- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Bowel obstruction describes the partial or complete blockage of the intestines, leading to a disruption in the normal passage of stool and gas. There is build-up proximal (before) to the obstruction, which causes proximal bowel dilatation and distal bowel collapse.
Bowel obstruction may occur in the small intestine (small bowel obstruction, SBO) or large intestine (large bowel obstruction, LBO) and can be classified into two main types:
- Mechanical obstruction: due to a physical blockage within the intestine
- Functional obstruction (i.e. pseudo-obstruction): due to impaired peristalsis (the normal coordinated movement of the bowel) with no physical blockage
Closed-loop obstruction
Closed-loop obstruction occurs when there is an obstruction at two different points along the same loop of bowel, effectively isolating a section of the bowel.
Closed-loop obstruction is a surgical emergency as the closed-loop will continue to distend and is at high risk of ischaemia and perforation.
Large bowel obstruction with a competent ileocaecal valve also creates a closed-loop picture.
Aetiology
Mechanical obstruction
The most common causes of mechanical bowel obstruction are:1
- Adhesions
- Hernias
- Tumours
Causes of mechanical obstruction can be divided extrinsic (outside of the bowel wall), mural (affecting the layers of the bowel wall) or intraluminal (within the bowel lumen).
Table 1. Causes of mechanical bowel obstruction
| Location | Causes |
| Extrinsic | |
| Mural |
|
| Intraluminal |
|
Functional/pseudo-obstruction
The exact cause of pseudo-obstruction is unknown, but it is thought to be related to impairment of the autonomic nervous system.2
Pseudo-obstruction may occur in patients with:3
- Infection and sepsis
- Injury or physical trauma
- Postoperative
- Cardiovascular disease: myocardial infarction, heart failure, stroke
- Metabolic disturbance: electrolyte imbalance, diabetic ketoacidosis
- Neurological disease: Parkinson’s disease, Alzheimer’s, multiple sclerosis
- Medications: opiates, anti-depressants
Acute pseudo-obstruction is also referred to as Ogilvie’s syndrome.
Clinical features
History
Typical symptoms of bowel obstruction include:
- Colicky, cramp-like abdominal pain
- Abdominal bloating
- Nausea and/or vomiting
- Absolute constipation/obstipation (no flatus or stool)
Other important areas to cover in the history include:
- Features suggestive of malignancy: anaemia, altered bowel habit, rectal bleeding, weight loss
- History of previous abdominal surgery, inflammatory bowel disease, diverticulitis or appendicitis
Clinical examination
Typical clinical findings on abdominal examination may include:
- Abdominal distension
- Generalised abdominal tenderness
- High-pitched or tinkling bowel sounds (early obstruction)
- Absent bowel sounds (late obstruction)
- Evidence of underlying cause: scars from previous surgery, obvious hernia
Typical findings on rectal (PR) examination may include an empty rectum or obstructing mass.
Presentations related to complications
Patients with bowel obstruction may develop complications and present with clinical features related to these complications.
Complications and related clinical features may include:4,5
- Bowel ischaemia: pain out of proportion to clinical examination, fever, tachycardia
- Bowel perforation with peritonitis: severe abdominal pain, abdominal guarding, rebound and percussion tenderness
- Perforation with intra-abdominal abscess: abdominal pain, fever, possible palpable mass
- Sepsis & multi-organ failure
- Electrolyte derangement: confusion & irritability, arrhythmia, nausea, fatigue
- Aspiration pneumonia: shortness of breath, productive cough, fever
Differential diagnoses
Possible differential diagnoses in the context of abdominal pain and vomiting include:
- Gastroenteritis
- Bowel ischaemia
- Acute pancreatitis
- Bowel perforation
- Acute appendicitis
Non-gastrointestinal conditions such as myocardial infarction, renal colic or ovarian torsion.
Investigations
Bedside investigations
Relevant bedside investigations include:
- Basic observations (vital signs)
- Pregnancy test: exclude ectopic pregnancy as cause for abdominal pain in females of childbearing age
Laboratory investigations
Relevant laboratory investigations include:
- Full blood count: raised white cell count
- Urea & electrolytes: vomiting may cause deranged renal function and electrolyte disturbance
- CRP & lactate: suggestive of bowel ischaemia
- Group & save: pre-operative
Imaging
Relevant imaging investigations include:
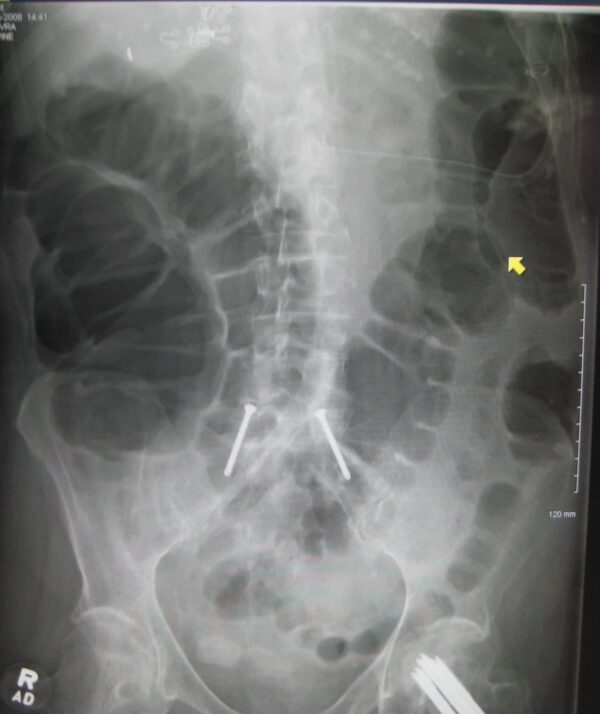
- Abdominal X-ray: may demonstrate signs of bowel obstruction, including dilated bowel loops with air-fluid levels
- CT abdomen & pelvis with IV contrast: the standard of care to confirm the diagnosis and assess the anatomical site, severity, underlying aetiology and complications
Small bowel vs large bowel obstruction on abdominal X-ray
Abdominal X-ray interpretation can be challenging in bowel obstruction, and a normal X-ray does not exclude obstruction. However, characteristic findings help to differentiate small bowel versus large bowel.
