- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A patent ductus arteriosus is the failure of the ductus arteriosus to close within the first 72 hours of life.1 This is more common in premature infants but also occurs in term infants.
Patent ductus arteriosus accounts for up to 10% of all congenital heart defects.
Aetiology
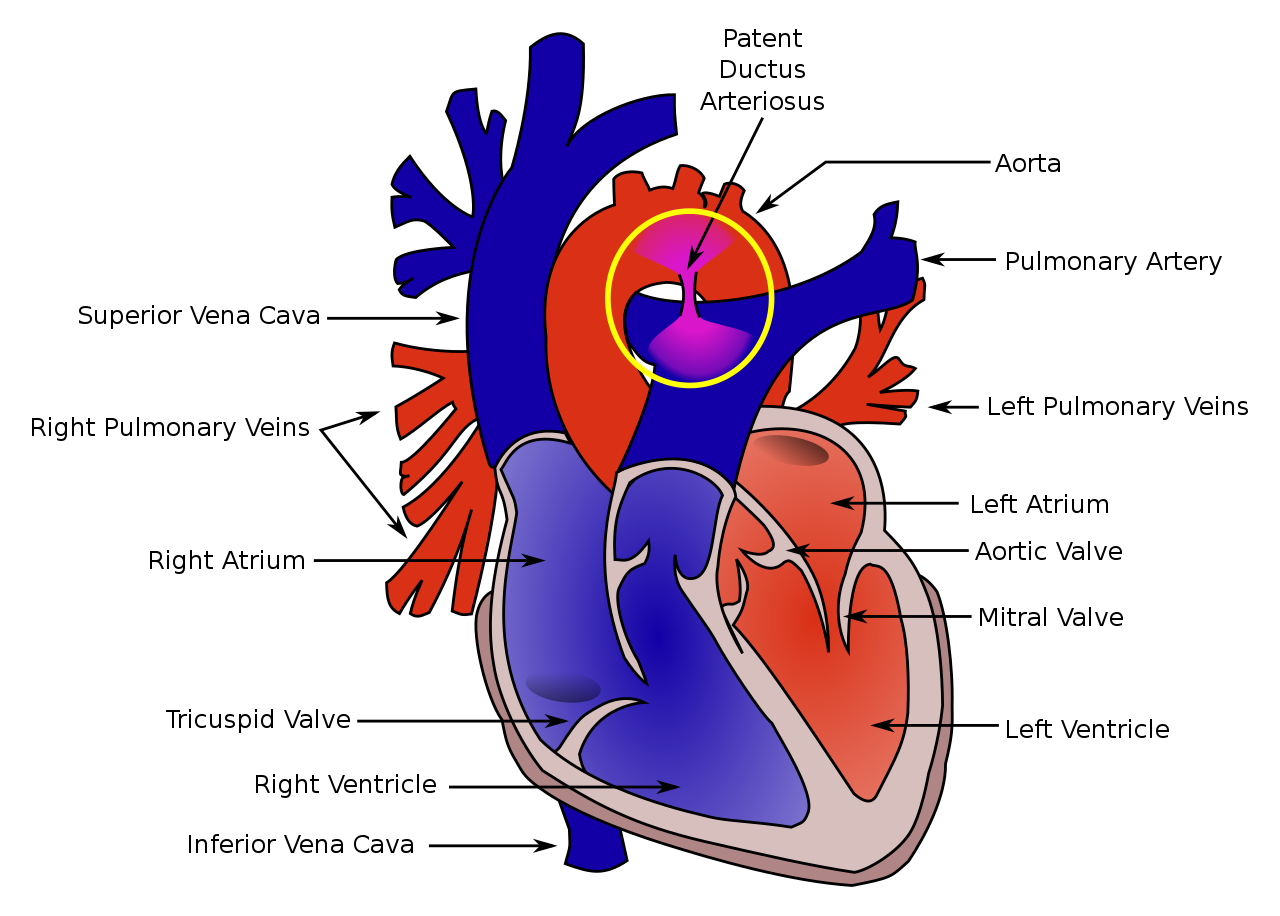
The ductus arteriosus is a key part of fetal circulation, connecting the pulmonary arteries with the aorta to bypass the lungs in utero.
