- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
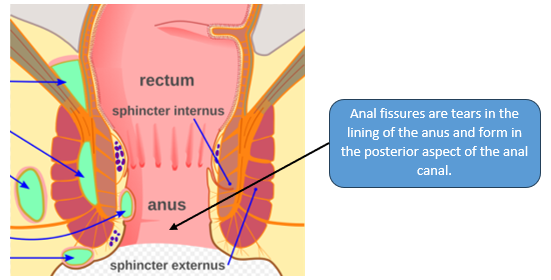
An anal fissure (fissure in ano) is a longitudinal and superficial tear of the epithelium and dermis at the anal margin extending up into the anal canal but below the dentate line.1 Anatomically, anal fissures develop in the posterior aspect of the anal canal.1
Anal fissures affect 1 in 350 people each year and can affect any age. At-risk groups include post-partum women and the elderly.1
Aetiology
Anal fissures are a multifactorial condition with many risk factors (with constipation being the most common).1-3
Pathophysiology that increases the risk of development of fissures include:3
- Mechanical/traumatic: due to the passage of a hard and bulky stool at the origin of an anodermal tear
- Hypertonia of the internal anal sphincter: this is thought to reduce the blood supply to the anus and thus slows down the healing process
- Ischaemia: hinders the healing of the fissure
Risk factors
Risk factors for the development of an anal fissure include:1-3
- Constipation
- Low fibre diet
- Inflammatory bowel disease (IBD)
- Chronic diarrhoea
- Pregnancy
- Opioid analgesia: due to constipation
Clinical features
History
Typical symptoms of anal fissures include:2-5
- Pain around the anus
- Painful defecation (described as ‘feeling like passing broken glass’)
- Rectal bleeding
- Abdominal pain (rare)
In the history, it is important to ask about a history of straining when passing stool and about the patient’s usual bowel movements – it can be useful to quantify the consistency using the Bristol stool chart. It is also important to ask about dietary and lifestyle factors (including medication) that may increase the risk of an anal fissure developing.
Consider ruling out associated systemic causes such as malignancy and inflammatory pathology by asking about:
- Vomiting
- Loss of appetite
- Weight loss
Clinical examination
In the context of a suspected anal fissure, examination of the perianal area may reveal a sentinel pile. The anal fissure itself is typically located in the posterior aspect, and can be observed by gently parting the perianal skin.2-5
A digital rectal examination is necessary but might not be possible due to the intense pain, and patients may require examination under anaesthesia (EUA).
If the digital rectal examination is tolerated, the anal canal is soft but painful on touch. The digital rectal examination aims to rule out canal irregularities and masses, which can indicate neoplastic pathology.
If tolerated, visual examination of the anal canal can be carried out using a proctoscope.
Clinical findings include:6
- Fissures can be palpable or visible around the anus
- A tear can be seen on the posterior aspect
Differential diagnoses
Possible diagnoses that present similarly to anal fissures include:1-3,6
- Thrombosed haemorrhoids: which present with anal pain and bright red rectal bleeding seen internally with a proctoscope
- Inflammatory bowel disease: presents with more chronic symptoms and other extra-intestinal features such as episcleritis and erythema nodosum
- Sarcoidosis
- Malignancy: anal carcinoma presents with red flag symptoms (change in bowel movements, weight loss, family history) and may require an examination under anaesthesia with biopsy
- Peri-anal abscess: presents with purulent discharge and anal pain. It appears as a pus-filled swelling rather than a tear in the skin.
