- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A hydrocele is a common cause of scrotal swelling. It results from the collection of excess fluid in the potential space between the parietal and visceral layers of the tunica vaginalis lining of the testes.1
Aetiology
Paediatric hydrocele
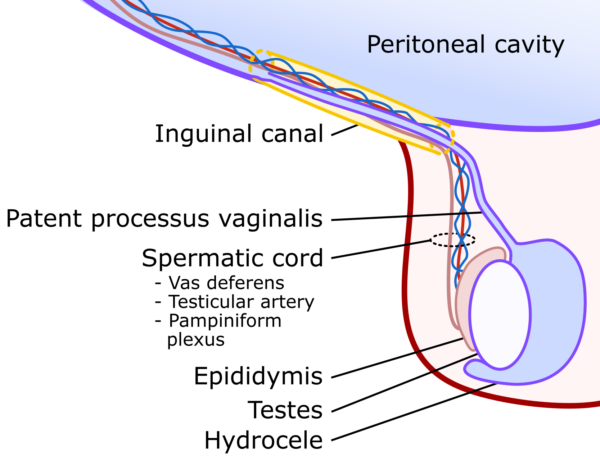
Towards the end of foetal development, the testes descend from their intra-abdominal position, through the inguinal canal and into the scrotum. They travel within an outpouching of peritoneum called the processus vaginalis. This forms the peritoneal lining of the testicle, becoming the tunica vaginalis.
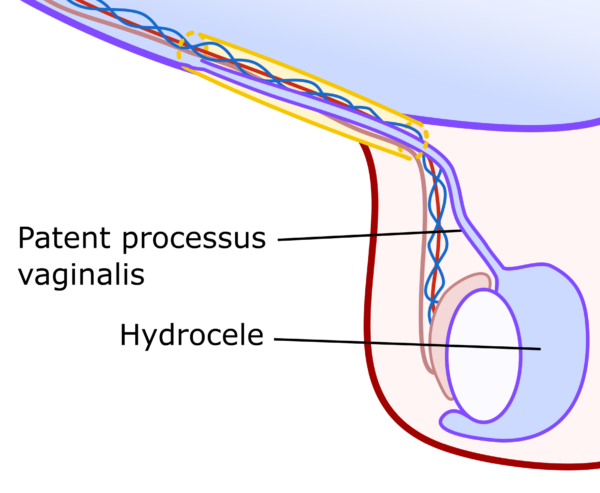
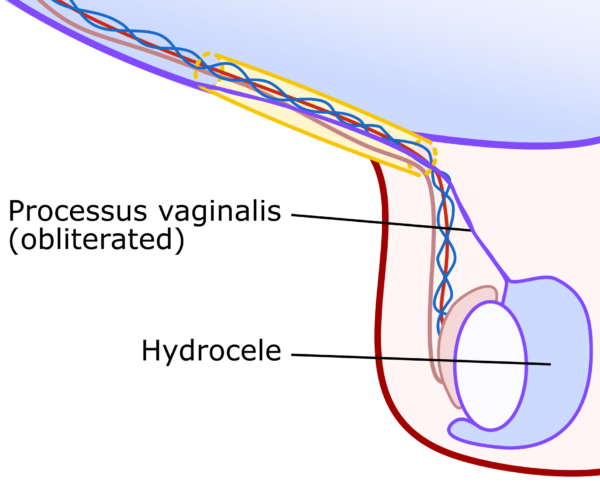
The tunica vaginalis has a visceral layer around the testicle and a parietal layer reflected within the scrotum, with a small amount of physiological fluid in the potential space between. The remainder of the processus vaginalis obliterates, leaving no connection between the peritoneal cavity and the testes.2 This is shown below in Figure 1.
Paediatric hydroceles are normally congenital as a result of a failure of the processus vaginalis to obliterate correctly.
When the processus vaginalis remains open, it leaves a connection between the peritoneal cavity and scrotum, which is termed a patent processus vaginalis (PPV). It is common for the processus vaginalis to be patent at the time of birth. However, the majority will close within the first two years of life.3
A PPV can allow peritoneal fluid to drain from the abdomen to the space around the testes, causing a hydrocele. Additionally, the patent connection can allow abdominal contents to descend through the inguinal canal, causing an associated congenital (indirect) inguinal hernia.
