- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Thrombocytopenia is a condition characterised by an abnormally low platelet count (<150 x 109/L). Platelets (also known as thrombocytes) are disc-shaped cell fragments whose function is to react to blood vessel injury by clumping to initiate the formation of a blood clot. Thrombocytopenia increases the risk of bleeding, however, most cases of thrombocytopenia are detected on a routine full blood count (FBC) in otherwise asymptomatic patients.
Aetiology and risk factors
There are many causes of thrombocytopenia, which can be broken down into three broad categories; reduction in platelet production, a reduction in platelet survival and dilution of platelet numbers.1
The average platelet life span is around 5 days, meaning even brief disruption to platelet production or survival can result in thrombocytopenia.
Reduction in platelet production
Reduced platelet production will quickly translate to reduced numbers of platelets in the circulation due to their relatively short life span (5 days).
Some causes of reduced platelet production include:
- Viral infections such as herpes simplex virus, cytomegalovirus, varicella-zoster virus, Epstein-Barr virus, rubella, enterovirus, mumps, hepatitis, and HIV.
- Chemotherapy agents: result in direct bone marrow toxicity, inhibiting the production of platelets.
- Aplastic anaemia: a form of bone marrow failure typically of idiopathic aetiology.
- Haematological malignancy such as leukaemia: due to crowding of the bone marrow by malignant cells.
- Non-haematological metastatic malignancy: again due to invasion and crowding of the bone marrow by malignant cells.
- B12 and folate deficiency: typically causes macrocytic anaemia and in some cases thrombocytopenia.
- Excess alcohol intake: results in direct bone marrow toxicity and liver cirrhosis.
- Congenital conditions including Fanconi’s anaemia, Wiskott-Aldrich syndrome (WAS) and many others.
Decreased platelet survival
If platelets survive for a shorter duration and the bone marrow is unable to adequately increase its production of platelets to match those being lost, thrombocytopenia will develop.
Platelet survival can be reduced by immune and non-immune causes.
Immune-mediated decreased platelet survival
Immune-mediated destruction of platelets typically occurs as a result of antibodies being directed at various platelet components.
Some immune causes of decreased platelet survival include:
- Idiopathic thrombocytopenic purpura (ITP): antibodies directed at the surface of platelets result in their destruction.
- Systemic lupus erythematosus
- Rheumatoid arthritis
- Sarcoidosis
- Antiphospholipid syndrome
Non-immune decreased platelet survival
Some non-immune causes of decreased platelet survival include:
- Medications (e.g. heparin, carbamazepine, ibuprofen, rifampin, trimethoprim, vancomycin)
- Splenomegaly: the spleen sequesters more platelets than normal, decreasing the total circulating number of platelets.
- Haemolytic uraemic syndrome (HUS): toxins from E.coli cause increased thrombogenicity of the vascular endothelium which results in the consumption of platelets due to thrombotic microangiopathy.
- HELLP syndrome: platelets are consumed due to increased exposure to von Willebrand’s factor resulting in widespread thrombotic microangiopathy.
- Thrombotic thrombocytopenic purpura (TTP): reduction in the function of the enzyme ADAMTS13 normally responsible for the breakdown of von Willebrand’s factor results in platelets being excessively consumed due to a similar mechanism as that described in HELLP syndrome.
Pseudothrombocytopenia
Pseudothrombocytopenia occurs when platelets undergo a phenomenon called ‘clumping’, in which they stick together causing a false low reading when passed through an auto-analyser.
Clinical features
History
Patients with thrombocytopenia are often asymptomatic until platelets fall to very low levels (often below 10) and as a result, most cases are detected incidentally on full blood counts performed for unrelated reasons.
However, if a patient injures themselves or undergoes a procedure whilst significantly thrombocytopenic (e.g. dental work, surgery) they are at risk of developing major haemorrhage.
If you suspect a patient may have thrombocytopenia, it is important to take a thorough bleeding history.
Typical symptoms associated with thrombocytopenia include:
- Spontaneous bruising or excessive bruising as a result of a minor injury
- Bleeding gums
- Epistaxis which may be excessive, frequent and prolonged
- Gastrointestinal bleeding: haematemesis, haematochezia and melaena
- Genitourinary bleeding: haematuria, post-coital bleeding
- Menorrhagia
Other important areas to cover:
- Recent infections
- Surgical history: ask about previous surgery and if there were any issues with bleeding or bruising.
- Dental history: ask about previous dental procedures and if there was significant bleeding.
- Obstetric history: ask about delivery and associated complications (e.g. post-partum haemorrhage)
- Medication history: ask about current medications (including blood thinning medication) and any recently prescribed medication or dose changes.
- Family history: ask about any history of bleeding problems in the family.
Symptoms of occult malignancy should also be screened for including: 2
- Bone pain
- Night sweats
- Weight loss
- Left upper quadrant discomfort (e.g. splenomegaly)
- Excessive thirst, urination and constipation (myeloma)
Clinical examination
Typical clinical findings in patients with severe thrombocytopenia include:
- Petechiae (<2 mm)
- Purpura (0.2-0.1 cm)
These can be found on the skin and the oral mucosa.
A lymphoreticular examination should be performed to look for evidence of underlying haematological malignancy (e.g. lymphadenopathy and/or hepatosplenomegaly).
