- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
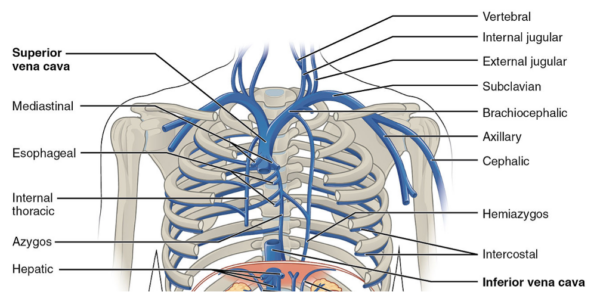
The superior vena cava (SVC) is a large vein that drains blood from the upper half of the body into the heart.
Overview of the superior vena cava
The superior vena cava transports blood from the head, neck, upper limbs and thorax into the right atrium.
The SVC is approximately 7cm long and does not have any valves. It is located in the right superior mediastinum. The SVC is formed by the right and left brachiocephalic veins joining together just behind the lower border of the first costal cartilage on the right.
Internal jugular and subclavian veins combine to create each brachiocephalic vein beneath the corresponding sternoclavicular joint.
Course of the SVC
The SVC begins below the lower border of the sternal end of the right first rib cartilage.
It then begins its descent straight behind the first and second intercostal spaces.
Before the SVC enters the pericardium, the azygos vein joins from the posterior aspect of the SVC at the level of T4. Several small pericardial veins, oesophageal veins and other contents of the mediastinum also drain into the SVC before it enters the pericardium.
The SVC enters the pericardium opposite the second right costal cartilage.
The SVC ends in the upper right atrium behind the third costal cartilage on the right.
The lower half of the SVC is located within the pericardium.
Through the course of the SVC, there is a slight curve towards the right side.
Anatomical relationships
Running on the left side of the SVC is the brachiocephalic artery and the ascending aorta. The ascending aorta and aortic arch overlap the SVC left laterally.
On the right side is the right phrenic nerve with accompanying vessels, the right pleura and the upper lobe of the right lung.
Posterior to the SVC lies the trachea, right vagus nerve and the root of the right lung. The right vagus nerve is located slightly to the left of the upper part of the SVC. The root of the right lung is found behind the lower part of the SVC.
Anterior to the SVC are the chest wall, thymus, internal thoracic vessels and the anterior margin of the right lung and pleura.
The portion of the SVC within the pericardium is covered by the serous layer of the pericardial membrane.
Tributaries of the superior vena cava
The tributaries of the SVC include:
- Azygous vein
- Minor veins: mediastinal veins, pericardial veins and oesophageal veins
The azygous vein travels over the root of the right lung and at the level of the second costal cartilage opens up into the SVC, just before it enters the pericardium.
The lumbar azygous, right subcostal and right ascending lumbar veins come together to form the azygous vein. The azygous vein drains the upper lumbar region and the right thoracic wall. It creates a canal which joins the superior and inferior vena cava.
Clinical relevance: SVC syndrome
Obstruction of the SVC causes SVC syndrome. The SVC is vulnerable to obstruction, with malignancy being the most frequent cause (especially non-small cell lung cancer).
Thrombotic causes of SVC syndrome are becoming more common due to the rise in the use of pacemakers and central venous catheters.
Clinical features of SVC syndrome include oedema of the head, neck, and arms due to elevated venous pressure in the upper body. Other signs include cyanosis, plethora, and dilated neck vessels. Pemberton’s sign is used to describe when these features occur when both arms are raised at the same time.
Oedema can damage the function of the larynx or pharynx leading to coughing, hoarseness, dyspnoea, stridor, and dysphagia. Headache, disorientation, and coma are symptoms of cerebral oedema.
Reviewer
Dr Matthew Tan
Vascular Clinical Research Fellow
Editor
Dr Chris Jefferies
References
Text references
- Sinnatamby CS. Last’s Anatomy, 12th Edition. Published in 2011.
- Snell RS. Clinical Anatomy by Regions, 9th Edition. Published in 2011.
- Chaurasia BD. Human Anatomy, Volume 1, 8th Edition, Published in 2019
- H Gray. Anatomy of the Human Body, 41st edition. Published in 2015
- Cohen R, Mena D, Carbajal-Mendoza R, Matos N, Karki N. Superior vena cava syndrome: A medical emergency? International Journal of Angiology 2008 17(01):43–6
- Wilson LD, Detterbeck FC, Yahalom J. Superior Vena Cava Syndrome with Malignant Causes. New England Journal of Medicine 2007 356(18):1862–9
- Kapoor S, Paik E, Rezaei E, Vu Where There Is Blood, There Is a Way: Unusual Collateral Vessels in Superior and Inferior Vena Cava Obstruction. RadioGraphics 2010 30:1, 67-78
- Lepper PM, Ott SR, Hoppe H, Schumann C, Stammberger U, Bugalho A. Superior Vena Cava Syndrome in Thoracic Malignancies. Respiratory Care 2011 56(5):653–66.
Image references
- Figure 1. Anatomy & Physiology. Thoracic Abdominal Veins. June 2013, Licence: [CC-BY-SA]




