- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
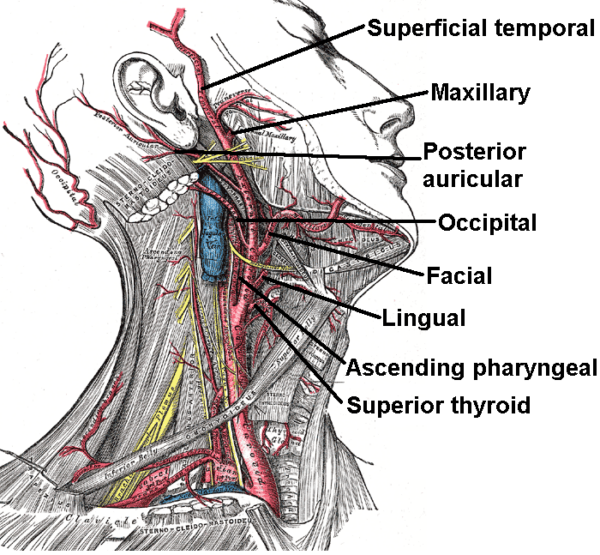
This article will cover the anatomy of the external carotid artery, including a description of its branches and relations with surrounding structures.
Overview of the external carotid artery
The external carotid artery (ECA) is one of the two main divisions of the common carotid artery.
The common carotid artery arises from the aortic arch on the left and the brachiocephalic trunk on the right.
The common carotid arteries ascend the neck bilaterally and bifurcate at the level of the thyroid cartilage, dividing into the internal carotid artery and the external carotid artery.
The internal carotid artery enters the cranial cavity via the carotid canal. In contrast, the external carotid artery ascends in the lateral neck within the carotid sheath, eventually supplying blood to the neck, head, and face areas.
The course of the external carotid artery
The external carotid artery originates from the bifurcation of the common carotid artery at the level of the thyroid cartilage.
The external carotid artery’s size diminishes as it courses superiorly and gives off five branches along its journey before terminating at the parotid gland with its last two branches: the maxillary artery and the superficial temporal artery.
Anatomical borders
Anterior
- Sternocleidomastoid muscle
- The platysma muscle
- Deep cervical fascia
- Superficial fascia
- Skin
Medial
- Hyoid bone
- Wall of the pharynx
- Superior laryngeal nerve
- Parotid gland
Lateral
- Internal carotid artery
Posterior
- Superior laryngeal nerve
- Styloglossus muscle
- Stylopharyngeus muscle
- Glossopharyngeal nerve (CN IX)
- Pharyngeal branch of the vagus nerve (CN X)
- Parotid gland
Anatomical variants
Most variation of the ECA is with its branches. However, variations involving the location of the common carotid bifurcation have been documented, with it occurring as high as the hyoid bone and as low as the cricoid cartilage.
Branches of the external carotid artery
The external carotid artery divides into eight different branches:
- Superior thyroid artery
- Ascending pharyngeal artery
- Lingual artery
- Facial artery
- Occipital artery
- Posterior auricular artery
- Maxillary artery
- Superficial temporal artery
These can be remembered using the anatomy mnemonic: Some Anatomists Like Freaking Out Poor Medical Students.
Superior thyroid artery
Origin
Stems anteriorly from the external carotid artery at the level of the hyoid bone.
Course
Travels inferiorly towards the thyroid gland, parallel with the thyrohyoid muscle’s lateral border.
Divisions
- The glandular branches
- The infrahyoid (hyoid) branch
- The sternocleidomastoid branch
- The superior laryngeal artery
- The cricothyroid branch
Blood supply
The superior thyroid artery helps supply blood to the thyroid, muscles of the larynx, and muscles of the neck.
Anatomical variants
May originate at the carotid bifurcation or the common carotid artery.
Ascending pharyngeal artery
Origin
The medial side of the external carotid artery near the carotid bifurcation.
Course
Ascends vertically between the internal carotid artery and the pharynx until it reaches the undersurface of the base of the skull. It terminates when it anastomoses with the facial artery’s ascending palatine branch and the vertebral artery’s ascending cervical branch.
Divisions
- The pharyngeal trunk
- The neuromeningeal trunk
Blood supply
The ascending pharyngeal artery helps supply blood to the pharynx, palatine tonsils, eustachian tube, tympanic membrane, dura mater, and the hypoglossal (XII), glossopharyngeal (IX), and vagus (X) nerves.
Anatomical variants
May originate from the internal carotid or occipital artery.
