- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Hyponatraemia occurs when there is a relative excess of water in the body compared to sodium. It is the most common electrolyte abnormality encountered in clinical practice. However, it can be challenging to diagnose and treat effectively.
Hyponatraemia is a serum sodium concentration <135mmol/L, with severe hyponatraemia being a serum sodium concentration <120mmol/L. It is often further categorised into acute (<48h duration) or chronic hyponatraemia.
Acute hyponatraemia can be life-threatening due to cerebral fluid shifts associated with the reduction in serum sodium.
The key to appropriate management of hyponatraemia is understanding the different underlying causes of hyponatraemia and how these relate to the patient’s hydration status.
Normal physiology
Serum osmolality measures the concentration of solutes in the blood, and sodium is the most important determinant of serum osmolality.
Serum osmolality determines the osmolar concentration of plasma. The law of osmosis states that water will flow from compartments with lower osmolality to compartments with higher osmolality, so long as the membrane separating the two compartments is permeable. In the body, this will occur between the plasma and interstitial (extracellular) fluid compartments, and also between the extracellular and intracellular compartments.
Any alteration in sodium concentration will affect serum osmolality, ultimately leading to shifts in water (osmotic shifts) between the intracellular and extracellular compartments.
Serum sodium regulation is maintained by a complex homeostatic mechanism involving thirst, anti-diuretic hormone (ADH), the renin-angiotensin-aldosterone system (RAAS) and renal sodium excretion.1 Dysfunction at any stage of this mechanism can lead to the development of hyponatraemia.
In healthy individuals, ADH is released in response to increased serum osmolality, leading to increased water retention in the collecting ducts of the kidney. This leads to a corresponding fall in serum osmolality.
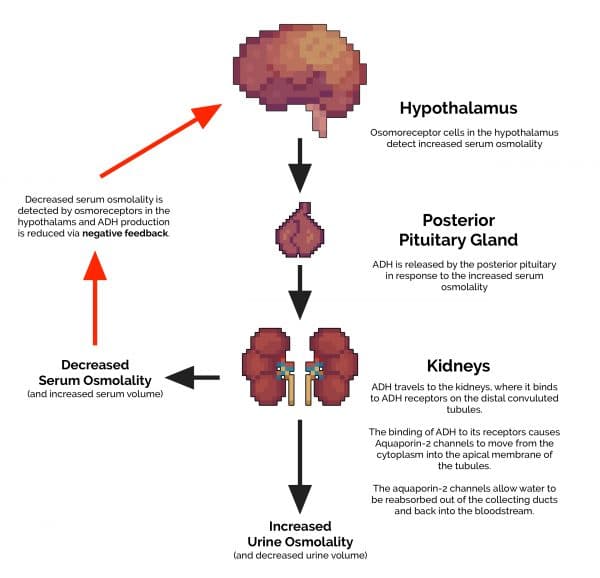
By the same mechanism, water ingestion will not lead to hyponatraemia as the fall in osmolality leads to suppression of ADH secretion, allowing water to be excreted in dilute urine.2
Note: One mechanism by which hyponatraemia can develop is inappropriate ADH secretion, i.e. ongoing secretion of ADH when osmolality is low or normal. This is a common cause of hyponatraemia, known as SIADH.
