- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
A 57 year old man presents to the emergency department with chest pain. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
- Chest pain
History
Presenting complaint
“Doctor, my chest, it’s still hurting. What’s going on?”
History of presenting complaint
Use the SOCRATES acronym to gather further information about the chest pain:
- Site – “Where exactly is the pain?”
- Onset – “How quickly did the pain reach its maximum intensity?”
- Character – “What kind of pain are you experiencing?” (e.g. sharp, dull, crushing)
- Radiation – “Does the pain move anywhere else?”
- Associated symptoms – “Have you developed any other symptoms?” (e.g. shortness of breath, pre-syncope, syncope)
- Timing – “How long has the chest pain been present?”
- Exacerbating and relieving factors – “Does anything make the pain worse?” “Does anything reduce the pain?”
- Severity – “On a scale of 1-10, how severe would you rate your pain?” (this can be useful later when assessing the impact of treatment)
Answer
“The pain is in the middle of my chest and came on suddenly an hour ago whilst I was watching TV. It feels like I’ve got an elephant sat on my chest doctor, it’s awful! I had a bit of tingling in my neck and jaw, but that’s gone now. I feel really sick, I vomited once at home before the ambulance arrived.
I do feel a little short of breath, which is weird, I’ve never had that before, maybe I’m just anxious. The pain isn’t affected by my position or by taking in a deep breath, it’s just always there. The pain has improved but it’s still aching and feels heavy, I’d say it was 8/10 at the start and it’s now about 5/10.”
Other areas of the history
Past medical history
Has the patient had chest pain in the past?
- When was the first episode?
- How frequently do the episodes occur?
- Is there an obvious trigger? (e.g. exertion)
- Have they been investigated for chest pain?
- Do they have a diagnosis of any cardiac problems?
Any other medical problems? (specifically cardiac risk factors)
- Diabetes
- Hypertension
- Hypercholesterolaemia
- Ischaemic heart disease
- Family history of cardiac issues
Social history
- Smoking history
- Alcohol intake
- Exercise tolerance
Answer
“I’ve never had chest pain like this before, maybe a few niggles every few months over the last few years, but nothing like this! I didn’t bother going to the doctor about the niggles, as they always settled on their own and I’ve never been diagnosed as having any heart trouble.”
“I’ve got high blood pressure and cholesterol, I’m on tablets for those though.”
“I do smoke, about 20 a day and have done for the last 30 years.”
“I’m not a drinker doctor, I like to stay healthy so I stay away from it.”
“I don’t really do much exercise, but I get from the shops and back without any trouble.”
Clinical examination
Clinical findings
- The patient has a regular pulse, is tachycardic at 105 bpm and is hypertensive with a BP of 160/110 mmHg.
- He has some xanthelasma around his eyes and also has corneal arcus.
- Heart sounds are normal and his chest is clear.
- There is no evidence of peripheral oedema.
- The abdomen is soft and non-tender. There is no organomegaly. There is no expansile mass on palpation of the aorta.
Differential diagnoses
- Acute coronary syndrome
- Pulmonary embolism
- Pericarditis
- Dissecting aortic aneurysm
- Oesophageal spasm
- Looking for acute ischaemic changes
Blood tests:
- Full blood count (e.g. severe anaemia can cause a myocardial infarction)
- Urea & electrolytes (e.g. abnormal electrolytes could cause arrhythmias)
- Troponin T – baseline + 3/6 hours from presentation (>20% rise suggest acute myocardial infarction)
- Lipid profile – useful for informing long-term cardiovascular risk reduction (e.g. statin dose)
- Serum glucose:
- Identifying hyperglycaemia can help to inform long-term management of modifiable risk factors.
- It is also important to identify hyperglycaemia in the acute setting. NICE recommends keeping blood glucose <11mmol/L whilst avoiding hypoglycaemia (e.g. dose-adjusted insulin infusion).
- Assess for signs of heart failure (e.g. cardiomegaly, pulmonary oedema)
Investigation results
An ECG was recorded and is shown below.
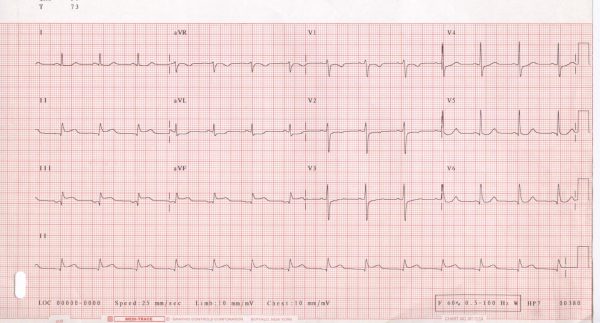
Inferior ST-elevation myocardial infarction (STEMI)
- The ECG reveals ST-segment elevation in Leads II, III and aVF, suggesting an inferior myocardial infarction.
Right coronary artery
- The right coronary artery provides the blood supply to the inferior/posterior portion of the heart.
Below is a guide to which vessels are most likely affected in each type of myocardial infarction:
- Anterior – Left coronary artery
- Posterior – Left circumflex artery (usually) and/or right coronary artery
- Inferior – Right coronary artery
- Lateral – Left circumflex artery
- Antero-septal – Left anterior descending artery (LAD)
For more information, see our guide to understanding an ECG.
Management
ABCDE approach
Initially, an ABCDE approach should be adopted to ensure any immediate threats to life are recognised and treated. This would include administering oxygen if appropriate (SpO2 <94%), gaining intravenous access, and administering medications such as morphine, glyceryl trinitrate and antiemetics.
Antiplatelet therapy
In the presence of ischaemic ECG changes or elevation of cardiac troponin, patients presenting with acute coronary syndrome (ACS) should be treated immediately with:
- Aspirin (300mg loading dose)
- A second rapid-acting antiplatelet such as ticagrelor or prasugrel
Coronary reperfusion therapy
Patients should immediately have their eligibility for coronary reperfusion therapy assessed (PCI vs fibrinolysis):
Offer coronary angiography, with follow-on primary PCI if indicated, as the preferred coronary reperfusion strategy for people with acute STEMI if:
- presentation is within 12 hours of the onset of symptoms and
- primary PCI can be delivered within 120 minutes of the time when fibrinolysis could have been given
Offer fibrinolysis to people with acute STEMI presenting within 12 hours of the onset of symptoms if primary PCI cannot be delivered within 120 minutes of the time when fibrinolysis could have been given.
Drugs
- Dual antiplatelet therapy (aspirin plus a second antiplatelet) is often continued for 12 months after PCI
- A single antiplatelet agent is then usually continued long-term
ACE-inhibitor (e.g. ramipril)
- Started at a low dose, then titrated upwards. Continued indefinitely.
- An ARB can be used if intolerant of an ACE inhibitor
Beta blocker
- For at least 12 months, beta-blockers should be continued indefinitely in patients with a reduced left ventricular ejection fraction (LVEF)
Statin
- All patients should be on a statin for secondary prevention
Address other cardiac risk factors
- Hyperglycaemia – check HBA1c and manage if required
- Smoking cessation
- Healthy diet
- Physical activity
- Weight loss (if appropriate)
Cardiac rehabilitation
- A structured program for improving cardiovascular health
References
- Glenlarson. Example ECG. License: [CC BY-SA].
- NICE. Acute coronary syndromes (including myocardial infarction); NICE Quality Standard. 2020. Available from: [LINK].
- NICE. Acute coronary syndrome. 2020. Available from:




