- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Diverticula are mucosal out-pouches in the colonic musculature. The presence of diverticula without symptoms is called diverticulosis.
Diverticular disease is symptomatic diverticula with no inflammation or infection. When these diverticula become inflamed, this results in diverticulitis.
Left-sided colonic diverticula (within the sigmoid and descending colon) are a feature of Western diets. Approximately 15% of cases involve right-sided diverticula (within the ascending colon) and are more common among patients of Asian descent, likely representing congenital diverticulae.1,2,3
This article will cover the clinical presentation, investigation and management of diverticulitis.
Aetiology
Diverticula occur when there is high intraluminal pressure within the bowel, which causes thinning of the bowel wall. Pouches of mucosa push through and develop into an outpouch (Figure 1).
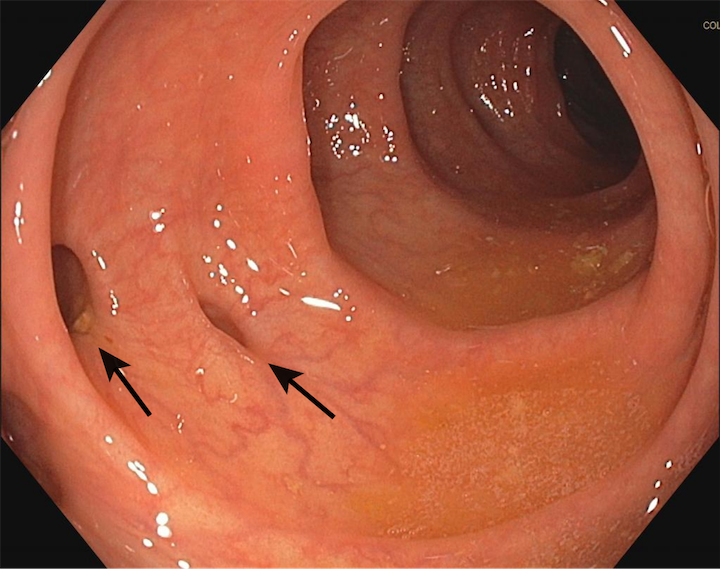
Inflammation is believed to be caused by bacterial overgrowth and translocation through the colonic mucosa, but the exact aetiology is unknown.4
Risk factors
Risk factors for diverticulosis and diverticulitis include:1,2
- Older age: in adults older than 85, 80% have diverticulosis
- Low-fibre diet (usually Western diets)
- Smoking
- Obesity
- Medication: NSAIDs and opioids increase the risk of perforated diverticulitis
Clinical features
History
Typical symptoms of diverticulitis include:
- Abdominal pain: most commonly in the left lower quadrant
- Change in bowel habit: diarrhoea or constipation
- Rectal bleeding
- Bloating
- Nausea and vomiting
- Anorexia
Clinical examination
Typical clinical findings of diverticulitis include:
- Tender abdomen +/- guarding
- Tachycardia
- Fever
Clinical features of complications
Patients with diverticulitis may develop complications and present with clinical features related to these complications.
Complications and related clinical features may include:1,2
- Abscess: tender mass on abdominal palpation, ongoing fever despite antibiotics
- Perforation leading to peritonitis: severe abdominal pain, abdominal guarding, rebound and percussion tenderness
- Sepsis: tachycardia, tachypnoea, hypotension, oligo/anuria or altered GCS
- Fistulation: can affect any abdominal organ or the skin (e.g. colovesicular and colovaginal fistula); clinical features vary but may include faecaluria, pyuria, or faecal leakage through the vagina
- Obstruction: inflammation leads to fibrosis and stricturing; features include abdominal pain, distension, vomiting and absolute constipation
- Bleeding: rectal bleeding, which can vary from minor to life-threatening, may require transfusion
Differential diagnoses
It can be helpful to group differentials of acute abdominal pain by organ system. The main gastrointestinal conditions to consider include:
- Inflammatory bowel disease
- Ischaemic colitis
- Colorectal cancer
- Irritable bowel syndrome
- Appendicitis
The sigmoid colon is mobile within the abdomen and may move to the right iliac fossa. This may mimic other conditions, such as appendicitis.
