- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Neck infections can be broadly classified into superficial and deep infections. Deep neck space infections refer to infection or abscess formation in the deep tissues, fascial planes and potential spaces in the neck.1
The deep cervical fascia of the neck creates potential spaces where infection can spread and develop. The classic deep space neck infections occur in the peri-tonsillar, parapharyngeal or retropharyngeal spaces.1 These infections if left untreated can lead to sepsis, acute airway obstruction and death.
This article will cover classic deep space neck infections and other specific neck space infections including Ludwig’s angina and cervical necrotising fasciitis.
Aetiology
Anatomy
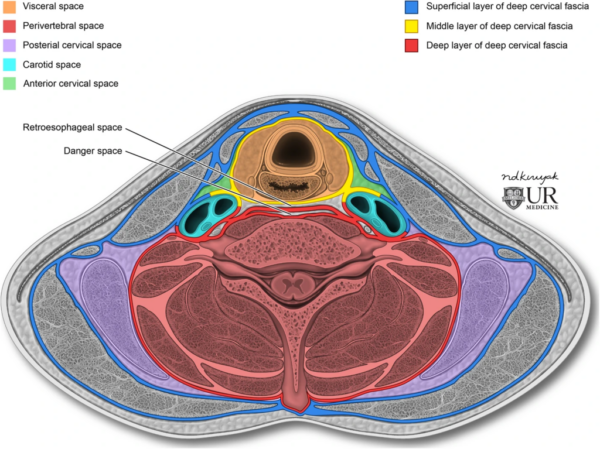
There are several potential spaces or compartments of the neck where infection can develop. These potential spaces only become apparent if filled with a fluid such as pus or blood.2
The neck is divided into deep space compartments by fascial layers. The anterior compartment compromises the carotid sheath and the pre-tracheal fascia with the posterior compartment comprising skeletal muscles of the cervical spine.3
The fascial spaces of the neck can further be classified into suprahyoid and infrahyoid spaces.2
The suprahyoid spaces include:
- Masticator space
- Pyteromandibular space
- Superficial temporal space
- Deep Temporal space
- Submandibular space
- Submental space
- Sublingual space
- Lateral pharyngeal (parapharyngeal space)
The infrahyoid spaces (Figure 1) include:
- Pretracheal space
- Perivertebral space
- Carotid space
- Retropharyngeal space
- Danger space
The most common sites for deep space infections include the submandibular space, the masticator space, the parapharyngeal space and the retropharyngeal space.
Infections related to neck anatomy
Parapharyngeal and peritonsillar space infection
The parapharyngeal space is an inverted cone-shaped space with the base being the skull base and the apex being the hyoid bone.1 It is divided into anterior and posterior compartments by the styloid process.
Parapharyngeal space abscess formation usually occurs as a complication of tonsillitis, dental infections or supraglottitis.1 Infection usually spreads by direct extension from the peritonsillar space.
The parapharyngeal space communicates directly with the retropharyngeal space and the submandibular space.1
A peritonsillar abscess is also known as a “quinsy”. Infection develops between the lateral aspect of the tonsil and the medial aspect of the superior constrictor muscle. For more information, see the Geeky Medics guide to peritonsillar abscess.
Retropharyngeal space infection
The retropharyngeal space extends from the base of the skull to the posterior mediastinum.2
Retropharyngeal abscesses/infections are more commonly seen in children as upper respiratory tract infections seed in the retropharyngeal lymph nodes. The retropharyngeal lymph nodes usually regress by the age of 5.2
Retropharyngeal abscesses in adults are less common and usually caused by trauma or direct extension from cervical spinal discitis or osteomyelitis.
Submental & submandibular spaces (Ludwig’s angina)
Ludwig’s angina is gangrenous cellulitis of the floor of the mouth which usually involves the three compartments of the floor of the mouth including submental, sublingual and submandibular tissues bilaterally.3
The most common source of infection is odontogenic (dental infection) and classically starts with infection of the 2nd or 3rd mandibular molars.
Cervical necrotising fasciitis
This is a rapidly progressive infection of the superficial tissues and fascia caused by toxins released by bacteria.4 The toxins cause localised necrosis of the subcutaneous tissue and fascial planes. Cervical necrotising fasciitis is rare but carries a very high morbidity and mortality rate. It can develop as a result of a deep space neck infection.
Pathophysiology
Infection usually spreads to the deep space areas of the neck via direct extension.5 This includes oropharyngeal infections such as tonsillitis, dental infections or from skin infections.6 Direct primary extension from the oral cavity is demonstrated in tonsillitis in children and dental infections in adults. Neck trauma (both blunt and penetrating) can also introduce infection in the deep space neck regions.5
Infection can also be caused by lymphatic spread from the oral cavity.