Causes of hyponatraemia
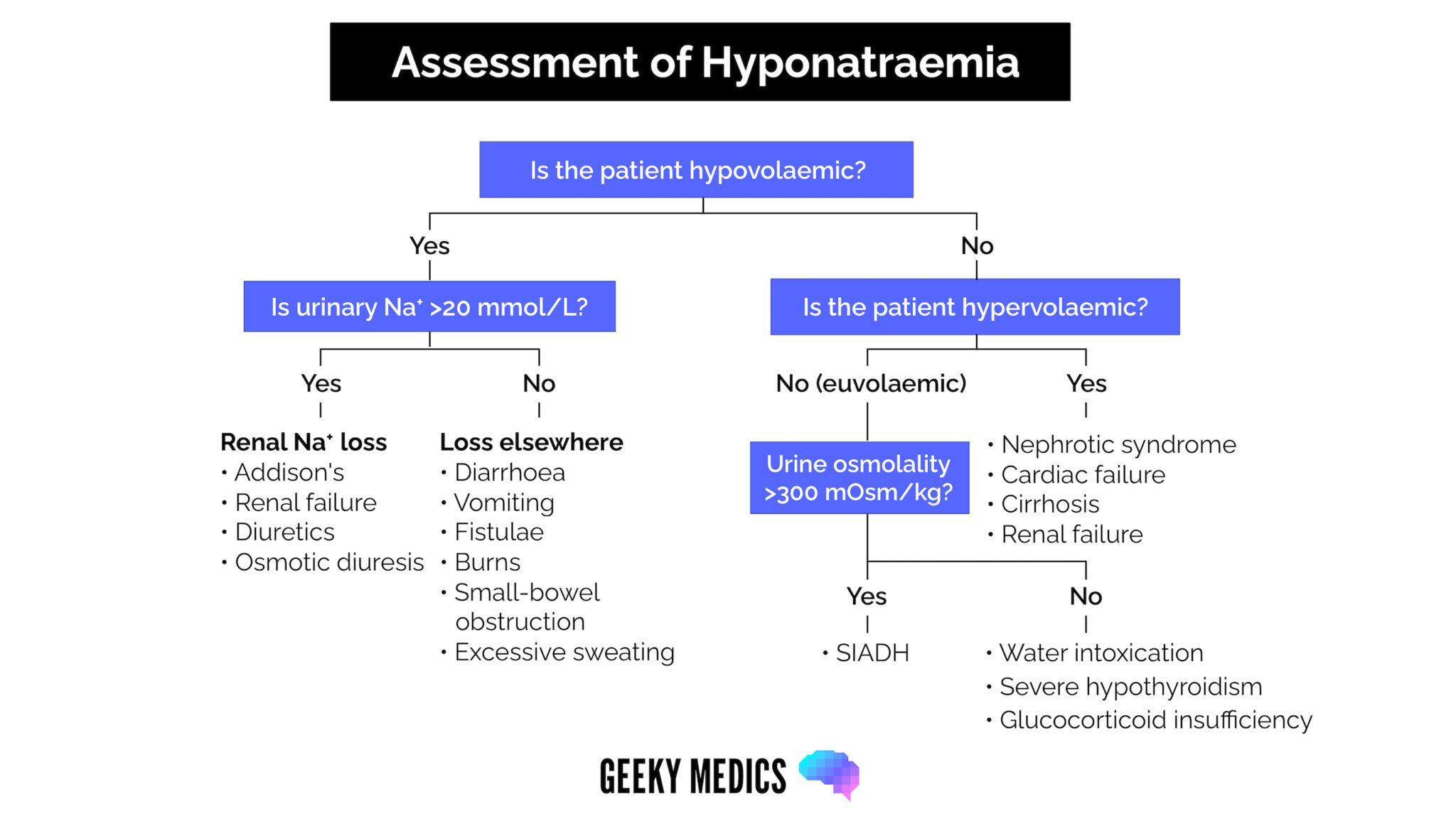
Hyponatraemia can develop by many different mechanisms. The critical first step in identifying the cause of hyponatraemia is determining whether the patient is:
- Hypovolaemic (dehydrated)
- Hypervolaemic (‘overloaded’)
- Euvolaemic
This is primarily achieved by clinical examination of hydration status.
Hypovolaemic hyponatraemia
In a hypovolaemic patient, hyponatraemia may be secondary to renal sodium loss or sodium loss from elsewhere (transdermal/gastrointestinal).
In either case, sodium is lost in association with water (which explains why the patient is hypovolaemic). Patients often drink hypotonic fluids (e.g. water, juice) to rehydrate, further worsening the hyponatraemia.
Urine sodium
Urine sodium is an important investigation in hypovolaemic hyponatraemia.
In a normally functioning kidney, sodium should be conserved in the urine if serum sodium levels are low:
- Urinary sodium >20mmol/L suggests a renal cause of sodium loss (the kidney is not conserving sodium)
- Urinary sodium <20mmol/L suggests a non-renal cause of sodium loss (the kidney is conserving sodium, but the sodium is being lost from elsewhere)
Renal causes of sodium loss (urine sodium >20mmol/L) include:
- Renal failure: creatinine will be increased, eGFR decreased
- Addison’s disease: associated with hyperkalaemia
- Excess diuretic medications: particularly thiazide-like diuretics
- Osmotic diuresis: severe hyperglycaemia
Non-renal causes of sodium loss (urine sodium <20mmol/L) include:
- Gastrointestinal losses: vomiting, diarrhoea, small bowel obstruction, fistulae
- Skin losses: excess sweating, burns
Hypervolaemic hyponatraemia
In a fluid overloaded patient, fluid accumulates in the extracellular (‘third’) space. This extra fluid causes a dilutional effect on serum sodium, causing hyponatraemia. In other words, there is more water than sodium, leading to a relative sodium deficiency.
It is important to diagnose and treat the underlying cause of fluid overload:
Congestive cardiac failure
In cardiac failure, fluid retention occurs due to various neuro-hormonal mechanisms, primarily affecting the renin-angiotensin-aldosterone system. There is also increased venous capillary pressure, encouraging fluid extravasation as oedema.