Gynaecological and urological differentials such as ectopic pregnancy, ovarian pathology or renal/ureteric stones are also important to consider.
Investigations
Investigations should be guided by clinical judgment according to the severity of the patient’s presentation (e.g. sepsis six if unwell and septic).
Bedside investigations
Relevant bedside investigations may include:
- Basic observations (vital signs): to ensure the patient is haemodynamically stable.
- Urinalysis: to exclude urological causes of abdominal pain (e.g. UTI)
- Urine pregnancy test: to exclude ectopic pregnancy in female patients of childbearing age
Laboratory investigations
Relevant laboratory investigations may include:1,2
- Full blood count: raised white cell count (indicates inflammation), anaemia (due to bleeding)
- Urea & electrolytes: baseline renal function and to identify renal impairment (important before contrast scans)
- CRP: raised in inflammation
- Group & save: before any surgical intervention
Imaging
Relevant imaging may include:2
- CT abdomen and pelvis with contrast: if contraindicated (e.g. AKI), then a non-contrast CT scan can be requested
Management
Diverticulitis treatment is dictated by its severity. Complications such as perforation, abscess formation or peritonitis indicate complicated diverticulitis. Patients without complications have non-complicated diverticulitis.
Medical management
Uncomplicated diverticulitis can be managed as an outpatient without antibiotics if there is no evidence of complications, comorbidities or immunosuppression. They should be followed up after the flare.4
Patients should receive antibiotics for acute episodes of complicated diverticulitis. Depending on the severity, this could be oral or intravenous. Co-amoxiclav for five days is commonly used for acute diverticulitis. Those with penicillin allergies may receive co-trimoxazole and metronidazole (always refer to local guidelines).
IV fluid should be considered if the patient appears dehydrated or is nil-by-mouth before surgery.1,4
Analgesia should be used and titrated as per the WHO pain ladder.
Surgical management
Most patients will be managed medically. However, surgical intervention may be required if this fails or complications occur.
Those with a fistula or persistent abscesses should also be assessed for surgical intervention. This can be either an open or laparoscopic resection, with the decision being made by the responsible consultant.
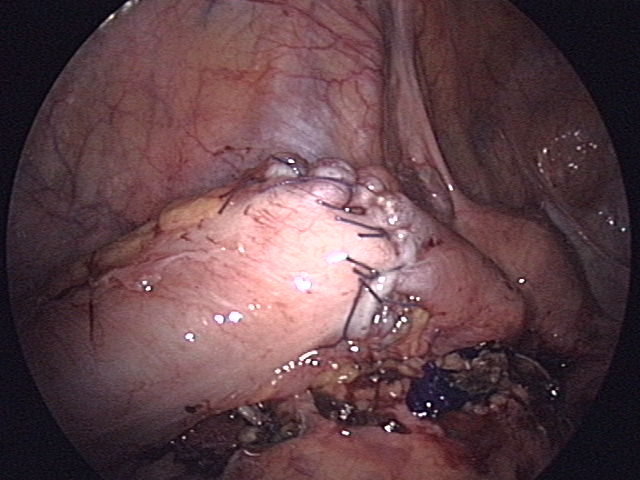
Treatment of peritonitis is divided into its causes (purulent vs faeculant). Patients with purulent peritonitis may be managed by laparoscopic lavage or resection, whereas faeculant peritonitis should be treated with colonic resection.