Cellulitis occurs which then develops into a phlegmon (acute inflammation of soft tissue) which if left untreated develops into an abscess.6
Cervical lymphadenitis is the most common cause of deep space neck infections in children where infection suppurates in retropharyngeal or parapharyngeal lymph nodes.5 The most common cause in adults is tonsillar or dental pathology.5
Causative organisms
Deep space neck infections are usually polymicrobial with streptococci, staphylococcus aureus and anaerobes being the most common causative organisms.6
Anaerobic bacteria are usually the causative organism in infections of dental origin with Streptococcus usually the causative organism in infections of pharyngo-tonsillar origin.5
Staphylococcus aureus is highly prevalent in deep space neck infections in children whereas Klebsiella pneumoniae is more commonly seen in diabetic patients.5
Risk factors
Risk factors for deep neck space infections include:
- Male
- Recurrent tonsillitis/peri-tonsillar abscesses
- Active smoker
- Poor oral hygiene/poor dentition
- Intravenous drug use
- Immunocompromise: long-term steroid use/HIV (increased risk of multiple or more extensive deep space neck infection)
- Type 2 diabetes mellitus
Clinical features
History
Typical symptoms of deep space neck infections include:
- Fever
- Throat pain
- Dysphagia/odynophagia
- Neck swelling
- Chest pain
Other important areas to cover in the history include:
- Social history: including smoking status
- Past medical history: recurrent throat infections and previous hospitalisations for neck infections
- Drug history: immunosuppressant medication including long-term steroid use
- Travel history: recent overseas travel
Clinical examination
Typical clinical findings in deep neck space infections include:
- Trismus
- Torticollis
- Floor of mouth swelling
- Cervical lymphadenopathy
- Drooling
A thorough oropharyngeal examination should be performed. This may show tonsillar enlargement or bulge of the peritonsillar space. Halitosis and trismus may also be noted.
Examination of the neck may identify cervical lymphadenopathy, a palpable fluctuant mass and reduced range of movement
Flexible nasal endoscopy (FNE)
Flexible nasal endoscopy involves the insertion of a flexible camera to visualise the laryngeal inlet and larynx. Asymmetrical bulging of the pharyngeal wall indicates the presence of a collection. Stenosis of the laryngeal inlet may indicate impending airway compromise.
Investigations
Laboratory investigations
Relevant laboratory investigations include:
- Full blood count: white cell count may be raised
- CRP: raised in the acute inflammatory response phase
- Urea and electrolytes: may show evidence of acute renal failure secondary to sepsis or dehydration
- Blood cultures: both aerobic and anaerobic to assess for the presence of a resultant bacteraemia
Imaging
Relevant imaging investigations include:5
- Lateral neck X-ray: helpful in young children to assess for a retropharyngeal abscess. They are better tolerated by children and avoid radiation from CT imaging.
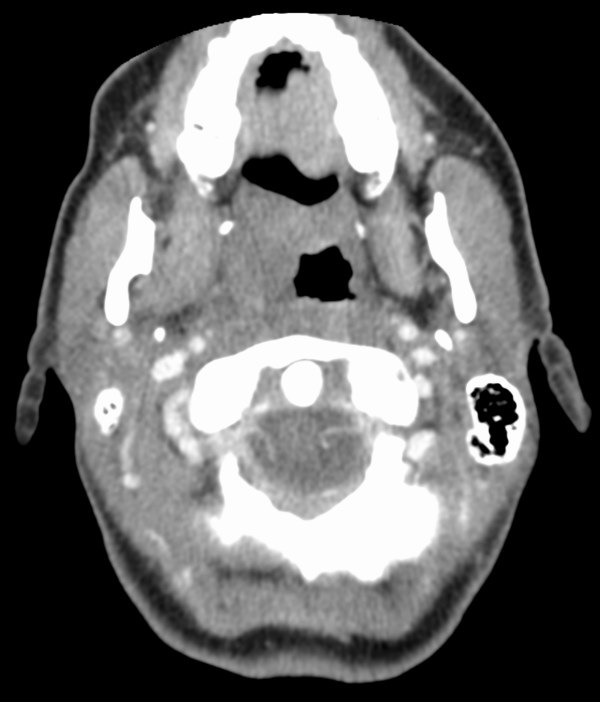
- CT neck with contrast (Figure 2): helps identify abscess formation by highlighting rim enhancement and central necrosis. This helps with pre-operative planning if incision and drainage are required.
- CT chest with contrast: usually performed at the same time as the CT neck, this helps to identify any extension of infection into the mediastinum (i.e. mediastinitis/mediastinal collection).
