- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
A 54 year old man presents to the emergency department following a collapse. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
- Blackouts and faints
- Decreased/loss of consciousness
History
Presenting complaint
“I was walking the dog today when I suddenly felt funny, the next thing knew, I was on the floor and somebody passing by had called an ambulance.”
History of presenting complaint
Did you have any symptoms before the collapse?
“No, I didn’t notice anything particularly out of the ordinary”
Did you experience any palpitations or chest pain?
“No, I don’t believe so”
Did you lose consciousness? If so, how long for?
“I definitely lost consciousness, but I’m not sure how long for, probably only 30 seconds or so”
What were you doing immediately before the loss of consciousness?
“I was walking across the sand dunes with the dogs”
“It was quite a sharp incline and I did run after the dog as he’d disappeared over the top of the dune and I was worried he’d run away”
Did anyone witness the collapse?
“Yes another dog walker came over, she called an ambulance”
Did you lose control of your bowels or bladder during the episode?
“No”
Have you sustained any injuries? Did you injure your head?
“I must have banged my shoulder because it’s hurting, I think it hit a rock”
“I don’t think I’ve injured my head”
Do you know where you are? What is today’s date? What is my job?
*Patient is orientated* – GCS 15
Have you experienced anything like this before?
“I’ve had a few faints in the past, not whilst walking the dogs though”
“I had one when I was getting out of the shower, the room was really hot and I started feeling nauseous then blacked out”
What’s your usual exercise tolerance?
“It’s decreased over the last year”
“I used to take the dogs out for at least an hour, often 2 hours”
“Now it’s more like 20 minutes maximum”
Why are you not able to stay out longer?
“Because I just don’t have the strength, I get tired much easier than I used too and often begin to feel quite short of breath”
Any nausea or vomiting?
“No”
Collateral history
A collateral history from a witness may provide valuable information about the nature of the patient’s collapse. Thankfully, the other dog walker came in the ambulance with the patient, so you can ask them some questions.
How did Mr Smith look when you arrived?
“He was very pale when I got to him”
Was he conscious when you arrived?
“Not initially, he didn’t respond for the first 30 seconds“
When he did regain consciousness, was he orientated?
“He wasn’t confused, he was orientated”
How quickly did he go from being unconscious to being orientated?
“He recovered quickly, within 20 seconds he appeared fairly normal, just a little pale”
Did you notice any jerking movements or tongue biting whilst he was unconscious?
“He wasn’t jerking, he was just lying still and I didn’t notice him biting his tongue”
Other areas of the history
Past medical history
- Pre-syncope/syncope (e.g. previous symptoms of dizziness or loss of consciousness)
- Seizures (e.g. known diagnosis of epilepsy)
- Cardiac conditions (e.g. arrhythmias, myocardial infarction, postural hypotension)
- Malignancy (e.g. loss of consciousness/seizures can be the presenting symptom of primary brain malignancy or secondary intracerebral metastases)
Medications
Regular medications:
- Be aware of medications that can cause syncope as a side effect (e.g. antihypertensives)
- Anticonvulsant medication (ensure the patient hasn’t missed any doses, which may have caused a seizure)
- Antiplatelets/anticoagulants (important when considering haemorrhage as a cause of loss of consciousness or traumatic haemorrhage secondary to the fall)
Recreational drug use:
- Many recreational drugs can cause a reduced level of consciousness, seizures and arrhythmias
Family history
- Cardiac disease (e.g. cardiac arrest/myocardial infarction in young members of the family)
- Seizures (e.g. epilepsy)
Social history
- Accommodation – the type of accommodation and details of who the patient is living with
- Alcohol history – a potential risk factor for falls and seizures
- Smoking history – a potential risk factor for malignancy and cardiovascular disease
- Occupation – loss of consciousness may have implications on the patient’s ability to work (e.g. if working at height or operating heavy machinery)
- Driving – the patient would not be able to drive until they have undergone further investigations to identify a cause for their loss of consciousness
Systemic enquiry
- Symptoms in other body systems that may be relevant (e.g. weight loss, fevers)
Answer
“I take ramipril for my blood pressure but no other regular medication. I’ve had several episodes of dizziness over the last year or so. I’ve not had any heart attacks or other medical problems and I’ve never taken any recreational drugs. There are no diseases that run in my family and I live alone in a bungalow. I used to drink a few pints of beer a week, but I stopped drinking a few years ago. I don’t smoke, I’m now retired and I don’t drive.”