After delivery, the rapid decrease in pulmonary vascular resistance diverts blood through the pulmonary circulation, while the increase in PaO2 and decline in prostaglandin causes the ductus arteriosus to close.
In some situations, this does not happen, leading to a patent ductus arteriosus (Figure 1). A large PDA can lead to the development of a left-to-right shunt where blood moves from the systemic circulation to the pulmonary circulation.
Risk factors
Risk factors for a patent ductus arteriosus include:
- Prematurity
- Low birth weight
- Other congenital heart defects
- Difficulty at delivery: hyaline membrane disease, sepsis
Clinical features
History
The clinical presentation of a patent ductus arteriosus depends upon the duct’s size and the patient’s gestational age.
With a large PDA, there may be a history suggestive of heart failure (due to left-to-right shunting of blood), including:
- Poor feeding
- Failure to thrive
- Respiratory distress with tachypnoea and dyspnoea. In premature infants, this may present with an increase in ventilator requirements.
Premature infants can also develop necrotising enterocolitis associated with a patent ductus arteriosus.
These symptoms are likely to occur earlier and be more severe in a premature infant than in a term infant.
Clinical examination
Clinical examination findings differ depending on the size of the PDA. A small PDA may not be audible on examination and have no clinical signs.
Typical clinical findings on cardiovascular examination may include:
- Wide pulse pressure
- Bounding pulses with a dynamic precordium
- Grade 1-3 continuous machinery murmur heard loudest at the left upper sternal edge
Differential diagnoses
Possible differential diagnoses of a patent ductus arteriosus include other congenital heart defects which may be associated with PDA or arise independently.
Investigations
Bedside investigations
Relevant bedside investigations include:
- ECG: may be normal with a small PDA; left ventricular hypertrophy can occur with large PDAs
Imaging investigations
Relevant imaging investigations include:
- Echocardiogram: will demonstrate the PDA and assess other parameters, including size, flow, and associated abnormalities
- Chest X-ray: with a small PDA, this may be normal. With a large PDA, there may be evidence of volume overload and prominence of the left atrium and ventricle
Management
Management depends on the size of the PDA and its impact on the infant.
Medical management
Some infants will outgrow the PDA. Fluid restriction and diuretics are used to manage the symptoms while this happens.
Ibuprofen, indomethacin, and paracetamol have all been used to reduce prostaglandins and close a patent ductus arteriosus. This is used when the infant is haemodynamically compromised by the PDA.
Surgical management
Surgical closure of a patent ductus arteriosus may be considered in severe cases and is typically considered in larger and older infants.
Complications
If a PDA is large and not managed appropriately, complications include:2
- Respiratory failure
- Cardiac failure
- Pulmonary vascular disease
- Necrotising enterocolitis
- Failure to thrive
Haemodynamically significant PDAs are associated with significant morbidity and mortality (up to 30%), often from complications.
Key points
- A PDA is a remnant of the fetal circulation and accounts for up to 10% of all cases of congenital heart disease
- The major risk factor for a PDA is prematurity
- A PDA murmur presents as a continuous machinery murmur loudest at the left upper sternal edge and is associated with bounding pulses
- PDA may be managed conservatively with fluid and diuretics, indomethacin, or surgical closure
- Complications include cardiac failure, pulmonary vascular disease and failure to thrive
Editor
Dr Chris Jefferies
References
- Clyman R. Ibuprofen and Patent Ductus Arteriosus. September 2000. Available from: [LINK]
- Dice and Bhatia. Patent Ductus Arteriosus: An Overview. Jul-Sep 2007. Available from: [LINK]