- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Trigeminal neuralgia is a form of neuropathic pain characterised by a sharp, shooting sensation affecting the face. The pain is intense and often significantly impacts quality of life.
The condition typically affects people over 50 but can occur at any age and is more common in women.1,2
Aetiology
Anatomy
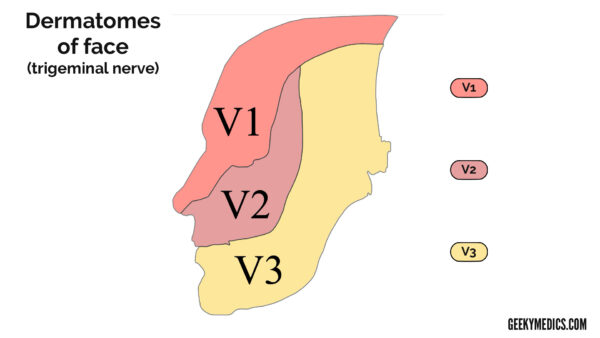
The trigeminal nerve (CN V) conveys sensory input from the face in a mask-like distribution and provides motor supply to the muscles of mastication via three divisions:
- The ophthalmic branch (upper, V1) supplies sensation to most of the cornea, scalp and forehead
- The maxillary branch (middle, V2) supplies sensation to the cheek, upper jaw, upper lip, teeth and gums, and the lateral aspect of the nose
- The mandibular branch (lower, V3) supplies sensation to the lower jaw, teeth and gums, and lower lip
Pathophysiology and classification
Trigeminal neuralgia is caused by disruption to the nerve function. The underlying pathophysiology is demyelination of the nerve, which is believed to be caused by compression.
Trigeminal neuralgia can be divided into 3 types:3
- Classic trigeminal neuralgia: vascular compression by a nearby artery or vein (most commonly the superior cerebellar artery)
- Secondary trigeminal neuralgia: relating to a tumour or due to underlying disease (e.g. multiple sclerosis, damage following facial injury/surgery, cyst or tumour)
- Idiopathic trigeminal neuralgia: if the cause is unknown
Risk factors
Risk factors for trigeminal neuralgia include:2,4
- Female sex
- Age (more common >50)
- Multiple sclerosis (increases the risk by a factor of 20 in comparison to the general population)
Clinical features
History
The classical presentation of trigeminal neuralgia is episodes of unilateral, sharp facial pain (which may be described as “burning”).5,6
Episodes may be associated with triggers, including:5,6
- Talking
- Washing the face
- Shaving
- Brushing teeth
- Exposure to cold air
Episodes may be triggered with only minor stimuli, and patients may be reluctant to have their face examined or touched due to fear of triggering the pain.
Less commonly, patients can experience ophthalmic symptoms, including lacrimation, conjunctival redness and photophobia.7
Clinical examination
In classic/idiopathic trigeminal neuralgia, physical examination including neurological examination, is usually normal. In secondary trigeminal neuralgia, there may be signs of the underlying disease process causing trigeminal neuralgia.
Differential diagnoses
Unilateral face pain can be a common presenting complaint for multiple other conditions such as migraines, cluster headaches, atypical facial pain, dental neuralgia and TMJ dysfunction:8
- Cluster headache: the patient is usually between 30-40 years old, six to nine times more common in females. Symptoms are always unilateral, lasting up to 1.5 hours and can be accompanied by other symptoms conjunctival injection and epiphora. These headaches occur in clusters, with weeks to months intervals
- Migraine: age of onset is usually around 20 years of age, can be unilateral or bilateral, has other associated symptoms such as photophobia. The attack can last 4-72 hours, it cycles in days to weeks intervals, with many different factors provoking the attacks.
- Atypical facial pain: affects face, neck and ear instead of just the trigeminal area, can last hours to days, pain is described as throbbing pain that is mild/moderate in severity. Can be provoked by stress and cold and associated with sensory abnormalities
If symptoms are bilateral, this can warrant further investigations, such as MRI, to rule out multiple sclerosis. Multiple sclerosis can have similar symptoms as TN, hence in younger patients, you would look for other symptoms (e.g. focal weakness, ataxia, optic neuritis/vision changes).
Investigations
Trigeminal neuralgia is usually a clinical diagnosis. However, investigations, such as blood tests and imaging, can be used to exclude other diagnoses or secondary causes of trigeminal neuralgia.
Inflammatory markers such as WCC and CRP can exclude causes. Imaging such as a brain MRI will be used to identify any cerebellopontine angle tumours, vascular abnormalities or areas of demyelination suggestive of multiple sclerosis.
Management
Medical management
Current NICE guidelines suggest carbamazepine, an anti-convulsant, for first-line management.6
Side effects include dizziness, drowsiness, nausea, diplopia, and hyponatraemia. If side effects are not tolerated or carbamazepine doesn’t relieve symptoms, the patient should be referred to a specialist.
Other treatment options include oxcarbazepine, lamotrigine, topiramate, gabapentin and pregabalin. Management of ophthalmic symptoms includes eye care and anaesthetic eyedrops.
Surgical management
If symptoms persist despite medical management, there are surgical options available to decompress the nerve or to ablate the nerve to prevent pain transmission through the nerve. However, these procedures have risks, especially if the V1 nerve is damaged, which can cause corneal anaesthesia.7
Complications
Pain caused by trigeminal neuralgia can be so severe that patients’ activities of daily living become impaired, and they are at risk of depression.6
Key points
- Trigeminal neuralgia is a debilitating condition causing episodes of severe facial pain
- Risk factors include age (>50), sex (F>M) and co-morbidities (especially multiple sclerosis)
- Clinical examination is usually normal, unless there is an underlying condition causing trigeminal neuralgia
- Investigations (e.g. imaging/MRI) are usually not required
- First line management is carbamazepine, surgical intervention can be considered for severe symptoms refractory to medical management
- Complications include impact on activities of daily living and depression
Reviewers
Dr Hameed Shalash
Consultant Neurologist
Dr Russel Tilney
Honorary Clinical Research Fellow
UCL
References
- National Institute of Neurological Disorders and Stroke. Trigeminal neuralgia. Published November 2023. Available from: [LINK]
- Maarbjerg, S., Gozalov, A., Olesen, J., & Bendtsen, L. (2014). Trigeminal neuralgia–a prospective systematic study of clinical characteristics in 158 patients. Headache: The Journal of Head and Face Pain, 54(10), 1574-1582.
- Olesen, J. (2018). Headache classification committee of the International Headache Society (IHS), the international classification of headache disorders. Cephalalgia, 38(1), 1-211.
- Cruccu, G., Di Stefano, G., & Truini, A. (2020). Trigeminal neuralgia. New England Journal of Medicine, 383(8), 754-762.
- Cruccu, G., Finnerup, N. B., Jensen, T. S., Scholz, J., Sindou, M., Svensson, P., … & Nurmikko, T. (2016). Trigeminal neuralgia: new classification and diagnostic grading for practice and research. Neurology, 87(2), 220-228.
- NICE CKS. Trigeminal neuralgia. Available from: [LINK]
- Bhatti, M. T., & Patel, R. (2005). Neuro-ophthalmic considerations in trigeminal neuralgia and its surgical treatment. Current Opinion in Ophthalmology, 16(6), 334-340.
- Singh MK, Egan RA. Trigeminal Neuralgia Differential Diagnoses. Published 2019. Available from: [LINK]




