- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A 7-year-old boy is brought to the GP by his mother due to a wheeze. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
- Wheeze
History
Presenting complaint
“It’s my son, Elliot, I’ve noticed a wheeze sometimes, and it’s worrying me.”
History of presenting complaint
When did you first notice the wheeze?
“6 months ago”
When does Elliott wheeze?
“Mainly when playing sports, but also sometimes in the mornings”
Has the wheeze been getting worse over time?
“It occurs more regularly with exercise now”
Have you noticed any other triggers for the wheeze?
“He seems more wheezy after he plays with his neighbour’s cat”
Have you tried any medications for the wheeze yet?
“No”
When did you first notice the cough?
“6 months ago”
When does Elliott cough?
“He always coughs in the mornings and often before bedtime too”
Does he bring up any phlegm with the cough?
“Yes”
What colour is the phlegm?
“Usually it is colourless, but sometimes it is yellow-green when he has a cold”
Have you ever noticed blood in the phlegm?
“Never”
When was the last time he was tested for COVID-19?
“He does twice-weekly lateral flow tests for school- they are always negative”
Shortness of breath?
“He’s increasingly short of breath when playing sports now”
Chest pain?
“Only when he feels very wheezy after playing sports”
Fever?
“Only when he has a cold”
Night sweats?
“No”
Family history of asthma?
“His father had childhood asthma”
Any A&E attendances for the wheeze?
“No”
For more information, see the Geeky Medics guide to respiratory history taking.
Clinical examination
Examination findings
Respiratory examination:
- Mild expiratory wheeze bilaterally
- No intercostal recession nor tracheal tug
- RR 24
- Sats 99% on room air
Cardiovascular examination:
- HS I + II + 0
- HR 80
- CRT 2 seconds
Patient’s elbow
An image of the patient’s anterior elbow crease is shown below:

Suggestive of atopic dermatitis
- Dry and erythematous skin
- Lichenification
- Areas of skin thinning (possibly secondary to steroid overuse)
Investigations
Measuring the peak expiratory flow rate (PEFR) is the first-line investigation as it is easy to perform during the initial consultation. Patients can also be given a peak flow meter to measure their PEFR at home.
Peak flow readings
The patient’s first week of peak flow readings are shown below:
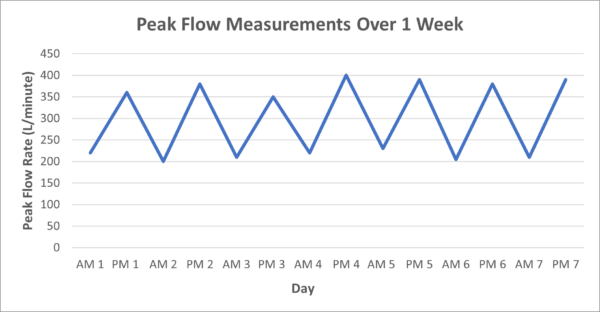
The measurements show diurnal variability, defined as a mean intra-day variation of peak expiratory flow rate >20%. In this graph, the mean intra-day variation is approximately 70%.
Diagnosis
Those in bold are the most likely, but a range of other potential differentials are shown using the VINDICATE acronym:
- Vascular –
- Inflammatory & infectious – asthma, series of lower respiratory tract infections
- Neoplastic
- Degenerative
- Idiopathic – gastro-oesophageal reflux disease, vocal cord dysfunction
- Congenital – cystic fibrosis, tracheomalacia
- Autoimmune – children’s interstitial lung disease
- Traumatic – inhaled foreign body
- Endocrine
Asthma is the most likely diagnosis. This is because asthma typically presents with wheeze/dyspnoea/cough, which are worse in the mornings and evenings, and can be triggered by exertion. Also, diurnal variation in peak expiratory flow rate is diagnostic for asthma.
Management
An inhaled corticosteroid, such as beclometasone dipropionate (Clenil) 100mcg BD, would be an appropriate initial preventer regime for a 7-year-old boy.
Complications
- Atelectasis
- Pneumonia
- Pneumothorax
- Respiratory failure
- Status asthmaticus (repeated asthma exacerbations without respite)
Editor
Dr Jess Speller
References
- James Heilman, MD. Atopy. License: [CC BY-SA]
- British Thoracic Society. BTS/SIGN Guideline for the management of asthma. Published in 2019. Available from: [LINK].