- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
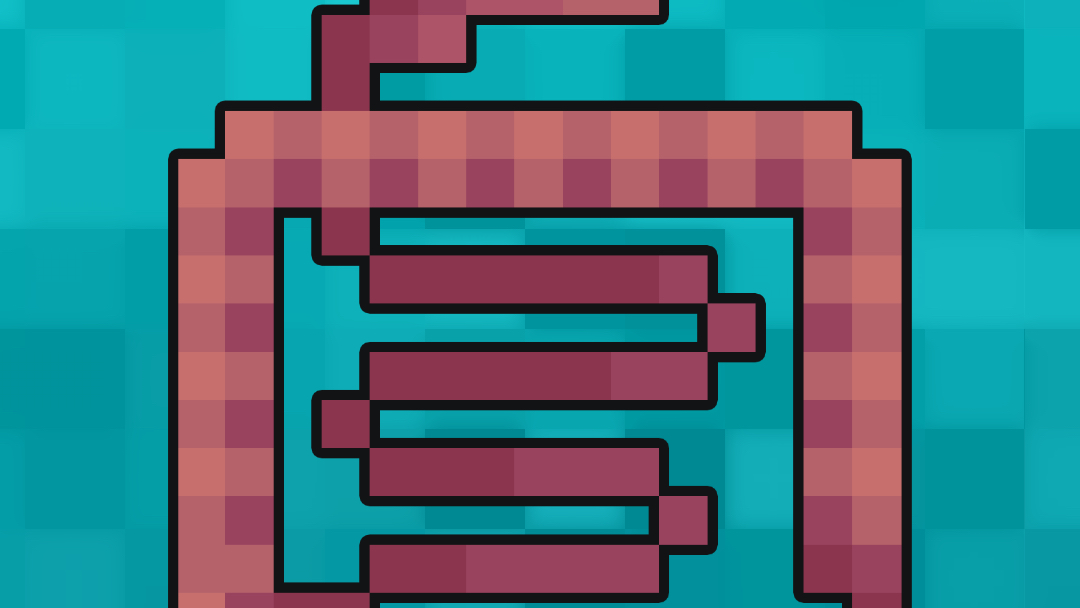
The small intestine is the primary digestive organ of the gastrointestinal tract and has an important role in aiding digestion and absorption of chyme received from the stomach.
Functions of the small intestine include chemical digestion of proteins, lipids and carbohydrates using enzymes to break down chyme into a form that can be absorbed in the small intestine across epithelial cells via simple and facilitated diffusion, and active transport.
The small intestine extends from the pylorus of the stomach to the ileocaecal junction where it meets the large intestine at the ileocaecal valve.1
The small intestine can be split into three structural parts: duodenum, jejunum, and ileum.
The first part of the duodenum, jejunum and ileum are found intraperitoneally. The jejunum and ileum are suspended by mesentery which is part of the peritoneum and contains the blood vessels and nerves.
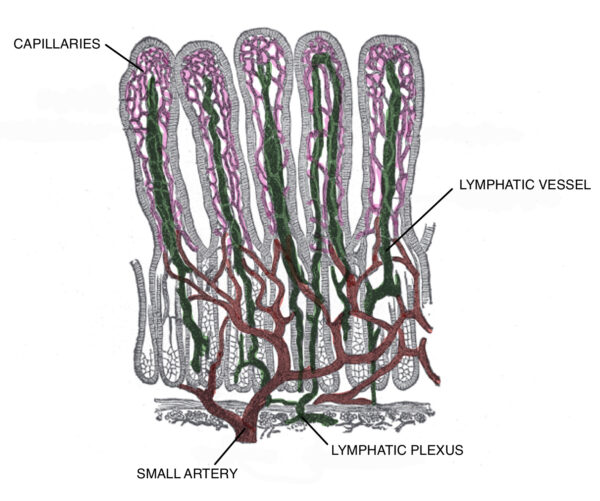
The small intestine contains valvulae conniventes which are large mucosal circular folds that project into the lumen of the small intestine. The valvulae conniventes occur around 2.5-5 cm below the pylorus of the stomach within the duodenum and are important in increasing the surface area of absorption.
Clinical relevance: Radiological appearance of the small intestine
On abdominal X-ray (AXR), the diameter should not normally exceed:
- 3 cm for the small intestine
- 6 cm for the large intestine
- 9 cm for the caecum
This is referred to as the 3/6/9 rule. The presence of a wider diameter is suggestive of small bowel obstruction.2,3
The most common cause of small bowel obstruction is adhesions which are usually related to previous abdominal surgery. Other causes include abdominal hernias and compression by neoplastic masses within the intestinal lumen or from the abdominal cavity.4
Duodenum
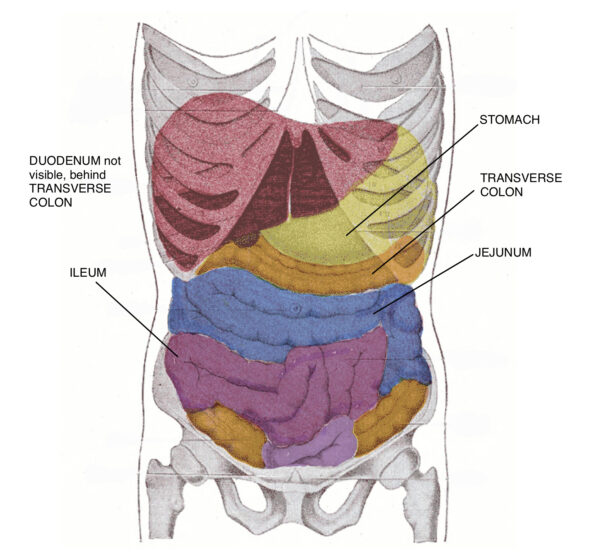
The duodenum is the shortest part of the small intestines, approximately 20-25 cm in length. It is shaped like a ‘C’ where it surrounds the head of the pancreas.
The duodenum can be further separated into four sections:
- Superior: intraperitoneal and freely mobile
- Descending: receives bile duct and main pancreatic duct via major duodenal papilla and accessory pancreatic ducts via minor duodenal papilla
- Horizontal: runs across the body of the L3 vertebra
- Ascending: runs alongside the abdominal aorta before terminating ventrally at the duodenojejunal flexure
Clinical relevance: Duodenal ulceration
Duodenal ulcers can develop secondary to NSAIDs or infection with Helicobacter pylori.
Symptoms include upper abdominal pain that is typically relieved by eating. In contrast, gastric ulceration tends to present with pain that worsens after eating.4
Acute complications of duodenal ulceration depend on the anatomical location of the ulcer:1
- Anterior: the ulcer may erode into the peritoneal cavity, causing peritonitis
- Posterior: the ulcer may erode into blood vessels, such as the gastroduodenal artery resulting in massive haemorrhage
Histology
The duodenum features a simple columnar intestinal epithelium which contains goblet cells and Paneth cells. Only the duodenum contains Brunner’s glands which are important in producing alkaline mucous to neutralise acidic chyme from the stomach and in optimising the activity of intestinal enzymes for absorption.
The separation between the duodenum and jejunum is marked by the suspensory muscle of the duodenum (ligament of Treitz), which fixes the duodenojejunal flexure to the right crus of the diaphragm. This is particularly important when diagnosing incomplete rotation or malrotation on a radiological scan.
Jejunum
The jejunum is located between the duodenum and ileum.
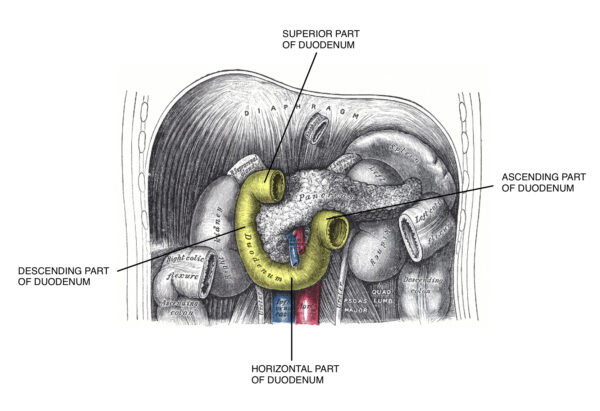
The structure of the jejunum is different to the duodenum as it is longer (approximately 2.5m) and contains plicae circulares and villi which increases the absorption of sugars, amino acids, and fatty acids (products of digestion).
Histology
The histology of the jejunum is similar to the duodenum, however, it does not contain Brunner’s glands. In addition, it does not contain Peyer’s patches which are present in the ileum only.
Ileum
The ileum is similar in structure to the jejunum and is the longest portion of the small intestine, being around 3 metres long.
The main function of the ileum is to absorb vitamin B12 and bile acids. The ileum joins the first part of the large intestine, the cecum, at the ileocaecal junction.
Histology
The ileum can be differentiated from duodenum and jejunum by the presence of Peyer’s patches. These are lymphoid follicles located in the mucosa layer and extend into the submucosa layer.
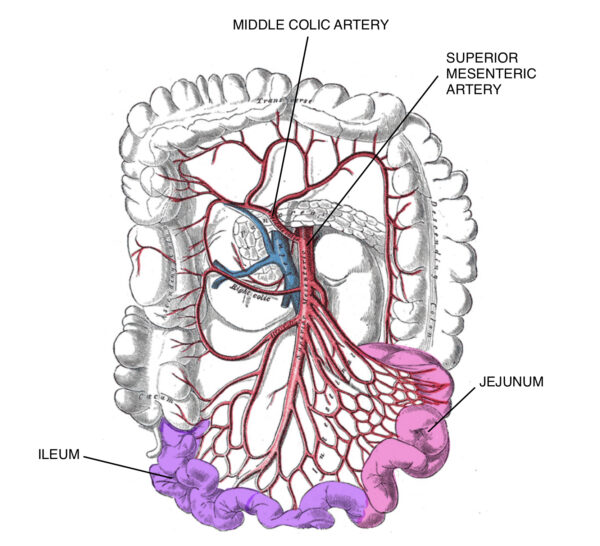
Arterial supply
Blood supply to the small intestine arises from the celiac trunk and superior mesenteric artery which are direct branches from the abdominal aorta.
The duodenum receives blood supply from both the coeliac trunk via the superior pancreaticoduodenal artery and from the superior mesenteric artery via the inferior pancreaticoduodenal artery due to embryonic gut derivatives from the foregut and midgut.
The foregut comprises the distal oesophagus to the proximal half of the second part of the duodenum. The midgut continues from the distal half of the second part of the duodenum down to the proximal 2/3 of the transverse colon.
The jejunum and ileum receive blood supply from the superior mesentery artery which forms arterial arcades within the mesentery. The vasa recta, the straight blood vessels from the arcade, supply the organs directly.1
Clinical relevance: Acute mesenteric ischaemia
Acute mesenteric ischaemia occurs when there is insufficient blood supply to the small intestine.
Acute mesenteric ischemia is a medical emergency that typically presents with severe generalised abdominal pain associated with nausea and vomiting. The condition has a high mortality rate and requires urgent revascularisation of the intestine and resection of any necrotic bowel.6
Venous and lymphatic drainage
Table 1. The venous and lymphatic drainage of the small intestine.
| Location | Venous drainage | Lymphatic drainage |
|
Duodenum |
Duodenal veins drain into pancreaticoduodenal veins where they merge into the superior mesenteric vein and common hepatic vein.
|
Drain into pancreaticoduodenal nodes, pyloric nodes, superior mesenteric nodes, and celiac lymph nodes. |
|
Jejunum and ileum |
Drains into venous arcades which drains into the superior mesenteric vein which goes on to form portal vein by merging with the splenic vein.
|
Travels in mesentery into mesenteric lymph nodes and then into superior mesenteric nodes or ileocolic nodes. This drains into cisterna chyli. |
Key points
- The small intestine is the primary digestive organ of the gastrointestinal tract.
- The three sections of the small intestine are the duodenum, jejunum and ileum.
- The small intestine is lined by simple columnar intestinal epithelium with each section of the small bowel having distinctive features (duodenum has Brunner’s gland, ileum has Peyer’s patches).
- The duodenum is found in the epigastric region surrounding the head of the pancreas and is split into four parts.
- The jejunum contains plicae circulares and villi which increase the absorption of products of digestion.
- The ileum is important in absorbing vitamin B12 and bile acids.
- The arterial supply of the small intestine is from the coeliac trunk and superior mesenteric artery.
Editor
Dr Chris Jefferies
References
- Gray’s Anatomy for Students, Third Edition.
- Radiopaedia. Small Bowel. Revised in 2019. Available from: [LINK]
- Geeky Medics. Abdominal X-ray Interpretation. Available from: [LINK]
- BMJ Best Practice. Small bowel obstruction. Available from: [LINK]
- BMJ Best Practice. Peptic Ulcer Disease. Published in 2020. Available from: [LINK]
- BMJ Best Practice. Ischaemic bowel disease. Available from: [LINK]