Lingual artery
Origin
The anterior surface of the external carotid artery at the level of the C3 vertebrae.
Course
Ascends within the carotid triangle towards the hyoid bone before descending to form a loop crossed by the hypoglossal nerve (CN XII). Moving along the superior border of the hyoid bone, it then passes between the hyoglossus and middle pharyngeal constrictor muscle before turning upwards and bifurcating into the deep lingual and sublingual arteries.
Divisions
- The suprahyoid branch
- The dorsal lingual branch
- The deep lingual artery
- The sublingual artery
Blood supply
The lingual artery helps supply blood to the tongue, salivary glands, soft palate, palatine tonsils, and muscles attached to the hyoid bone.
Anatomical variants
May originate from the common carotid artery or a common trunk together with the facial and superior thyroid arteries.
Facial artery
Origin
Branches from the external carotid artery just above the lingual artery within the carotid triangle, beneath the ramus of the mandible.
Course
Travels beneath the digastric and stylohyoid muscles and deep to the submandibular gland. It then curves upwards over the mandible at the anteroinferior angle of the masseter, ascending as it moves anteriorly up the cheek until it reaches the corner of the mouth.
The facial artery then travels up in parallel with the lateral border of the nose until it terminates at the medial commissure of the eye with the angular artery branch.
Divisions
The cervical branch consists of:
- The ascending palatine artery
- The tonsillar artery
- The submental artery
- The glandular branches
The facial branch consists of:
- The inferior labial artery
- The superior labial artery
- The lateral nasal branch
- The angular artery
Blood supply
The facial artery helps supply blood to the muscles of the face, cervical lymph nodes, palatine tonsils, lips, and parts of the nose.
Anatomical variants
May arise from a common trunk together with the lingual artery to form the linguofacial trunk.
Occipital artery
Origin
Originates from the external carotid artery at the level of the posterior belly of the digastric muscle (just above the bifurcation of the common carotid artery).
Course
Passes posteriorly, parallel and deep to the posterior belly of the digastric muscle until it reaches the skull, where it passes in a groove on the temporal bone medial to the mastoid process. Accompanied by the greater occipital nerve, it pierces the deep cervical fascia between the trapezius and sternocleidomastoid muscles.
Upon reaching the scalp, it terminates by giving off several branches that travel across the surface of the occipitofrontalis muscle and anastomose with their contralateral counterparts. The greater occipital nerve accompanies the terminal portion of the artery.
Divisions
- The sternocleidomastoid branch
- The auricular branch
- The mastoid branch
- The descending branch
- The occipital branches
- The meningeal branch
Blood supply
The occipital artery helps supply blood to the dura mater, the auricle, the sternocleidomastoid, and the deep posterior muscles of the back.
Anatomical variants
May originate from the internal carotid artery. Additionally, it may share a common origin trunk from the external carotid artery with other branches, e.g. the ascending pharyngeal, the posterior auricular, and the superior thyroid arteries.
Posterior auricular artery
Origin
The posterior aspect of the external carotid artery above the digastric and stylohyoid muscles.
Course
Ascends within the digastric triangle of the neck, continuing between the parotid gland and styloid process of the temporal bone until it reaches the auricle of the ear. It then travels in a groove between the auricular cartilage and the temporal bone’s mastoid process until it terminates at the scalp posterior to the auricle.
Divisions
- The stylomastoid artery
- The posterior tympanic branch
- The auricular branch
- The occipital branch
- The parotid branch
Blood supply
The posterior auricular artery helps supply blood to the semicircular canals, the bony tympanic cavity, the tympanic membrane, the external auditory meatus, and the facial nerve.
Anatomical variants
May branch off the occipital artery instead of the external carotid artery.
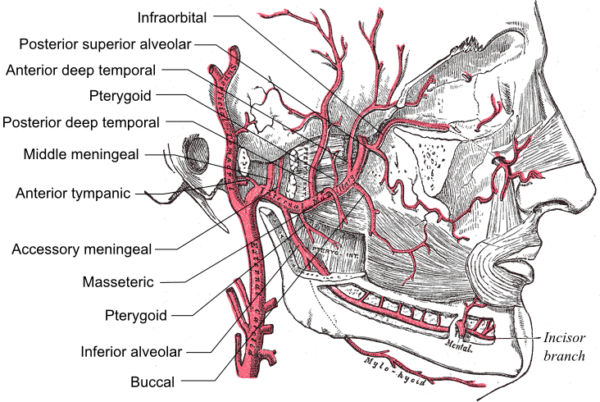
Maxillary artery
Origin
From the external carotid artery, deep to the neck of the mandible, initially embedded in the substance of the parotid gland.