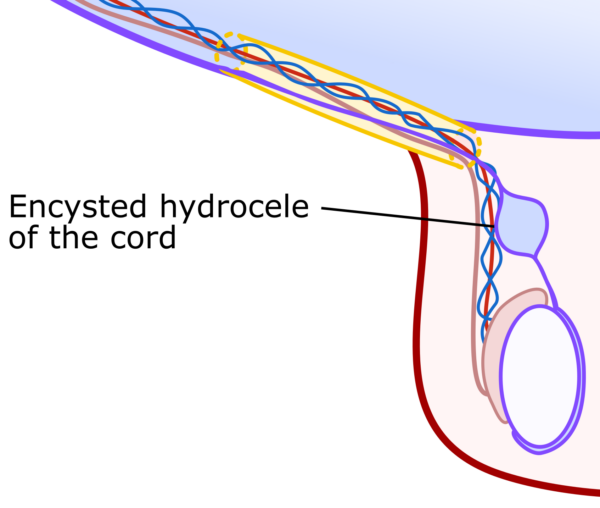
Incomplete obliteration of the processus vaginalis leaving a pocket of fluid at some point along the tract can also occur and is termed an ‘encysted hydrocele of the cord’.2 Examples of a patent processus vaginalis with associated hydrocele and hydrocele of the cord are seen in Figures 2a and 2b, respectively.
Adult hydrocele
These can be primary (idiopathic) or secondary (reactive). The former typically increases slowly over several years and is thought to result from an imbalance between production and reabsorption of fluid within the tunica vaginalis.
A secondary hydrocele occurs in response to an insult to the testicle, such as infection (epididymoorchitis), trauma, and rarely testicular tumour or filariasis.4,5 This type of hydrocele is non-communicating and is illustrated in Figure 3.
Clinical features
History
In children, it is useful to know whether the swelling fluctuates in size to help determine whether the hydrocele is communicating or non-communicating.
If a child has a patent processus vaginalis (causing a communicating hydrocele) then the swelling typically increases in size during the day as peritoneal fluid drains into the scrotum with gravity and reduces at night when the child lays horizontally.2
In adults the course of the swelling may hint at the aetiology, whether it occurred following an episode of infection or trauma (secondary hydrocele) or whether it has been gradually increasing over longer period (primary hydrocele).5
Clinical examination
Hydroceles are scrotal swellings that can vary in size. Larger hydroceles can encroach on the contralateral side and extend into the ipsilateral inguinal canal. They are typically painless unless there is an ongoing pathology, such as epididymo-orchitis.5
The swelling is usually smooth and can feel firm or hard due to the tense collection of fluid rather than fluctuant.
Hydroceles usually transilluminate, whereas hernias do not. However, this does not apply to neonatal hernias, which can also transilluminate. Unlike a hernia, you should be able to get above a hydrocele, though in large hydroceles extending into the canal, this isn’t always obvious to appreciate.
The underlying testicle in a hydrocele is usually impalpable. This is something to be mindful of as a small number of testicular tumours can present with an associated hydrocele.
For more information, see the Geeky Medics guide to testicular examination.
Differential diagnoses
Indirect inguinal hernia
This is associated with a patent processus vaginalis and can occur concurrently with hydrocele. Hernias typically have a history of reducibility unless they are incarcerated.
Incarcerated hernias are generally painful and may be associated with bowel obstruction.
Encysted hydrocele of the cord
This presents as a swelling separate from the testes that can occur anywhere in the line of the processus vaginalis, including the inguinal canal.
Testicular tumour
Testicular cancer can feel hard and swollen like a hydrocele, or cause a reactive hydrocele if they invade through the tunica albuginea.5
Investigations
Hydrocele is often a clinical diagnosis, though the following investigations can be useful.
Laboratory investigations
Whilst not specifically indicated, blood tests can be useful to look for an ongoing underlying cause, where suspected, e.g. inflammatory markers in acute epididymo-orchitis or tumour markers in suspected testicular cancer.
Scrotal ultrasound
Ultrasound is useful to confirm the diagnosis and assess the underlying testicle, which is often not reliably felt due to the hydrocele. Ultrasound can rule out testicular tumours and assess for concurrent inguinal hernia.6
Management
Paediatrics
Conservative management is usually undertaken in children under 12 months, as most will resolve spontaneously.