Liver cirrhosis (liver failure)
Decreased albumin synthesis leads to hypoalbuminaemia. This causes reduced oncotic pressure in the bloodstream, leading to fluid loss into the extracellular space. Furthermore, increased pressure in the portal venous system (portal hypertension) leads to fluid accumulation in the peritoneal space (ascites).
End-stage renal failure
In end-stage renal failure, the kidney loses the ability to effectively act as a filter from the bloodstream, and urine output decreases. This leads to significant fluid retention, although eGFR must be severely reduced for this to be the cause of oedema (end-stage renal failure).
Nephrotic syndrome
In nephrotic syndrome, inappropriate loss of albumin through the glomerulus leads to hypoalbuminaemia, which decreases plasma oncotic pressure, and fluid accumulates in the extracellular space.
Euvolaemic hyponatraemia
In euvolemic hyponatraemia, the diagnosis is most commonly SIADH. Less common causes include primary polydipsia or severe endocrine disturbances (hypothyroidism/cortisol deficiency).2
Urine osmolality
In euvolaemic hyponatraemia, it is important to check the urine osmolality. Urine osmolality measures the concentration of solutes in the urine, including sodium and urea, and will often be measured in conjunction with serum osmolality.
Under normal conditions, urine osmolality should be decreased when serum sodium (and serum osmolality) is low, as the body attempts to conserve sodium by producing dilute urine.
If the urine osmolality is raised (>300mOsm/kg – concentrated urine with high sodium levels), the diagnosis is likely SIADH. The key concept to understand is that a raised urine osmolality in the presence of low serum osmolality suggests SIADH, as the kidney is inappropriately producing concentrated urine despite low serum osmolality.
If the urine osmolality is decreased (<300mOsm/kg – dilute urine), water intoxication may be the cause (primary polydipsia). This can be seen in patients with psychiatric disturbances or users of the recreational drug ecstasy. Rarer causes include severe hypothyroidism or glucocorticoid deficiency.
Hyponatraemia flowchart
Once the patient’s hydration status has been determined and urine osmolality/urine sodium has been checked, the flowchart below can be followed to narrow down the cause of hyponatraemia.
Clinical features
The clinical features of hyponatraemia are primarily neurological, developing due to the effects of cerebral oedema, which can occur secondary to fluid shifts across the blood-brain-barrier.3
Clinical features depend on the severity of hyponatraemia and the rate of change in sodium concentration, as the brain can adapt to a slowly developing chronic hyponatraemia.1
Some patients with chronic hyponatraemia of 120mmol/L (severe) may be relatively asymptomatic. However, others with acute hyponatraemia of 130mmol/L (mild) may have severe symptoms.
History
Mild to moderate symptoms of hyponatraemia include:4
- Anorexia
- Headache
- Nausea/vomiting
- Lethargy
- Confusion
- Ataxia
Severe symptoms of hyponatraemia include:
- Seizures
- Cerebral obtundation / coma
Clinical examination
The key to clinical examination in hyponatraemia is an accurate assessment of fluid/hydration status, as this will help to classify the likely cause of hyponatraemia and guide initial management.
It is important to check for neurological signs that would indicate severe hyponatraemia.
Signs of hypovolaemia include:
- Tachycardia, hypotension (late sign)
- Dry mucous membranes
- Reduced skin turgor
Signs of hypervolaemia include:
- Peripheral oedema
- Raised jugular venous pressure (JVP)
- Bibasal lung field crepitations (pulmonary rales)
Neurological signs of severe hyponatraemia include:
- Cognitive impairment
- Drowsiness
- Signs of seizure activity/brainstem herniation (indicate life-threatening hyponatraemia with cerebral oedema)
Investigations
All patients with hyponatraemia identified on a urea & electrolytes (U&E) profile will require further blood and urine tests to help determine the underlying cause of hyponatraemia. Blood and urine tests must be performed simultaneously to compare urine and serum osmolality accurately.
Laboratory investigations
Relevant blood tests include:
- Serum urea & electrolyte panel: to confirm hyponatraemia, assess renal function and potassium levels.
- Serum osmolality: usually decreased in hyponatraemia; if normal consider pseudohyponatraemia, if raised consider hyperglycaemia.
- Liver function tests: assess the albumin levels in hypervolaemic hyponatraemia, and exclude obstructive jaundice if pseudohyponatraemia is suspected.
- Serum lipids: to assess for lipaemia if pseudohyponatraemia is suspected.
- Serum glucose: significant hyperglycaemia can cause hyponatraemia, often with raised serum osmolality.
- Serum cortisol/thyroid function tests: exclude Addison’s (low cortisol level) / severe hypothyroidism (high TSH, low T3) as rare causes of euvolaemic hyponatraemia.
