- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
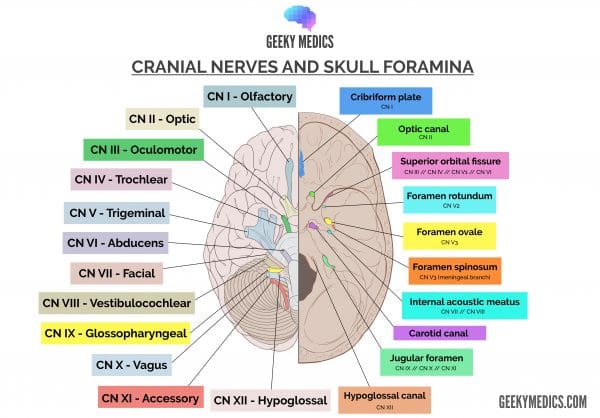
Cranial nerve X is the vagus nerve. The literal translation is “wandering” as it takes a wandering course from the skull to the abdominal cavity. The vagus nerve supplies sensory, special sensory, motor and parasympathetic innervation to structures of the head, neck and thoracoabdominal cavity.
First, we will discuss the embryology of the vagus nerve, followed by the structure, function and clinical relevance of this fascinating nerve.
Check out our summary of the cranial nerves here.
You can also check out our cranial nerve anatomy quiz here.
Embryology of the vagus nerve
The vagus nerve is associated with two pharyngeal arches: the fourth and sixth.
Structures derived from the fourth pharyngeal arch include:
- Bones and soft tissue: thyroid and epiglottic cartilages
- Muscles: cricothyroideus and soft palate muscles (excluding tensor veli palatini)
- Nerve: the superior laryngeal branch of the vagus nerve
Structures derived from the sixth pharyngeal arch include:
- Bones and soft tissue: cricoid, arytenoid, corniculate, cuneiform cartilages
- Muscles: all intrinsic laryngeal muscles except cricothyroideus
- Nerve: the recurrent laryngeal branch of the vagus nerve
Having two separate pharyngeal arches develop with independent nervous supply is important, as it allows functional control of phonation and swallowing.
Nuclei of the vagus nerve
The vagus nerve has numerous functions, each derived from different nuclei in the medulla oblongata and pons. We have broken this down simply into the functional classification described below:
- Parasympathetic: dorsal motor nucleus
- Motor: nucleus ambiguus (also parasympathetic to the heart)
- Special sense: solitary nucleus
- Sensory (crude touch, pain and temperature): spinal trigeminal nucleus
Intracranial vagus nerve
Arising from these four nuclei, the fibres of the vagus nerve converge to exit the medulla at the post-olivary sulcus. Superior to this point of exit lies the glossopharyngeal nerve (CN IX); and inferiorly lies the spinal accessory nerve (CN XI).
The vagus nerve then moves inferolaterally with CNs IX and XI to enter the jugular foramen.
Extracranial vagus nerve: head
Upon exiting the jugular foramen, an auricular branch is given off, supplying somatic sensation to the posterior external auditory canal and external ear. This is the only branch of the vagus nerve given to the head.
Extracranial vagus nerve: neck
As the vagus nerve continues to course down the neck, it travels in the carotid sheath, posterior to the common carotid artery and internal jugular vein.
The following branches leave the vagus nerve as it descends the neck (superior to inferior).
Pharyngeal branches
Supplies motor innervation to most of the soft palate and pharynx.
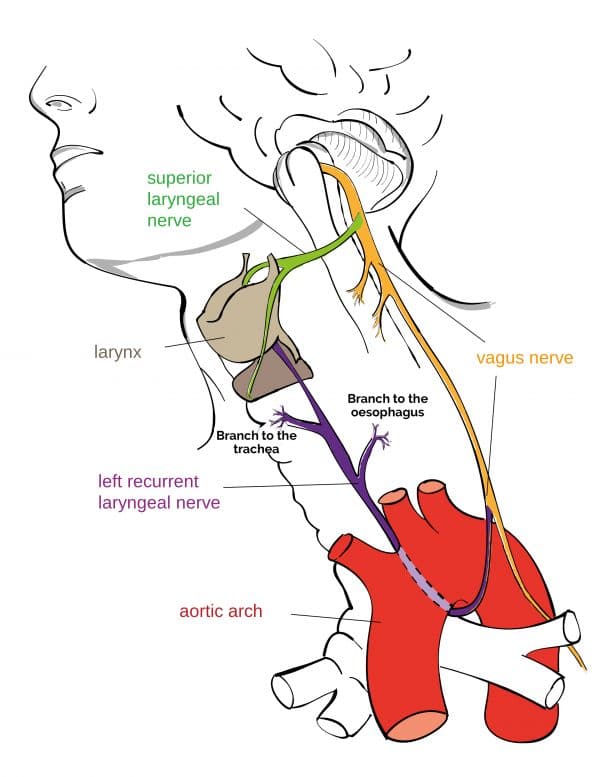
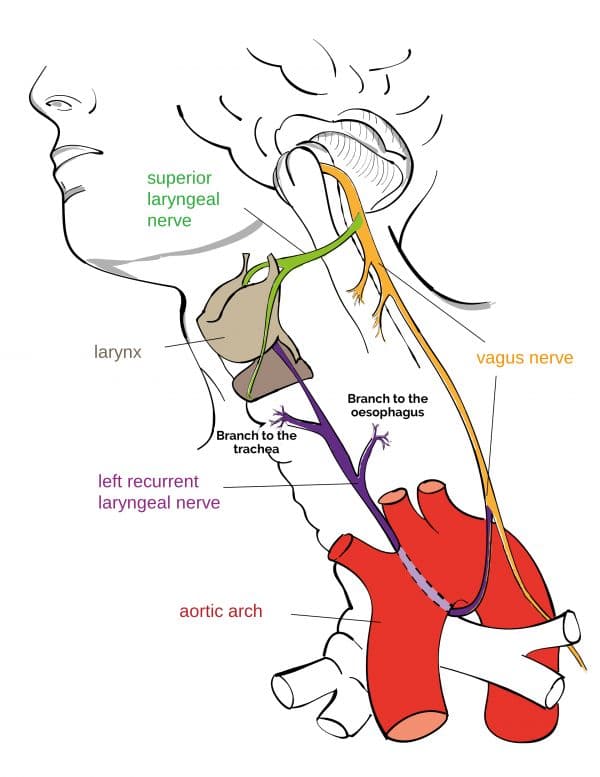
Superior laryngeal nerve
Two branches:
- Internal branch: sensory innervation to thelaryngopharynx and superior larynx (including taste to the epiglottis)
- External branch: motor innervation to the cricothyroideus muscle
Right recurrent laryngeal nerve (branches from the vagus in the neck)
Loops under the right subclavian artery and ascends to the larynx. Provides motor innervation to most laryngeal muscles.