Table 2. Differentiating features of small and large bowel on abdominal X-ray.
| Feature | Small bowel | Large bowel |
| Location | Central | Peripheral |
| Diameter | >3cm |
Colon >6cm Caecum >9cm |
| Mucosal folds | Valvulae conniventes – stretch across the whole diameter of bowel loops | Haustra – stretch part-way across the diameter of bowel loops |
| Intra-luminal gas | Usually minimal | Mixture of gas and faeces (mottled appearance) |
Management
Initial management
Following resuscitation, initial supportive care consists of:
- Nil-by-mouth (NBM): bowel rest to reduce peristalsis
- Intravenous fluids: maintain hydration and correct any electrolyte disturbance
- Nasogastric tube with free drainage: decompress bowels, relieves abdominal distension and vomiting and reduces the risk of aspiration
- Urinary catheter: monitor urine output and fluid balance
- Analgesia
- Antibiotics: if septic
‘Drip and suck’
The initial measures for managing bowel obstruction are colloquially referred to as ‘drip and suck’:
- Drip: intravenous fluids
- Suck: nil-by-mouth and nasogastric tube insertion
Definitive management
Subsequent treatment depends upon the aetiology, location of obstruction and patient co-morbidities:3,6,7
- Adhesions: water-soluble contrast study (gastrografin)
- Sigmoid volvulus: endoscopic decompression with flexible sigmoidoscopy to allow for semi-elective surgery or as the only treatment in high-risk patients
- Left-sided bowel tumour: endoscopic stenting as a bridge to surgery or palliation
- Stricture: endoscopic dilatation or placement of stent
- Pseudo-obstruction: correct electrolyte abnormalities, discontinue anti-kinetic drugs, treat the underlying cause
Indications for emergency surgery
Emergency surgery is indicated in patients with:4,5
- Suspicion of complicated bowel obstruction: perforation or ischaemia
- Closed loop obstruction
- Strangulated hernia
- Obstructing tumour: if not amenable to stenting
- Failure of non-operative treatment: usually after 72 hours
Key points
- Mechanical bowel obstruction is most often caused by adhesions, hernias or tumours and can affect the small or large bowel
- Typical symptoms include colicky abdominal pain, abdominal distension, nausea and vomiting and absolute constipation
- Typical signs include abdominal distension, generalised abdominal tenderness and high-pitched or absent bowel sounds
- Bowel obstruction is confirmed using a CT of the abdomen & pelvis with contrast
- Initial management is with ‘drip & suck’, nasogastric tube and intravenous fluids in addition to nil-by-mouth and urinary catheter for monitoring fluid balance
- Management with surgery indicated in the case of complications, closed-loop obstruction or failed conservative management
- Complications include bowel ischaemia, perforation, electrolyte derangement and aspiration pneumonia
Reviewer
Mr Oddai Alkhazaaleh
Consultant General and Upper GI Surgeon
Editor
Dr Chris Jefferies
References
- World Journal of Emergency Surgery. Bowel obstruction: a narrative review for all physicians – Causes of bowel obstruction in adults. Published in 2019. Available from: [LINK]
- Patient UK. Intestinal Obstruction and Ileus. Published in 2020. Available from: [LINK]
- Medical Clinics of North America. Dynamic Ileus and Acute Colonic Pseudo-Obstruction. Published in 2008. Available from: [LINK]
- BMJ Best Practice. Small bowel obstruction. Published in 2021. Available from: [LINK]
- BMJ Best Practice. Large bowel obstruction. Published in 2023. Available from: [LINK]
- UpToDate. Large bowel obstruction. Published in 2023. Available from: [LINK]
- UpToDate. Management of small bowel obstruction. Published in 2022. Available from: [LINK]
Image references
- Figure 1. Geeky Medics. Small bowel obstruction
- Figure 2. James Heilman, MD. Large bowel obstruction. Licence: [CC BY-SA]