Clinical examination
- Cardiovascular examination
- Respiratory examination
- Cranial nerve examination
- Upper and lower limb neurological examination
- General musculoskeletal examination
Clinical findings
Cardiovascular examination:
- Pulse – 65 bpm (slow rising in nature)
- BP – 150/120 mmHg
- CRT – <2 seconds
- Auscultation:
- Ejection systolic murmur heard loudest over the sternum
- The murmur can be heard radiating to the carotid arteries
Respiratory examination:
- Equal air entry
- No added sounds
- Sats 98%
- Respiratory rate – 16
Neurological examination:
- Cranial nerves intact
- No upper or lower limb neurological deficits
Musculoskeletal examination:
- Some bruising on the right shoulder
- Normal range of movements in all joints
- Nil else of significance
Investigations
Basic observations (vital signs): BP, pulse, respiratory rate, oxygen saturation, temperature
Blood tests:
- Capillary blood glucose
- Full blood count
- Urea & electrolytes
- CRP
- Troponin
- Coagulation
Other tests:
Bedside investigation results
Vital signs:
- BP 150/120 mmHg
- Pulse 65 bpm
- RR 16
- Oxygen saturation 98% breathing air
- Temperature – 36.3°c
Blood tests:
- Capillary blood glucose – normal
- FBC – normal
- CRP – normal
- Troponin – negative
- U&Es – normal
- Coagulation – normal
ECG
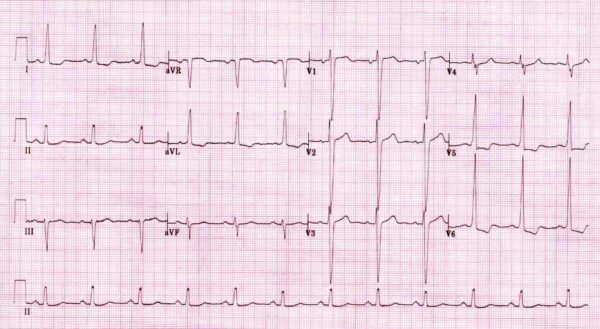
- Rate – 75bpm
- Sinus rhythm
- Normal PR interval
- Normal QRS duration
- Normal QT interval
Left ventricular hypertrophy with strain pattern:
- Increased R wave amplitude in left-sided leads (I, aVL and V5-6)
- Increased S wave depth in the right-sided leads (III, aVR, V1-3)
- ST depression in the lateral leads (I, aVL and V5-6)
For more information, see our guide to ECG interpretation.
- Clear lung fields
- Cardiomegaly
For more information, see our guide to chest X-ray interpretation.
Differential diagnoses
- Vasovagal syncope
- Aortic stenosis
- Hypertrophic cardiomyopathy
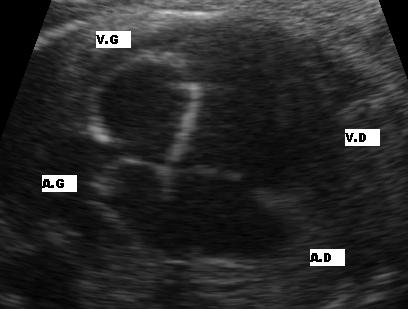
Echocardiography
- A transthoracic echo demonstrates severe aortic stenosis with associated left ventricular hypertrophy.
Management
Symptomatic patients require early surgical intervention as no medical therapy for aortic stenosis can improve overall patient outcome.
Medical therapy
Modification of atherosclerotic risk factors is strongly recommended. Aortic stenosis in older patients should be recognised as a significant risk for ischaemic heart disease: ²
- Commence statin therapy if cholesterol raised
- Commence antihypertensive medication if the patient is found to be hypertensive (being careful not to induce hypotension)
- If the patient smokes, smoking cessation advice should be given
- All patients should receive advice on how to eat a healthy balanced diet
If a patient is unsuitable for surgical intervention:
- Consider prescribing digoxin, diuretics and an ACE inhibitor to provide symptomatic relief from heart failure symptoms.
- Maintenance of sinus rhythm is important (use antiarrhythmic drugs as required)
Aortic valve replacement
Aortic valve replacement (AVR) is the definitive therapy for severe aortic stenosis (AS).
Operative mortality of AVR for AS:
- 1-3% in patients < 70 years
- 4-8% in older adults
Early valve replacement is strongly recommended for all symptomatic patients with severe AS who are suitable for surgery.
Transcatheter aortic valve implantation (TAVI)
TAVI provides a method of AVR which does not carry the same risks as surgical AVR.
TAVI can be performed under a general anaesthetic or under local anaesthetic with sedation, making it an option for patients who are unsuitable for surgical AVR.
TAVI involves the replacement of the aortic valve of the heart via the blood vessels (not requiring open-heart surgery). The replacement valve is delivered via one of several access methods: transfemoral (in the upper leg), transapical (through the wall of the heart), subclavian (beneath the collarbone) or direct aortic (through a minimally invasive surgical incision into the aorta). The whole procedure occurs under fluoroscopic and echocardiographic guidance.
Key points:
- TAVI is less invasive and carries fewer risks than a surgical aortic valve replacement.
- TAVI is of equal efficacy as surgical AVR in patients who are unsuitable for surgery.
- As with any surgical procedure, there are associated risks which include major bleeding, stroke, arrhythmias, myocardial infarction, aortic dissection and residual aortic regurgitation.
Balloon valvuloplasty
This procedure involves widening of a stenotic aortic valve using a balloon catheter inside the valve. The balloon is inflated in an effort to increase the opening size of the valve and improve blood flow. Current evidence supports the safety and efficacy of balloon valvuloplasty for aortic valve stenosis in adults and children. However, re-stenosis and clinical deterioration occur within 6-12 months in most patients.³
In adults, the procedure is only used to treat patients who are unsuitable for surgery, due to the efficacy typically being short-lived.
References
- Electrocardiographic left ventricular hypertrophy with strain pattern: prevalence, mechanisms and prognostic implications. Cardiovasc J Afr. 2008 Feb; 19(1): 39–45.
- By Nevit Dilmen (Own work). Licence: [CC BY-SA 3.0]
- Prasad Y, Bhalodkar NC; Aortic sclerosis–a marker of coronary atherosclerosis. Clin Cardiol. 2004 Dec;27(12):671-3. Available from: [LINK]
- Balloon valvuloplasty for aortic valve stenosis in adults and children. NICE Interventional Procedure Guideline (2004). Available from: [LINK].