- Ultrasound neck: helpful when combined with percutaneous drainage if the abscess/collection is small, superficial and accessible. It has a very limited role in true deep space neck infections as it offers poor visualisation of these areas.
Management
Immediate management
Deep space neck infections are potentially life-threatening and require immediate assessment due to the risk of airway compromise. A full ABCDE assessment should be performed and the patient cared for in a monitored resuscitation bay.
Airway assessment is critical and patients may require their airway securing immediately if there is any evidence of compromise. Anaesthetic and ENT surgical teams should be informed.
Broad spectrum intravenous antibiotics should be administered based on local anti-microbial prescribing guidelines.
If the patient is stable, a CT neck and chest with contrast should be considered for further assessment and to guide management. Admission to intensive care or a high dependency unit may be required for airway monitoring or vasopressor support.
Non-operative management
Non-operative management (with broad-spectrum antibiotics) is considered for abscesses <2.5cm in diameter or if there is an inflammatory reaction but no evidence of a frank abscess on imaging.5
An ultrasound neck with percutaneous drainage can be considered if the collection is accessible.
The patient should be closely monitored and undergo repeat imaging if there is no clinical or biochemical improvement.
Surgical management
If a CT scan shows an abscess >2.5cm in diameter the patient will usually require surgical exploration with incision and drainage.
Surgical approaches include:1
- Transoral approach: ipsilateral tonsillectomy with deroofing of the abscess/collection and drainage of purulent material from the parapharyngeal space.
- Transcervical approach: incision over the area of maximum fluctuance or a ‘hockey stick’ incision. Loculations and the abscess capsule are broken down. Drains may be inserted to allow ongoing purulent material to be evacuated.
If there is evidence of a mediastinal collection or abscess then the patient should be referred to the cardiothoracic surgical team for assessment.
Complications
Complications of deep space neck infections include:
- Sepsis
- Acute airway obstruction: some patients require tracheostomy
- Mediastinitis/mediastinal abscess: infection tracts inferiorly from the neck
- Lemierre’s syndrome: thrombophlebitis of the internal jugular vein
- Carotid artery aneurysm
Key points
- Deep neck space infections refer to infection or abscess formation in the deep tissues, fascial planes and potential spaces in the neck
- An understanding of the underlying anatomy combined with a knowledge of red flag features and risk factors is required
- Cross-sectional imaging (usually CT) should be undertaken promptly if there is clinical suspicion of a deep neck space infection
- Deep space neck infections are potentially life-threatening and require immediate assessment due to the risk of airway compromise
- Management of deep space neck infections includes airway management, broad-spectrum antibiotics and surgical drainage of any abscess
- Complications include sepsis, airway obstruction, mediastinal involvement (requiring cardiothoracic input) and vascular complications.
Reviewer
Mr Tom Paterson
ST6 ENT Registrar
Queen Elizabeth University Hospital, Glasgow
Editor
Dr Chris Jefferies
References
- Watkinson J, Clarke R, Paleri V et al. Neck space infections In: Scott-Brown’s otorhinolaryngology head and neck surgery. 8th ed. Vol 3. CRC Press;2019:p623-631
- Van Gijn D, Dunne J. The Neck In: Oxford Handbook of head and neck anatomy. 1st ed. OUP;2022:p186-195
- Corbridge R, Steventon N. Anatomy of the Neck In: Oxford Handbook of ENT and Head and Neck Surgery. 3rd ed. OUP;2020:p278-281
- Grisaru-Soen G, Komisar O, Aizenstein O et al. Retropharyngeal and parapharyngeal abscess in children—Epidemiology, clinical features and treatment. Int J Pediatr Otorhinolaryngol 2010;74:1016-1020
- Sethi N, Pearson A, Bajaj Y. Key clinical topics in otolaryngology. 1st Jaypee Medical Publishing 2016. 203-207
- Vallee M, Gaborit B, Meyer J et al. Ludwig’s Angina: a diagnostic and surgical priority. Int J Infect Dis 2020;93:160-162
- Rajak S, Figueira E, Haridas A et al. Periocular necrotising fasciitis: a multicentre case series. Br J Ophthalmol 2016;100:1517-1520
- Gujrathi A, Ambulgekar V, Kathait P. Deep space neck infection-A retrospective study of 270 cases at tertiary care center. World J Otorhinlaryngol Head Neck Surg 2016;2:208-213
Image references
- Nadezdha D. Kiriyak. Infrahyoid deep neck spaces. License: [CC BY]
- James Heilman, MD. Peritonsillar Abscess. License: [CC BY]