A persistent or enlarging hydrocele would warrant referral to paediatric surgeons for consideration of surgical repair. In children with a suspected communicating hydrocele due to a PPV this would be a ligation and division of the processus vaginalis, normally undertaken via a groin approach.2
Adults
Conservative management
Unless a sinister underlying cause is present, hydroceles are benign and hence small, asymptomatic hydroceles do not require treatment. Larger hydroceles, however, can be uncomfortable and unsightly, and patients are often keen for intervention in these cases.
Aspiration
Using a needle to aspirate the fluid off the hydrocele is no longer recommended as the hydrocele quickly reoccurs, and the procedure introduces a risk of infection.
Surgical repair
This aims to drain the hydrocele and prevent recurrence. It is performed through a scrotal incision (transverse or midline), usually under a general or regional anaesthetic. Two eponymous techniques are generally used:7,8
- Lord’s plication: this involves opening and draining the hydrocele and plicating (bunching up with sutures) the excess tunica vaginalis. This tends to be used for smaller hydroceles.
- Jaboulay procedure: this involves opening and draining the hydrocele and excising the excess tunica vaginalis. This is more commonly used in larger hydroceles or those with thickened tunica vaginalis.
Complications
All operations carry the risk of complications. The surgical risks for hydrocele repair in adults are shown below.8
- Common: postoperative discomfort/swelling/bruising, bulky feeling testicle, due to the bunched-up tunica vaginalis
- Uncommon: bleeding (resulting in scrotal haematoma) – rarely this requires a surgical evacuation, infection – rarely resulting in abscess requiring a surgical drainage
- Rare: recurrence of hydrocele, chronic scrotal pain
The Lord’s procedure has been shown to have a lower rate of bleeding as there is no excision.8
Key points
- Hydrocele is a benign cause of scrotal swelling due to fluid accumulation within the layers around the testicle.
- In children, this can be due to a patent processus vaginalis, a persistent connection between the peritoneal cavity and scrotum.
- In adults, this is either idiopathic or secondary to other causes such as trauma, infection or, rarely, tumour.
- Scrotal ultrasound is the best way to evaluate scrotal swellings, confirm the diagnosis and look for any underlying causes.
- If conservative management has failed, surgery is the mainstay of treatment.
- Surgery is used to drain and prevent recurrence of the hydrocele and the two common procedures are Lord’s or Jaboulay.
Editor
Dr Chris Jefferies
References
- Dagur G, Gandhi J, Suh Y, Weissbart S, Sheynkin YR, Smith NL, Joshi G, Khan SA. Classifying Hydroceles of the Pelvis and Groin: An Overview of Etiology, Secondary Complications, Evaluation, and Management. Curr Urol 2017;10(1):1-14.
- Patoulias I, Koutsogiannis E, Panopoulos I, Michou P, Feidantsis T, Patoulias D. Hydrocele in Pediatric Population. Acta Medica (Hradec Kralove) 2020;63(2):57-62.
- Brainwood M, Beirne G, Fenech M. Persistence of the processus vaginalis and its related disorders. Australas J Ultrasound Med 2020;23(1):22-9.
- Otabil KB, Tenkorang SB. Filarial hydrocele: a neglected condition of a neglected tropical disease. J Infect Dev Ctries 2015;9(5):456-62.
- Reynard, J., Brewster, S. F., Biers, S., & Neal, N. L. (2019). Oxford handbook of urology (4th ed.). Oxford University Press.
- Valentino M, Bertolotto M, Ruggirello M, Pavlica P, Barozzi L, Rossi C. Cystic lesions and scrotal fluid collections in adults: Ultrasound findings. J Ultrasound 2011;14(4):208-15.
- Rioja J, Sánchez-Margallo FM, Usón J, Rioja LA. Adult hydrocele and spermatocele. BJU Int 2011;107(11):1852-64.
- Tsai L, Milburn PA, Cecil CL, Lowry PS, Hermans MR. Comparison of Recurrence and Postoperative Complications Between 3 Different Techniques for Surgical Repair of Idiopathic Hydrocele. Urology 2019;125:239-42.