- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
An acute ST-elevation myocardial infarction (STEMI) is a clinical event characterised by transmural myocardial ischaemia resulting in myocardial injury or necrosis. It is one of three types of acute coronary syndrome. The other forms include unstable angina and non-ST-elevation myocardial infarction (NSTEMI).
The diagnosis of STEMI requires the presence of acute anginal chest pain and ST elevation on an electrocardiogram. Elevated biomarkers such as troponin do not contribute to diagnosing a STEMI.
Aetiology
A STEMI is caused predominantly by complete occlusion of one or more coronary arteries that supply the heart, usually due to a thrombus. A thrombus is mostly made up of aggregated platelets and thrombin.
The disruption of blood flow to the coronary artery reduces oxygen perfusion, which can involve the myocardium’s full thickness, resulting in a transmural infarction.
Risk factors
Risk factors for STEMI include any cardiac risk factors which increase the risk of coronary artery atherosclerosis.
Non-modifiable risk factors include:
- Male sex
- Older age
- Previous history of ACS/ischaemic heart disease
- Family history of ACS/ischaemia heart disease
- Renal insufficiency
- Diabetes
Modifiable risk factors include:
- Smoking
- Longstanding hypertension
- Hyperlipidaemia
- Obesity & sedentary lifestyle
Clinical features
History
Initial assessment of anyone with acute chest pain involves a thorough history. For more information, see the Geeky Medics guide to chest pain history taking.
Typical features of cardiac chest pain include:
- Site: central or left-sided chest pain (usually lasting > 15 minutes)
- Onset: “crescendo pain” with increasing severity over several minutes
- Character: described as substernal pressure, heaviness, squeezing, and aching
- Radiation: left arm, shoulders, neck, or jaw
- Severity: variable, can range from 1 to 10 out of 10
Associated symptoms may include sweating, nausea, vomiting, dyspnoea, fatigue and/or palpitations.
Clinical examination
All patients with suspected ACS require a comprehensive cardiovascular examination. However, examination findings can be non-specific in a STEMI.
Examination findings can vary significantly and may reflect complications such as left ventricular failure or ventricular septal rupture:
- Hypotension or hypertension may occur depending on the extent of the myocardial infarction