Investigations
Blood tests
Blood tests relevant to thrombocytopenia include:
- Full blood count (FBC)
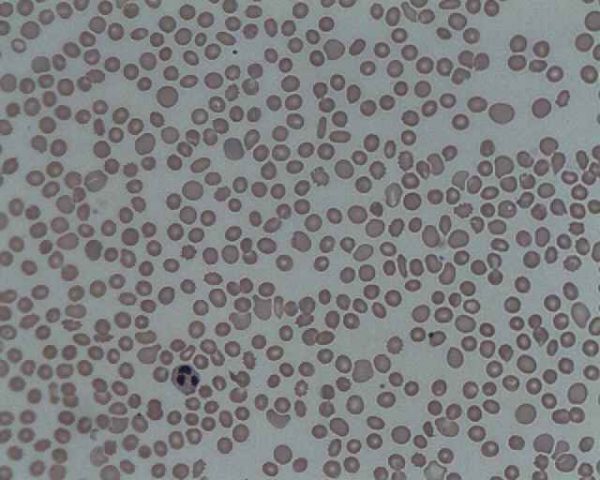
- Blood film
- U&Es
- Prothrombin time (PT) and activated partial thromboplastin time (aPTT)
- B12 and folate
Bone marrow biopsy
Bone marrow biopsy may be indicated if there are concerns about underlying malignant invasion of the bone marrow (e.g. leukaemia) or aplastic anaemia.
Genetic screening
Patients may undergo genetic screening if a congenital cause of thrombocytopenia is suspected.
Management
There is a wide range of management options for thrombocytopenia which differ depending on the underlying aetiology. Below is a brief overview of a range of different management options which may be considered for patients with thrombocytopenia.
Secondary care referral
Hospital referral is not usually required if the patient has modest isolated thrombocytopenia (platelet count 100-150 x 109/L), without atypical features such as lymphadenopathy or fever.1 FBC should, however, be monitored closely in primary care to ensure that platelets and other blood counts are not continuing to deteriorate (e.g. aplastic anaemia). Patients should be advised to seek review if they experience any bleeding or spontaneous bruising.
Indications for urgent referral to haematology include:
- severe thrombocytopenia (20 x 109/L)
- severe bleeding
- red cell fragments or blasts on the blood film
- a history of constitutional symptoms (e.g. fever, weight loss, night sweats), spontaneous bruising/bleeding or abnormalities on examination of the blood film.
Consider a discussion with a haematologist if the platelet count is less than 100 x 109/L.
Patient education
Patients with severe thrombocytopenia are advised:
- to avoid contact sports and activities which increase their risk of significant trauma
- to avoid NSAIDs (which impair platelet function)
- to maintain good dental hygiene (to minimise the risk of gingival bleeding and the need for dental procedures)
- to avoid deep intramuscular injections if possible
If patients with thrombocytopenia require surgical or dental procedures, they may be provided with treatments to temporarily increase their platelet count (e.g. platelet transfusion, steroids) or increase clot stability (e.g. tranexamic acid).
Platelet transfusion
Platelet transfusions are often required for patients with severe thrombocytopenia (e.g. <10 x 109/L) or for those who need a temporary boost to their levels for a procedure (e.g. major surgery). Transfusions should be used sparingly as there is a risk of alloimmunisation against HLA antigens and/or platelet glycoproteins.
Platelet transfusions are also used in the emergency setting if patients with thrombocytopenia are actively bleeding.
Tranexamic acid
Tranexamic acid reduces the conversion of plasminogen to plasmin, preventing fibrin degradation and increasing clot stability.
Gauze soaked in tranexamic acid may be used to manage superficial bleeding.
Oral or intravenous preparations of tranexamic acid may also be used in the peri/post-operative period to increase clot stability and reduce the risk of bleeding.
Steroids
Steroids (e.g. prednisolone) are commonly used in the management of immune-mediated thrombocytopenia (e.g. ITP) to suppress immune-mediated destruction of platelets allowing for count recovery.
Thrombopoietin receptor (TPO) agonists
TPO agonists such as Eltrombopag (daily tablet) and Romiplostim (weekly subcutaneous injection) directly stimulate the production of platelets by the bone marrow. They are typically used as a second-line treatment in ITP (if steroids fail) and also in the management of aplastic anaemia.
Bone marrow transplantation
Allogenic bone marrow transplantation is only used in cases of severe thrombocytopenia unresponsive to other therapies (e.g. aplastic anaemia). Treatment involves induction chemotherapy to wipe out the host’s stem cells and then infusion of donor stem cells in the hope of curing the underlying pathology. There is a wide range of serious acute and chronic complications of allogeneic bone marrow transplantation which are beyond the scope of this article.
Complications
The major potential complication of thrombocytopenia is excessive and uncontrolled bleeding (e.g. gastrointestinal haemorrhage, intracranial haemorrhage).3
Key points
- Thrombocytopenia is defined as a platelet count of <150 x 109/L.
- The average platelet life span is around 5 days, meaning even brief disruption to platelet production or survival can result in thrombocytopenia.
- Thrombocytopenia increases the risk of bleeding, however, most cases of thrombocytopenia are incidentally detected on a routine full blood count (FBC) in otherwise asymptomatic patients.
- Typical clinical signs associated with severe thrombocytopenia include petechiae and purpura on the skin and mucous membranes.
- Key investigations for thrombocytopenia include a full blood count and blood film.
- There is a wide range of management options for thrombocytopenia including patient education, platelet transfusion, tranexamic acid, steroids and TPO receptor antagonists.
- The main potential complication of thrombocytopenia is major haemorrhage.
References
- Patient.info, Thrombocytopenia and Platelet Function Disorders, Published 14.01.2015. Available from: [LINK]
- BMJ Best Practice, Assessment of Thrombocytopenia, Published 2018. Available from: [LINK]
- National Heart, Lung and Blood Institute, Thrombocytopenia. Available from: [LINK]
- James Heilman, MD. Licence: CC BY-SA. Available from: [LINK]
- AfroBrazilian. Licence: CC BY-SA. Available from: [LINK]
- Prof. Erhabor Osaro. Licence: CC BY-SA. Available from: [LINK]