Clinical relevance: vagus nerve examination
The vagus nerve has many functions, but we really only test one of these: the efferent (motor) limb of the cough or gag reflexes.
By stimulating the oropharynx with a long cotton tip, the efferent limb of the gag reflex causes the muscles of the pharynx to gag in an attempt to rid this region of the foreign object. During coughing, the vagus nerve provides motor input to roughly the same muscles to constrict the pharynx and allow high velocity, forceful coughing.
Extracranial vagus nerve: thorax
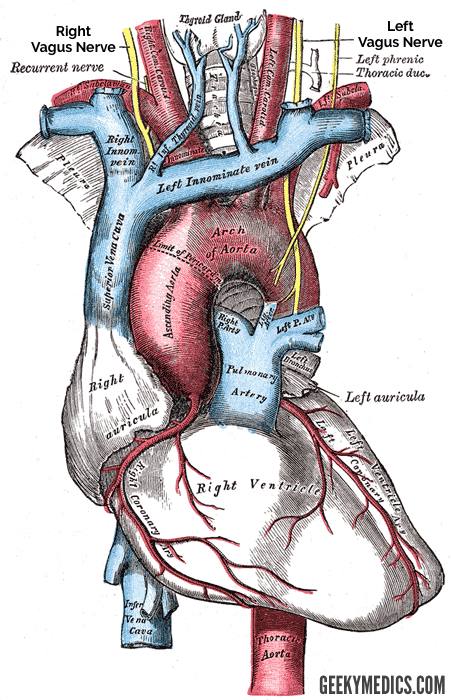
Towards the base of the neck, both the left and right vagus nerves take different paths.
Left vagus nerve
The left vagus nerve passes between the left common carotid artery and the left subclavian artery. It then enters the thorax posterior to the sternoclavicular joint and forms the anterior vagal trunk.
Right vagus nerve
The right vagus nerve passes anterior to the right subclavian artery. It enters the thorax posterior to the sternoclavicular joint and forms the posterior vagal trunk.
Anterior and posterior vagal trunks
Branches from the vagal trunk contribute to the oesophageal plexus, supplying motor innervation to this muscular structure.
In the thorax, two branches arise from the anterior and posterior vagal trunks.
Left recurrent laryngeal nerve (branches from the anterior vagal trunk in the thorax)
The left recurrent laryngeal nerve loops under the arch of the aorta and ascends into the larynx. It provides motor innervation to intrinsic laryngeal muscles.
Cardiac branches
The cardiac branches provide parasympathetic and visceral innervation to the heart.
Clinical relevance: refractory tachycardia
We also know that the vagus nerve supplies the sinoatrial and atrioventricular nodes of the heart with parasympathetic innervation. Patients who lose vagal tone may lose the parasympathetic tone in these regions, allowing uncontrolled sympathetic activity presenting as a refractory tachycardia. While quite rare, keep this in the back of your mind!
Extracranial vagus nerve: abdomen
Both the left and right vagal trunk enter the abdomen through the oesophageal hiatus at the vertebral level of T10.
In the abdomen, the vagus nerve terminates as many parasympathetic and sensory branches supplying the oesophagus, stomach, small intestine, and the proximal 2/3 of the colon.
Key points
- CN X is the vagus nerve
- It originates in the medulla oblongata
- Its major role is parasympathetic innervation of the viscera
- The recurrent laryngeal nerve loops under the right subclavian artery and (left) aortic arch
- It passes through the jugular foramen with CN IX and XI
- It provides many fibre types, each of which are shown in the table below
| General somatic afferent | Special visceral afferent | General visceral afferent | General visceral efferent | Special visceral efferent |
| Skin around ear | Taste and sensation to the epiglottis | Sensory information to body viscera | Parasympathetic to glands of GI tract | Motor innervation to soft palate, pharynx and larynx |
References
Reference texts
- Sinnatamby, C. S. (2011). Last’s Anatomy, International Edition: Regional and Applied. Elsevier Health Sciences.
- Moore, K. L., Dalley, A. F., & Agur, A. M. (2013). Clinically oriented anatomy. Lippincott Williams & Wilkins.
- Nolte, J. (2002). The human brain: an introduction to its functional anatomy.
- Snell, R. S. (2010). Clinical neuroanatomy. Lippincott Williams & Wilkins.
Reference images
- Patrick J. Lynch. License: [CC BY]. Modified by Dr Lewis Potter.
- Henry Vandyke Carter. License: [Public domain]
- Jkwchui. License: [CC BY-SA]