Course
Passes between the neck of the mandible and the sphenomandibular ligament and runs towards the pterygopalatine fossa (either superficially or deep to the lateral pterygoid muscle) where it terminates.
Divisions
The maxillary artery divides into three portions based on its relationship to the lateral pterygoid muscle:
- The mandibular (first) division (before the lateral pterygoid muscle)
- The pterygoid (second) division (on the lateral pterygoid muscle)
- The pterygopalatine (third) division (after the lateral pterygoid muscle)
The mandibular division consists of five branches:
- The deep auricular artery
- The anterior tympanic artery
- The middle meningeal artery
- The accessory meningeal artery
- The inferior alveolar artery
The pterygoid division consists of five branches:
- The masseteric artery
- The pterygoid artery
- The buccal (buccinator) artery
- The anterior and posterior deep temporal arteries
The pterygopalatine division consists of six branches:
- The posterior superior alveolar artery
- The infraorbital artery
- The artery of the pterygoid canal
- The pharyngeal artery branch
- The descending palatine artery
- The sphenopalatine artery
Blood supply
The maxillary artery helps supply blood to the tympanic membrane, the Eustachian tube and external ear, the mandible, the maxilla, the calvaria, the dura mater, the mucosa of the nasal septum and turbinates, and many muscles of the face.
Anatomical variants
Approximately 66% travel laterally to the lateral pterygoid muscle, and 33% travel medially.
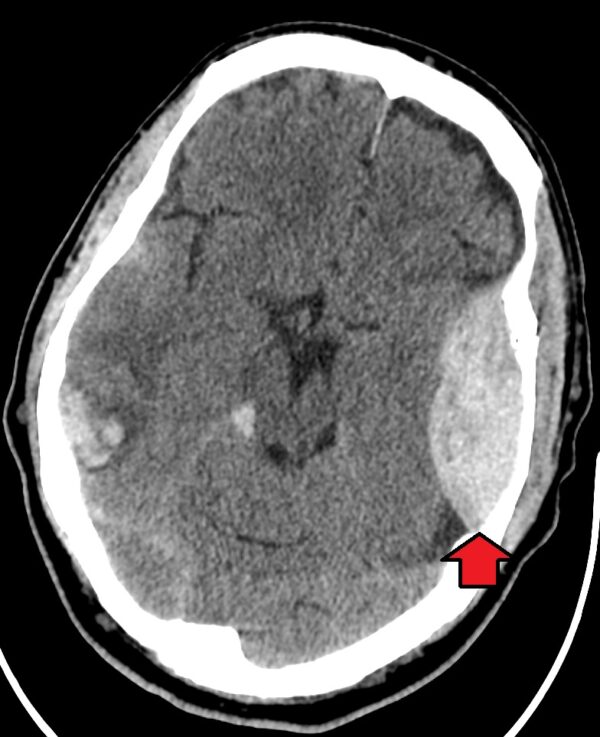
Clinical relevance: Extradural (epidural) hematomas
Extradural haematomas form from trauma to the middle meningeal artery (which supplies the calvaria and the dura mater) at the pterion. This causes a hematoma formation between the layers of the dura.
A characteristic clinical presentation is a lucid interval following an initial loss of consciousness before an eventual second loss of consciousness. Epidural hematomas require emergency evacuation to release pressure from the brain.
Superficial temporal artery
Origin
In the parotid gland at the level of the neck of the mandible.
Course
Passes superficially over the posterior root of the zygomatic process of the temporal bone, in front of the tragus of the auricle. Upon reaching the calvaria, it divides into its terminal branches: anterior (frontal) and posterior (parietal).
Divisions
- The parotid branch
- The transverse facial artery
- The anterior auricular branch
- The zygomatico-orbital artery
- The middle temporal artery
- The anterior (frontal) branch
- The posterior (parietal) branch
Blood supply
The superficial temporal artery helps supply blood to the muscles and skin of the face and scalp.
Anatomical variants
Some people may lack either the frontal or parietal branch. Branches may arise directly from alternate origins, e.g. the transverse facial artery arising directly from the external carotid artery.
Clinical relevance: Giant cell arteritis (temporal arteritis)
Giant cell arteritis is a common primary systemic vasculitis, which often affects the superficial temporal artery (thus is also referred to as temporal arteritis).
