- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
An ectopic pregnancy occurs when a fertilised ovum implants outside of the uterus. The most common location for ectopic pregnancy to occur is in one of the fallopian tubes, due to tubal dysfunction.
In the UK, there are approximately 11,000 ectopic pregnancies annually, and the incidence is increasing.1
Aetiology
Ectopic pregnancies are classified by the anatomical site of the implantation of the pregnancy:
- Tubal (usually ampulla): 93%
- Interstitial (implantation in the interstitium where the fallopian tube meets the uterus): 1.1 – 6.3%
- Cervical: 0.15%
- Ovarian: 0.5%
Ectopics can occur in the myometrium when a fertilised ovum implants in a Caesarean section scar. There have been isolated cases of ectopic pregnancies as far afield as the liver.
Risk factors
There is often no identifiable cause for ectopic pregnancy. However, the following risk factors are associated with an increased likelihood of developing the condition:
- Previous ectopic pregnancy (indicating damage to a fallopian tube)
- Assisted reproduction techniques (e.g. in-vitro fertilisation)
- History of pelvic inflammatory disease (resulting in tubal occlusion due to adhesions)
- Endometriosis
- Tubal occlusion from sterilisation*
- Intrauterine contraception*
*Sterilisation and intrauterine contraception considerably decrease the chance of pregnancy. However, if pregnancy occurs, the risk of ectopic pregnancy is increased.
Clinical features
Patients with an ectopic pregnancy usually present with unilateral abdominal pain from 5 weeks of expected gestation onwards. Patients may be unaware of the pregnancy and using contraception.
In some cases, patients may present significantly shocked due to haemorrhage following the rupture of the ectopic pregnancy.
History
Typical symptoms of ectopic pregnancy include:
- Abdominal pain (usually unilateral but can be bilateral)
- Pelvic pain
- Amenorrhoea or a missed period
- Vaginal bleeding (with or without clots)
- Dizziness, fainting or syncope
- Shoulder tip pain
Other important areas to cover in the history include:
- Menstrual history including date of last menstrual period
- Sexual history
- Past medical history (previous gynaecological surgery, endometriosis, IVF
- Medication history: contraceptives, anticoagulants
Clinical examination
In the context of a suspected ectopic pregnancy, a pelvic examination is necessary.
Typical clinical findings in ectopic pregnancy include:
- Pelvic or abdominal tenderness
- Adnexal tenderness
- Vaginal bleeding
- Haemodynamic compromise: if rupture and haemorrhage
Pregnancy testing
Any woman of reproductive potential who presents with abdominal or pelvic pain should always have a pregnancy test. If the pregnancy test is positive, they have an ectopic pregnancy until proven otherwise.
Investigations
Bedside investigations
Relevant bedside investigations in the context of ectopic pregnancy include:
- Basic observations (vital signs): to assess for haemodynamic compromise
- Urine pregnancy test (hCG urine dipstick): would be positive in ectopic pregnancy.
- Urinalysis: to exclude a urinary tract infection. If findings suggest a urinary tract infection, ectopic pregnancy would still need excluding (as the patient may have both).
- Vaginal swabs: to assess for sexually transmitted infections (which can pre-dispose to an ectopic pregnancy)
Laboratory investigations
Relevant laboratory investigations in the context of ectopic pregnancy include:
- Baseline blood tests (FBC, U&E, coagulation, CRP): white cells may be raised, and there may be anaemia
- Serum hCG: the level will depend on the gestation and viability of the pregnancy. This is often used to monitor response to treatment (see below)
- Group and save: important to perform as the patient may require a blood transfusion
Imaging
Relevant imaging investigations in the context of ectopic pregnancy include:
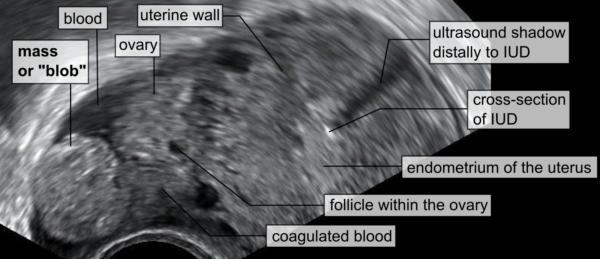
- Transvaginal ultrasound scan: the most accurate method of confirming the presence of tubal ectopic pregnancy
Management
Initial assessment
An ABCDE approach should be followed during the initial assessment and management of patients with suspected ectopic pregnancy. Ectopic pregnancy may present with significant haemodynamic instability requiring resuscitation and blood transfusion.
Definitive management
There are three management options for ectopic pregnancy, depending on the haemodynamic stability of the patient and investigation findings:
- Expectant management
- Medical management
- Surgical management
If the ectopic pregnancy has ruptured, surgical management is usually required.