- Low-grade fever
- Pale, cool and/or clammy skin
- Signs of acute heart failure: tachycardia, gallop rhythm, third and fourth heart sounds, bibasal crackles, peripheral oedema, elevated jugular venous pressure and/or tender hepatomegaly
- Systolic murmur due to acute mitral regurgitation or ventricular septal rupture and/or pericardial rub
Differential diagnoses
Chest pain has a wide range of potential causes. Differential diagnoses to consider in the context of acute chest pain include:
- Cardiovascular: other forms of ACS (unstable angina or NSTEMI), acute pericarditis, myocarditis, aortic stenosis, aortic dissection
- Respiratory: pulmonary embolism, pneumonia, pneumothorax
- Gastrointestinal: oesophageal spasm, oesophageal rupture, GORD, acute gastritis, cholecystitis, acute pancreatitis
- Musculoskeletal: costochondritis
Investigations
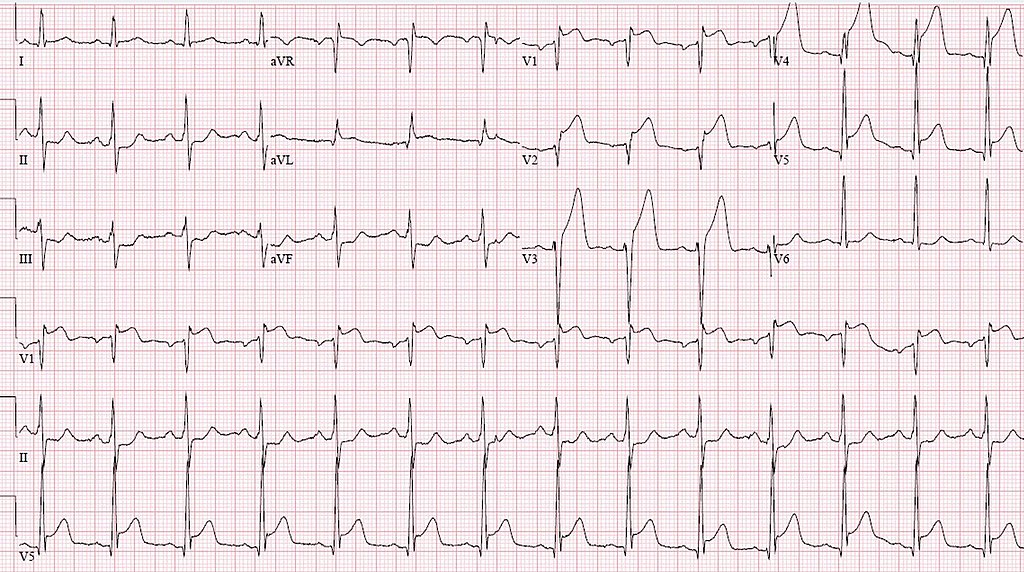
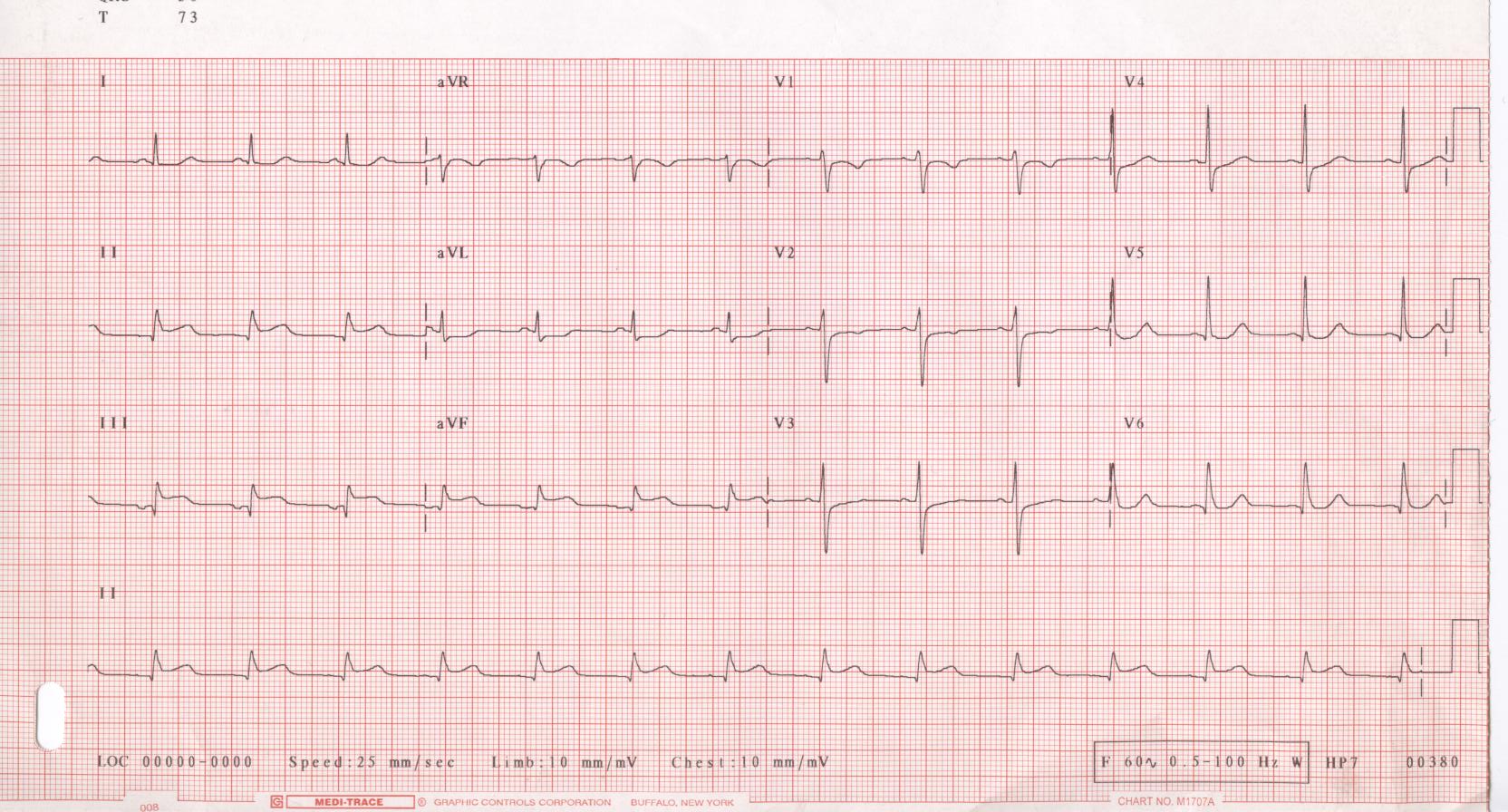
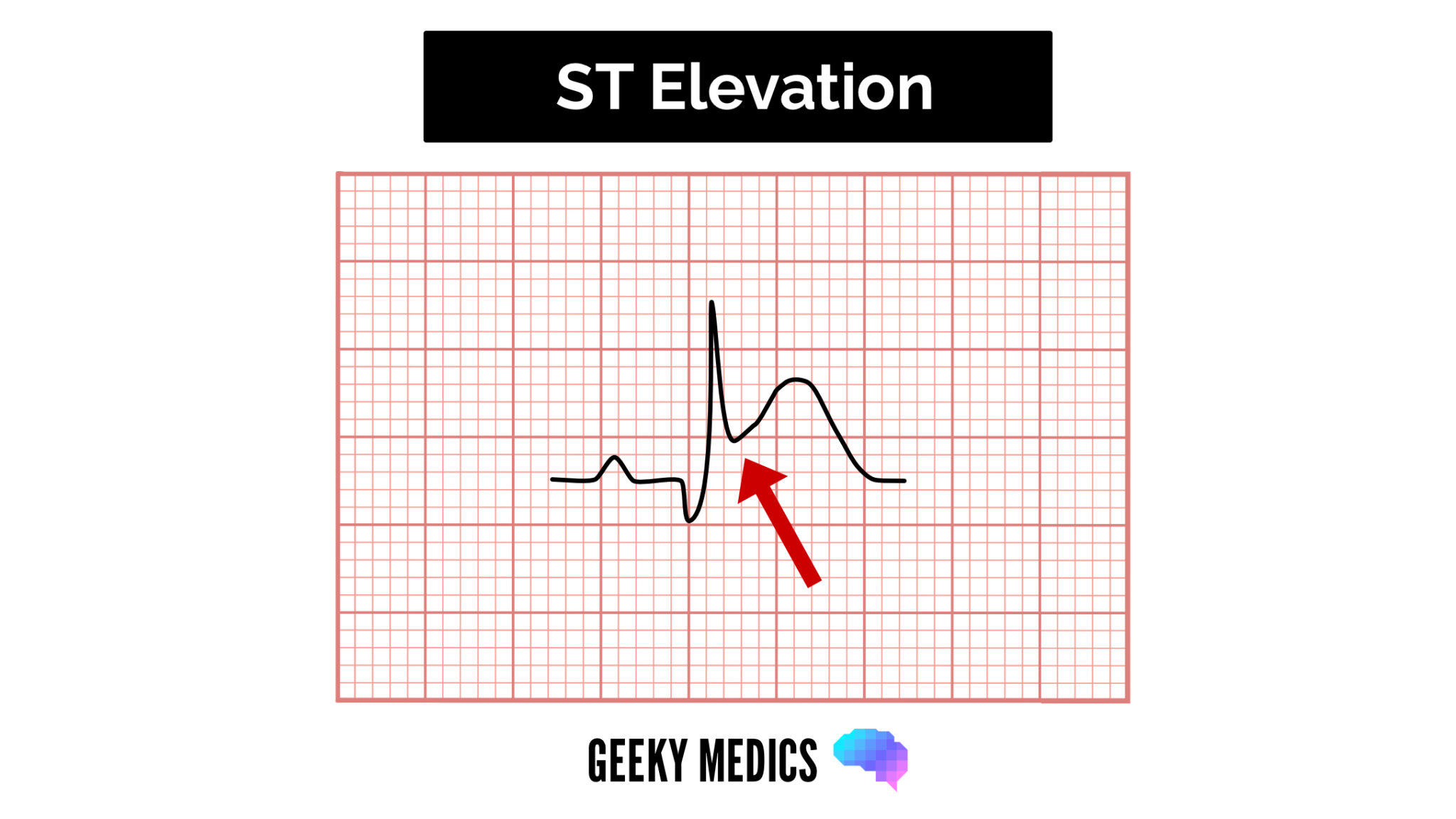
The most important investigation in the context of ACS is a 12-lead ECG. The diagnosis of STEMI requires the presence of acute anginal chest pain and ST elevation on an ECG.
