malignancy, gastro-oesophageal reflux disease)
- Smoking history
- Alcohol history
- Allergies
- Occupation (excessive voice use e.g. professional singer)
Clinical examination
Patients presenting with features of head and neck cancer require a thorough examination of the oral cavity and a neck lump examination. A cranial nerve examination may also be relevant if there is concern about neural impingement.
All patients will direct visualisation of the larynx, usually by flexible nasolaryngoendoscopy or direct laryngoscopy.
Differential diagnoses
Papillomas
Papillomas are benign wart-like vocal cord lesions arising secondary to HPV infection. They present with cough, hoarseness and can progress to stridor. Diagnosis is usually clinical using direct visualisation and later confirmed with a biopsy.
Granulomas
The vocal cords can occasionally develop small inflammatory lesions (granulomas). These can develop in response to chronic use or in the presence of gastro-oesophageal reflux. Patients can present with dry cough, dysphonia, hoarseness and feeling of a lump in the throat.
Vocal cord polyps
Vocal cord polyps are another common cause for hoarseness in patients with excessive voice use. These are usually small and bilateral and cause hoarseness which is typically worse at the end of the day.
Vocal cord cysts
Cysts on the vocal cords can also present with hoarseness, chronic cough and feeling of lump in the throat. Mucous retention cysts are small, soft vocal cord lumps and develop as a result of a blocked mucus producing gland.
Investigations
Bedside investigations
Direct examination of the larynx via a flexible nasal endoscope or direct laryngoscope can usually be undertaken in clinic. This can show vocal cord lesions as well as immobility of the vocal cords.
Imaging
Patients can either be investigated with CT or MRI of the head and neck with contrast. Positron emission tomography (PET) is required to identify distant metastases.
Other investigations
Direct examination of the whole upper aerodigestive tract (pan-endoscopy) under a general anaesthetic is required for comprehensive clinical assessment. This allows for biopsies to be taken and identification of secondary malignancies.
Staging
Head and neck malignancies are staged according to the TNM classification where T refers to tumour size, N refers to nodal metastases and M refers to distant metastases. Staging is determined as per the American Joint Committee on Cancer system.
Management
Early-stage laryngeal cancer can be managed with either transoral resection of the primary lesion or primary radiotherapy.
Advanced stage malignancy can be managed with organ-preserving approaches in the form of curative primary chemo-radiotherapy.
An alternative approach in advanced stages is primary surgery and adjuvant radiotherapy. The main determinant in deciding between the two approaches is the baseline speech and airway function on presentation.
The larynx can be removed partially in the form of a supraglottic laryngectomy or a hemilaryngectomy if disease is early and localised. This can avoid the need for an artificial airway.
However, patients with laryngeal cancer most often require a total laryngectomy. This removes the larynx and brings the trachea to the skin surface as a stoma. Often, a rim of hypopharynx needs to also be removed and reconstructed at the time of procedure either by primary closure or with the aid of a skin flap.
Complications
If left untreated, laryngeal cancer will occlude the airway and invade adjacent structures such as the oesophagus, trachea, nerves (recurrent laryngeal, vagus, hypoglossal, accessory) and vessels (carotid artery, internal and external jugular veins).
Common post-operative complications following a laryngectomy include:
- Local complications: wound infection and breakdown leading to pharyngo-cutaneous fistulas, bleeding and haematoma formation
- Airway issues requiring emergency treatment
- Long-term dysphagia
Risk of complications is increased in patients who also undergo lymph node dissection and radiotherapy.
Prognosis
Survival rates vary depending on the cancer stage at initial diagnosis as well as the initial location of the tumour (Table 2). Cancer of the vocal cords is the most common type of laryngeal cancer and has a survival rate of 83% if detected early.
Table 2. Survival rates in laryngeal cancer.10
| Location | Survival rate |
| Supraglottis | 46% |
|
Local disease Regional disease Metastatic disease |
61% 47% 30% |
| Glottis | 76% |
|
Local disease Regional disease Metastatic disease |
83% 48% 42% |
| Subglottis | 52% |
|
Local disease Regional disease Metastatic disease |
60% 33% 45% |
Key points
- Laryngeal cancer describes any malignant lesion located at the supraglottis, glottis or subglottis.
- The histology of the majority of laryngeal cancer is squamous cell carcinoma.
- The main risk factors for developing laryngeal cancer are smoking, alcohol, increasing age, poor oral hygiene and HPV infection.
- Common symptoms include hoarseness, dysphagia, stridor, otalgia, neck lump and weight loss.
- Findings on clinical examination may include intra-oral mass, lymphadenopathy and in some cases cranial nerve palsies.
- All patients with a recent change to their voice or new lymphadenopathy require assessment with flexible nasolaryngoendoscopy.
- Management of laryngeal cancer involves a combination of surgery and radiotherapy.
- A laryngectomy removes the whole of the larynx and brings the trachea to the skin as a stoma.
- If left untreated, laryngeal cancer will progress to occlude the airway and erode the neck vessels.
- Prognosis depends on the anatomical location and stage of the tumour at initial clinical presentation.
Reviewer
Mr Arun Takhar
Head and Neck Fellow
Editor
Dr Chris Jefferies
References
Text references
- Ciolofan MS, Vlăescu AN, Mogoantă C-A, et al. Clinical, Histological and Immunohistochemical Evaluation of Larynx Cancer. Curr Heal Sci J 2017; 43: 367–375.
- Wang WL, Chang WL, Yang HB, et al. Quantification of tumor infiltrating Foxp3+ regulatory T cells enables the identification of high-risk patients for developing synchronous cancers over upper aerodigestive tract. Oral Oncol 2015; 51: 698–703.
- Koroulakis A, Agarwal M. Cancer, Laryngeal. StatPearls Publishing. Available from: [LINK]
- Almadori G, Bussu F, Cadoni G, et al. Multistep laryngeal carcinogenesis helps our understanding of the field cancerisation phenomenon: A review. Eur J Cancer 2004; 40: 2383–2388.
- Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: A brief review of recent epidemiological evidence. In: Lung Cancer. 2004. Epub ahead of print August 2004. DOI: 10.1016/j.lungcan.2004.07.998.
- Osazuwa-Peters N, Boakye EA, Chen BY, et al. Association between head and neck squamous cell carcinoma survival, smoking at diagnosis, and marital status. JAMA Otolaryngol – Head Neck Surg 2018; 144: 43–50.
- Homann N, Tillonen J, Meurman JH, et al. Increased salivary acetaldehyde levels in heavy drinkers and smokers: a microbiological approach to oral cavity cancer. Carcinogenesis 2000; 21: 663–8.
- Martel C de, Plummer M, Vignat J, et al. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer 2017; 141: 664–670.
- Kiaris H, Ergazaki M, Segas J, et al. Detection of Epstein-Barr virus genome in squamous cell carcinomas of the larynx. Int J Biol Markers 1995; 10: 211–215.
- Cancer.Net. Laryngeal and Hypopharyngeal Cancer: Statistics. Available from: [LINK]
Image references
- Figure 1. OpenStax College. Anatomy of Nose-Pharynx-Mouth-Larynx. License: [CC-BY]. Available from: [LINK]