It can present with headache +/- scalp tenderness, jaw claudication, transient vision loss, and systemic symptoms such as fever and lethargy. In addition, a weakly palpable pulse and bruit may be present over the superficial temporal artery. A superficial temporal artery biopsy is required for diagnosis. Corticosteroids are the primary treatment.
For more information, see the Geeky Medics guide to temporal arteritis.
Giant cell arteritis can also manifest in the lingual artery, leading to oedema, pallor, pain, and intermittent claudication. Following a superficial temporal artery biopsy, the posterior auricular artery is required to compensate for blood supply to the area.
Clinical relevance: Head and neck surgery
Knowledge of the external carotid artery branches is essential for head and neck surgery, as these structures present a high risk of profuse bleeding. Procedures such as thyroid surgery or maxillofacial surgery may require ligation of the superior thyroid artery and facial artery, respectively.
In addition to bleeding risk, branches of the external artery play a significantly beneficial role in procedures of the head and neck. The facial artery acts as a vascular supply for flaps in the reconstructive procedures of the face whilst providing the blood supply necessary for the healing process following maxillofacial surgical procedures. The occipital artery and posterior auricular artery can be used as graft vessels to restore blood supply following lesions to the Circle of Willis.
Reviewer
Dr Timo Van Aswegen
Radiology Registrar
Editor
Dr Chris Jefferies
References
Reference texts
- Brennan, P.A., Standring, S.M., and Wiseman, S.M. Gray’s Surgical Anatomy (1st edition). Elselvier (2019). ISBN: 9780702073885
- Gofur, E.M., Al Khalili, Y. 2022. Anatomy, Head and Neck, Internal Maxillary Arteries. Available from: [LINK]
- Guo Y, Chen H, Chen X, Yu J. Clinical importance of the occipital artery in vascular lesions: A review of the literature. (2019). The Neuroradiology Journal, 32(5):366-375. doi: 10.1177/1971400919857245.
- Hacein-Bey, L., Daniels, D.L., Ulmer, J.L., Mark, L.P., Smith, M.M., Strottmann, J.M., Brown, D., Meyer, G.A., Wackym, P.A. (2002). The ascending pharyngeal artery: branches, anastomoses, and clinical significance. American Journal of Neuroradiology, 23(7):1246-56.
- Hyun Jin Park, Ji-Hyun Lee, Wonsug Jung. (2022). The Superficial Temporal Artery and Zygomatico-Orbital Artery: Superficial Arterial Distribution of the Anterior Temple Area. BioMed Research International, vol. 2022, Article ID 3790546, 6 pages.
- Isolan, G.R., Pereira, A.H., de Auiar, P.H.P., Antunes, A.C.M., Mousquer, J.P., and Pierobon, M.R. (2011). Microsurgical anatomy of the external carotid artery: a stereoscopic study. Jornal Vascular Brasileiro, 11(1), 3-11. Retrieved from https://www.jvascbras.org
- Lettau, J. and Bordoni, B., 2022. Anatomy, Head and Neck, Lingual Artery. Available from: [LINK]
- Meegalla, N., Sood, G., Nessel, T.A., et al. 2021. Anatomy, Head and Neck, Facial Arteries. Available from: [LINK]
- Moore, K. L., Dalley, A. F., & Agur, A. M. Clinically oriented anatomy (8th edition). Lippincott Williams & Wilkins. (2017). ISBN: 9781975104962
- Nguyen, J.D., Duong, H. 2022. Anatomy, Head and Neck, Posterior Auricular Artery. Available from: [LINK]
- Sethi, D., Gofur, E.M., Munakomi, S., 2021. Anatomy, Head and Neck, Carotid Arteries. Available from: [LINK]
- Standring, S. Gray’s Anatomy (42nd edition). Elselvier (2020). ISBN: 9780702077074
- Thwin, S.S., Soe, M.M., Myint, M., Than, M. and Lwin, S. (2010). Variations of the origin and branches of the external carotid artery in a human cadaver. Singapore Medical Journal, 51(2), e40.
- White, A. M. and Lasrado, S., 2021. Anatomy, Head and Neck, Thyroid Arteries. Available from: [LINK]
Reference images
- Figure 1. Mikael Häggström. External carotid artery. License: [Public domain]
- Figure 2. Mikael Häggström. Maxillary artery branches. License: [Public domain]
- Figure 3. James Heilman. Epidural hematoma. License: [CC BY-SA 4.0]