Other investigations (including troponin) do not contribute to diagnosing a STEMI. However, these investigations may identify complications (e.g. signs of heart failure on a chest X-ray) or help guide management.
Bedside investigations
When ACS is suspected, a 12-lead ECG should be acquired and interpreted within 10 minutes or as soon as possible.
In the proper clinical context, a STEMI is diagnosed when there is a new and persistent ST-segment elevation in at least two contiguous leads of ≥1mm in all leads except V2-V3 with the following cut-off points:
- ≥2.5 mm in men <40
- ≥2 mm in men >40
- ≥ 1.5 mm in women regardless of age
1mm = 1 small square (in a standard ECG strip)
It’s important to consider patients with left bundle branch block (LBBB) can mimic acute ischemia and should be further evaluated using Sgarbossa’s criteria.
Contiguous ECG leads lie next to each other anatomically and indicate specific vascular territory. Because of the variability of individual coronary anatomy, these patterns are generalisations and not hard and fast rules.
- Left anterior descending (LAD) occlusion produces ST elevation in the precordial leads (V1-3)
- Right coronary artery (RCA) occlusions produce ST changes in the inferior leads (II-III-AVF)
- Left circumflex artery (LCA) occlusions produce ST elevation in the lateral leads (I, AVL and V5-6)
See the Geeky Medics guides to ECG interpretation for more information.
Laboratory investigations
Relevant laboratory investigations include:
- Troponin
- Full blood count: check for anaemia
- Urea & electrolytes: renal function may affect treatment options, and chronic kidney disease is a risk factor for cardiovascular disease
- Liver function tests
- Lipid profile
- Thyroid function tests: check for hypo/hyperthyroidism
- HbA1C and glucose: hyperglycaemia is common in ACS and associated with worse outcomes
Troponin
Troponin is released from ischaemic muscle. Cardiac troponins T and I are highly sensitive and specific for myocardial damage. Serum levels increase within 3-12 hours from the onset of chest pain, peak at 24-48 hours, and can remain high for up to 14 days in the presence of normal creatine clearance.
Other cardiac enzymes (e.g. CK-MB) increase within 3-12 hours of the onset of chest pain. However, these are not routinely measured since sensitivity and specificity are not as high.
ACS is not the only cause of a raised troponin, and troponin levels must be interpreted in the clinical context. Other causes of raised troponins include:
- Tachy/bradyarrhythmias
- Aortic dissection
- Heart failure
- Myocarditis
- Chronic kidney disease
- Sepsis
Imaging
Relevant imaging investigations include:
- Chest X-ray: to identify other causes of chest pain and pulmonary oedema
Management
STEMI is an emergency situation, and an initial ABCDE approach should be taken.
All patients should be placed on continuous monitoring (including ECG, pulse, blood pressure, and oxygen saturation) to identify life-threatening arrhythmias (e.g. ventricular fibrillation or tachycardia).
Arranging rapid reperfusion therapy is essential to reduce further ischaemic cardiac injury and avoid complications.
Immediate management
Immediate management of STEMI includes:
- Analgesia
- Loading dose (300mg) of aspirin
- Oxygen if SpO2 <94%
MONA
MONA is a mnemonic for the initial management of a STEMI.
- Morphine
- Oxygen (saturations under 94%)
- Nitrates
- Aspirin (300mg loading dose)
Reperfusion therapy
The NICE guidelines advise that patients with a STEMI presenting within 12 hours of the onset of symptoms should be discussed urgently for either:
- Primary percutaneous coronary intervention (if available <120 minutes of presentation)
- Thrombolysis (if PCI is not possible within 120 minutes)
The current gold standard treatment option is primary percutaneous intervention (PCI) to allow the vessel to be opened as quickly as possible, as ‘time is muscle’.
Primary percutaneous coronary intervention
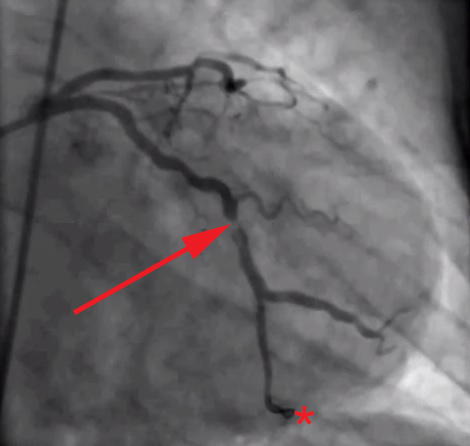
Percutaneous coronary intervention (PCI) involves catheterising the patient’s radial or femoral artery and feeding up a guide wire to the coronary arteries under X-ray guidance.