The decision between expectant and medical management, and medical and surgical management, depends on NICE guidelines and patient preference.
Expectant management
Expectant management involves monitoring serum bHCG and performing serial ultrasound scans to monitor the ectopic pregnancy until it spontaneously resolves (‘watch and wait’ approach).
Expectant management is suitable for women who meet the following criteria:
- Pain-free
- Haemodynamically stable
- Tubal ectopic pregnancy visible on ultrasound measuring <35 mm (and no visible heartbeat)
- Serum hCG <1,000 IU/L*
- Able to return for follow-up
Expectant management can be considered for women who have a serum hCG between 1,000 – 1,500 IU/L, providing they meet the other criteria above.
Medical management
Medical management involves using methotrexate to stop the growth of the ectopic pregnancy and allow resolution to occur.
Medical management is suitable for women who meet the following criteria:
- No significant pain
- Unruptured ectopic pregnancy with an adnexal mass <35 mm (and no visible heartbeat)
- No intrauterine pregnancy is seen on the ultrasound scan: some women may have a heterotopic pregnancy where an intrauterine pregnancy occurs alongside an ectopic pregnancy
- Serum hCG <1500 IU/L*
- Able to return for follow-up
*Women with a serum hCG between 1500 – 5000 may be considered for medical management.
The serum hCG level is monitored to ensure it is declining and not continuing to rise. If serum hCG levels continue to rise, a re-assessment of the management plan should occur.
Surgical management
Surgical management involves the surgical removal of the ectopic pregnancy.
Surgery should be offered to those women who meet any of the following criteria:
- Unable to return for follow-up
- Significant pain
- Adnexal mass ≥35 mm
- Fetal heartbeat visible on the scan
- Serum hCG level ≥5000 IU/L
In cases of tubal ectopics, a laparoscopic salpingectomy is usually performed, removing both the ectopic pregnancy and the fallopian tube.
Anti-D prophylaxis should be given to all rhesus-negative women who undergo surgical management of an ectopic pregnancy.
Surgical management options
Salpingectomy is the removal of the ectopic pregnancy along with the fallopian tube. It is the preferred option in women with no other risks to their fertility, as it reduces the likelihood of a repeat ectopic pregnancy. It can affect future fertility, so women should be carefully counselled about the pros and cons of the procedure.
Salpingotomy is an alternative that seeks to remove the ectopic pregnancy whilst preserving the fallopian tube. It is usually offered to women with other fertility issues, such as damage to the other fallopian tube. It does carry a greater risk of a future ectopic pregnancy than a salpingectomy.
Complications
If an ectopic pregnancy is not diagnosed and treated promptly, complications can include:
- Fallopian tube or uterine rupture
- Secondary massive haemorrhage
- Death
Complications of surgical management can include:
- Bleeding
- Infection
- Damage to local structures (uterus, bladder, bowel, vasculature)
Psychological support
Whilst an ectopic pregnancy is a potentially life-threatening situation for a woman, it is important to also acknowledge that the removal of an ectopic pregnancy also represents the loss of what may be a much-longed-for pregnancy. Women should be offered the same emotional support as anyone who has experienced early pregnancy loss.
For women who have undergone a salpingectomy, there may be further emotional support needed to allow them to come to terms with the potential impact on their future fertility.
The Ectopic Pregnancy Trust website has some useful resources for patients and professionals.
Key points
- An ectopic pregnancy occurs anywhere outside of the uterus.
- The most common location for ectopic pregnancy to occur is in one of the fallopian tubes.
- The most common symptoms include abdominal pain, pelvic pain, amenorrhoea and vaginal bleeding (with or without clots).
- The most common clinical findings include pelvic or abdominal tenderness and adnexal tenderness.
- Urine hCG, serum hCG and abdominal ultrasound are the primary investigations required to confirm the diagnosis.
- Medical management involves the administration of systemic methotrexate, with ongoing monitoring of serum hCG levels.
- Surgical management involves removing the ectopic pregnancy (most commonly a laparoscopic salpingectomy).
- Complications can include fallopian tube rupture, haemorrhage and death.
Reviewer
Dr Ashley Jefferies
Community Sexual and Reproductive Health Registrar
Editor
Dr Chris Jefferies
References
- Goumalatsou, Charlotte, ‘Gynaecology’, in Andrew Baldwin (ed.), Oxford Handbook of Clinical Specialties, 11 edn, Oxford Medical Handbooks (Oxford, 2020; online edn, Oxford Academic, 1 Oct. 2020).
- Mikael Häggström.Blob sign of ectopic pregnancy. License: [Public domain]
- NICE.Ectopic pregnancy and miscarriage: diagnosis and initial management. 2021. Available from: [LINK]