Note: calculated serum osmolality = (2 x Na) + Glu + Urea (all in mmol/L).
Relevant urine tests include:
- Urine osmolality: required to confirm a diagnosis of SIADH. A raised urine osmolality in the presence of low serum osmolality suggests SIADH.
- Urine sodium: useful to differentiate renal vs extrarenal cases of sodium loss in hypovolaemic hyponatraemia. Values >20mmol/L are suggestive of renal sodium loss. Urine sodium is also a useful investigation to help confirm a diagnosis of SIADH (markedly raised in SIADH >40mmol/L).2
Pseudohyponatraemia
Hyperlipidaemia, hyperproteinaemia or hyperbilirubinaemia (secondary to obstructive jaundice) can interrupt some laboratory analysis methods of measuring serum sodium, leading to falsely low readings. This is known as a pseudohyponatraemia.
Serum osmolarity is classically normal if measured. Pseudohyponatraemia is rare but important to exclude before initiating treatment for hyponatraemia.
Hyperglycaemia associated hyponatraemia
In patients with significant hyperglycaemia (e.g. DKA / HHS), the increase in serum glucose raises serum tonicity, pulling water out of cells and expanding the extracellular space, causing a dilutional effect on serum sodium concentrations.
In this case, total body sodium remains unchanged, and sodium concentration will generally correct with the correction of the hyperglycaemia. Calculated serum osmolality is classically raised.
Management
Management aims to restore a normal serum sodium level at an appropriate pace. This is primarily achieved by treating the underlying cause and aiming to restore normal volume status.
Acute severe hyponatraemia
Acute hyponatraemia with severe neurological symptoms (e.g. seizures, severe drowsiness) is a medical emergency. Initial treatment involves IV hypertonic saline bolus (100ml 3% NaCl) with close monitoring of serum sodium.5
The diagnosis and management of the underlying cause is essential once the neurological status begins to improve.
Note: Some clinicians recommend cautious hypertonic saline use in patients with severe hyponatraemia (<120 mmol/L), even without neurological symptoms. However, this is usually a consultant-led decision.5
Hyponatraemia without severe neurological symptoms5
In the absence of acute severe hyponatraemia, a cautious approach to management is taken. If the sodium is corrected too quickly, patients are at risk of severe complications (osmotic demyelination syndrome).
The general goal of treatment is to correct by no more than 6mmol/L in the first 6 hours and no more than 10mmol/L in the first 24 hours.1
The initial management approach depends on volume status. In all cases, identification and management of the underlying cause is essential.
Hypovolaemic hyponatraemia
Rehydration with intravenous 0.9% normal saline, with regular monitoring of serum sodium.
Hypervolaemic hyponatraemia
Fluid restriction (<1.5L/24h), with regular monitoring of serum sodium.
Euvolaemic hyponatraemia
Fluid restriction (1.5L/24h), with regular monitoring of serum sodium. Oral salt tablets may be required if fluid restriction alone is ineffective.
Complications
Complications of hyponatraemia include:1
- Gait disturbance and falls: particularly in elderly patients
- Cerebral oedema: can lead to brainstem herniation and death
- Osmotic demyelination syndrome: severe and often irreversible neurological deficits secondary to intracerebral fluid shifts caused by the rapid correction of hyponatraemia; classically occurs 2-4 days after the treatment, typically presenting with quadriplegia and pseudobulbar palsy
Key points
- Hyponatraemia is the most common electrolyte disturbance seen in clinical practice.
- The severity of symptoms is related to both the severity of hyponatraemia and the rate of change in serum sodium concentration.
- The range of underlying causes of hyponatraemia is broad, yet these can be separated into hypovolaemic, hypervolaemic and euvolaemic hyponatraemia.
- The key to diagnosis is an accurate assessment of hydration status.
- Acute severe hyponatraemia can be life-threatening and should be treated with hypertonic (3%) saline.
- Management depends on the underlying cause; however, care should be taken not to correct sodium concentration too rapidly due to the risk of osmotic demyelination syndrome.
Editor
Dr Chris Jefferies
References
- Patient.info Professional. Hyponatraemia. February 2021. Available from: [LINK].
- UpToDate. Diagnostic evaluation of adults with hyponatremia. July 2023. Available from: [LINK].
- UpToDate. Manifestations of hyponatremia and hypernatremia in adults. January 2021. Available from: [LINK].
- UpToDate. Overview of the treatment of hyponatremia in adults. July 2023. Available from: [LINK].
- UpToDate. Treatment of hyponatremia: Syndrome of inappropriate antidiuretic hormone secretion (SIADH) and reset osmostat. February 2022. Available from: [LINK].