Hartmann’s procedure
This involves a sigmoid colectomy and the formation of an end colostomy. An anastomosis and colostomy reversal can be performed once the patient has recovered from the acute illness. This carries a high risk and may not be completed in every patient.5
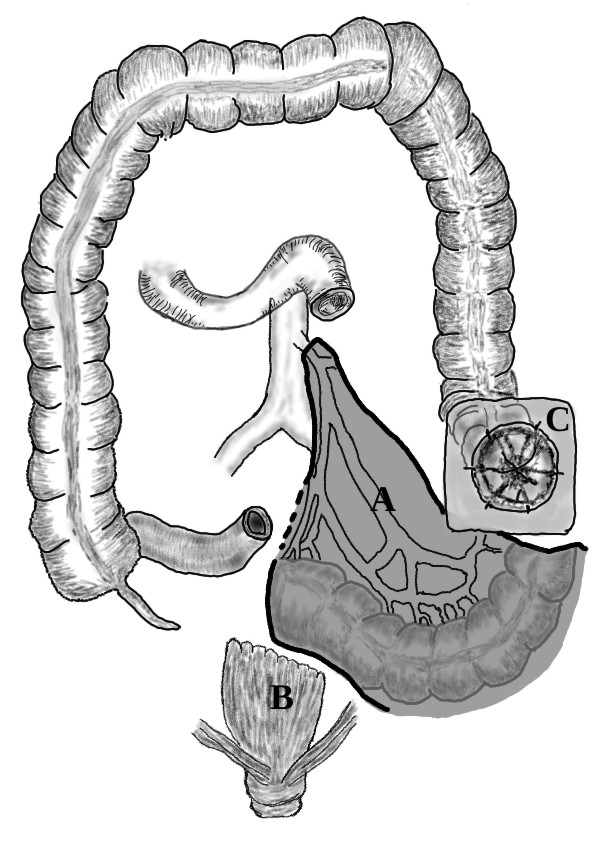
Primary anastomosis
This procedure involves resecting the diseased bowel (i.e. sigmoid colectomy) and forming an anastomosis between a healthy proximal margin and the rectum. A loop ileostomy may be used short-term if the surgeon is concerned about anastomotic breakdown.
Diverticular abscesses
Diverticular abscesses can be managed medically with antibiotics, surgically or by radiological percutaneous drainage.
Percutaneous drainage is guided by CT or ultrasound. A drain is inserted and allows the abscess to drain. Typically, abscesses larger than 3 cm are considered for drainage.4
Follow-up
Colonoscopy can determine the extent of diverticulosis and exclude other conditions, such as colorectal cancer and IBD. It is performed at least six weeks after the episode. It should not be done in acute diverticulitis due to the risk of perforation.1,4
CT colonography is an imaging technique used when colonoscopy is contraindicated.1,4
Management of diverticular disease
Diverticular disease can be managed with a high-fibre diet, good oral fluid intake and bulk-forming laxatives.2 Patients should be advised to avoid NSAIDs (e.g. ibuprofen) due to the risk of perforation.1,4
Appropriate safety netting advice should be given, with patients advised to seek advice if symptoms do not improve or worsen.
Complications
Complications of diverticulitis include:
- Abscess formation
- Perforation leading to peritonitis
- Sepsis
- Fistulation
- Bowel obstruction
- Bleeding
Key points
- Diverticulitis is caused by inflammation and infection of diverticula (outpouchings in the colon)
- Most episodes occur on the left side of the abdomen and involve the sigmoid and descending colon
- Typical symptoms include fever, left lower quadrant pain and rectal bleeding
- Typical clinical signs include abdominal tenderness, tachycardia and signs of peritonism
- Diverticulitis is confirmed using a CT of the abdomen & pelvis with contrast
- It can be managed as an outpatient or inpatient with antibiotics, surgery or radiological interventions depending on the severity
- Common complications include perforation, sepsis and bleeding
Reviewer
Miss Hema Sekhar
Colorectal Consultant
Editor
Dr Chris Jefferies
References
- NICE CKS. Diverticular disease. Published in 2022. Available from: [LINK]
- Patient UK. Diverticular disease. Published in 2020. Available from: [LINK]
- NIH. Acute diverticulitis. Published in 2022. Available from: [LINK]
- European Society of Coloproctology. Guidelines for the management of diverticular disease of the colon. Published in 2020. Available from: [LINK]
- PubMed. Hartmann’s procedure or primary anastomosis? Published in 2012. Available from: [LINK]
Image references
- Figure 1. Jmarchn. Diverticulosis. Licence: [CC BY-SA 3.0]
- Figure 2. Anpol42. Hartmanns operation of the colon. Licence: [CC BY-SA 4.0]
- Figure 3. Anpol42. Manual anastomosis of sigmoid colon. Licence: [CC BY-SA 4.0]