Investigations
Bedside investigations
- Basic observations, including temperature: to rule out infected abscess
- Stool sample: to rule out infective aetiology if a patient presents with diarrhoea
Laboratory investigations
For benign anal fissures, it is a clinical diagnosis and thus does not need laboratory investigations. However, one can consider:
- Full blood count and CRP: to check for signs of inflammation
- Faecal calprotectin: to rule out inflammatory bowel disease (this test is 90% sensitive and specific)
- Thyroid function tests (TFTs): thyroid disorders can be a cause of chronic diarrhoea or constipation
Imaging
Normally imaging is not required to reach the diagnosis but is used to rule out other diagnoses like IBD or malignancy:
- CT scan
- Colonoscopy
Management
Management of anal fissures involves three objectives: relieving symptoms, controlling the promoting factor and anal fissure healing.3-4 Based on NICE guidelines, it is important to try conservative management before moving on to medications and surgery.3,6
Conservative management
Conservative management includes:2-4
- Easing pain and discomfort: patients can sit in a shallow warm bath to relieve pain; if they have severe pain topical anaesthetic (lidocaine 5% ointment) can be considered
- Keep the stool soft and avoid straining: using lactulose and other stool softeners if needed
- Dietary modification: high fibre diet and adequate fluid intake
- Hygiene: keeping the anal area clean
Medical management
Usually, anal fissures heal after two weeks on their own. If they do not heal, they may require medical management.2-4, 6-8
Glyceryl trinitrate ointment acts on anal sphincter hypertonia and causes vasodilation of the surrounding blood vessels, which can help with healing.7 A key side effect to mention to the patient is headaches post-application.
If glyceryl trinitrate is not tolerated or does not work, another medication used is a topical calcium channel blocker (e.g. diltiazem).6-8
If there is no improvement with a topical cream, the next stage would be examination under anaesthesia with botulinum toxin injections to the internal anal sphincter.6-8 Botulinum is injected into the internal anal sphincter, and this blocks the presynaptic reuptake of acetylcholine, which reduces the contraction of striated and smooth muscles of the anal canal.7
Surgical management
If the anal fissure does not heal or is reoccurring, surgery is advised. Surgery is recommended after six to eight weeks of medical treatment.2-4, 6 Surgery is only the first line if the fissure has hyperalgesia or is infected.
Different surgical procedures are available:4,7,8
- Lateral internal sphincterotomy: partial resection of the internal anal sphincter to relieve hypertonia and allow healing of the fissure left in place (the side effect of incontinence is permanent and hence not a preferred procedure in females and should consider other surgical procedures).
- Fissurectomy: an alternative involving resection of fibrous edges of the fissure. It can also be completed with anoplasty.
Complications
The main complications associated with anal fissures include:
- Faecal incontinence after surgery
- Recurrence
Key points
- An anal fissure is a benign tear in the lining of the anus, which usually forms on the posterior aspect of the anal canal
- Patients present with intense pain post-defecation and with associated bright red rectal bleeding
- The most common risk factor for anal fissures is constipation
- Management is usually conservative (high fibre diet and stool softeners), and if that is unsuccessful, patients may require surgery
- Common complications include recurrence of anal fissures and faecal incontinence due to surgery
Reviewer
Mr Sanjay Panchal
Consultant General Surgeon
Editor
Dr Jess Speller
References
- Patient.info. Anal fissure for medical professionals. Published in 2022. Available from [LINK]
- Jmarchn via Wikimedia Commons. Adapted by Geeky Medics. Outline of anorectal abscesses Published in 2023. Licence: [CC BY-SA]
- NICE CKS. Anal Fissure. Published in 2023. Available from [LINK]
- Vitton, V. et al. (2022) ‘Treatment of anal fissures: Results from a National Survey on French practice’, Clinics and Research in Hepatology and Gastroenterology, 46(4), p. 101821. doi:10.1016/j.clinre.2021.101821.
- British Journal of General Practice. Anal Fissure: diagnosis, management and referral in primary care. Published in 2019. Available from [LINK]
- Patient.info. Anal fissure. Published in 2022. Available from [LINK]
- Wollina. U ‘Pharmacological Sphincterotomy for Chronic Anal Fissure by Botulinum Toxin A.’ Published in 2008. Available from [LINK]
- Jones.O ‘Mechanism of action of botulinum toxin on the internal anal sphincter.’ Published in 2004. Available from [LINK]