Contrast is injected to identify the occlusion, which can be opened with a balloon. A stent is placed to maintain artery patency. Aspiration of the thrombus can be performed in selected cases.
Thrombolysis
Thrombolysis involves injecting a fibrinolytic medication to dissolve thrombi rapidly. Some examples of thrombolytic agents include streptokinase, alteplase and tenecteplase.
However, this has significant bleeding risks and often fails to open the artery up, requiring the patient to undergo ‘rescue angioplasty’ with higher bleeding risks.
Secondary prevention
All patients diagnosed with acute coronary syndrome require long-term management and prevention strategies.
The following medications are recommended to reduce the risk of future events (secondary prevention) and improve myocardial function:
- ACE inhibitor or ARB: continued indefinitely
- Dual antiplatelet therapy (aspirin plus a second agent): for up to 12 months
- Beta-blocker for at least 12 months: continued indefinitely in the presence of reduced left ventricular ejection fraction
- Statin: continued indefinitely
Cardiac rehabilitation should be offered to all patients:
- Advice on lifestyle, driving, flying and sex
- Tailored physical activity
- Stress management
- Health and lifestyle education
Complications
Complications of a STEMI include:
- Tachyarrhythmias: sinus tachycardia, atrial fibrillation, atrial flutter, ventricular tachycardia and/or fibrillation (mono/polymorphic ectopic)
- Bradyarrhythmias: sinus bradycardia, atrioventricular blocks, atrial flutter/fibrillation with slow ventricular response
- Re-infarction or infarct extension: most common in the initial few days
- Ventricular free-wall/septal rupture
- Acute mitral regurgitation
- Left ventricular aneurysm
- Stent thrombosis following PCI
- Bleeding (e.g. intracranial, gastrointestinal) following thrombolysis
- Pericarditis (Dressler’s syndrome)
- Depression
Prognostic factors
The following features are associated with a worse prognosis:
- Greater severity of myocardial necrosis (based on serum troponin, ECG changes and degree of LV dysfunction on echocardiography)
- Site of the infarction: anterior myocardial infarction generally has a less favourable prognosis than inferior myocardial infarction
- Delayed reperfusion with short-term and long-term treatment
- Comorbidities (e.g. hypertension, chronic kidney disease, anaemia and diabetes mellitus)
- Older age
Key points
- A STEMI is a form of acute coronary syndrome diagnosed by chest pain and ST elevation on an ECG
- The cause is due to an occlusion of a coronary artery resulting in transmural myocardial ischaemia
- A STEMI usually presents with cardiac chest pain with or without associated symptoms (e.g. nausea)
- The most important investigation in the context of suspected ACS is a 12-lead ECG
- Management of a STEMI requires initial stabilisation (ABCDE approach), antiplatelets and reperfusion therapy (PCI vs thrombolysis)
- Complications may include cardiogenic shock, arrhythmias and heart block
Reviewer
Dr Abubakr Khalil
Consultant Cardiologist
Altnagelvin Hospital, Londonderry
Editor
Dr Chris Jefferies
References
- NICE. Acute coronary syndromes. 2020. Available from: [LINK]
- BMJ Best Practice. Overview of Acute Coronary Syndrome. 2022. Available from: [LINK]
- de Luna, A. B., Fiol-Sala, M., & Antman, E. M. (2008). The 12 lead ECG in ST elevation myocardial infarction: a practical approach for clinicians. John Wiley & Sons.
- Watson, T. J., Ong, P. J., & Tcheng, J. E. (2018). Primary angioplasty: a practical guide.
- Albarran, J., & Tagney, J. (Eds.). (2008). Chest Pain: Advanced Assessment and Management Skills. John Wiley & Sons.
Image references
- Figure 1. Various authors. ST elevation myocardial infarction ECG (cropped). License: [CC BY]
- Figure 2. Glenlarson. ECG 001. License: [CC BY-SA]
- Figure 3. Todt T, Maret E, Alfredsson J, Janzon M, Engvall J, Swahn E. Coronary angiography of a STEMI patient, showing partial occlusion of left circumflex coronary artery. License: [CC BY]