- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This article provides a step-by-step approach to counselling patients about systemic corticosteroids in an OSCE setting.
Opening the consultation
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Clarify the purpose of the consultation: “I’ve come to discuss a type of medication known as steroids, would that be okay?”
It is important to establish a good rapport and an open line of communication with the patient early in the consultation: “If you have any questions at any point – or if something is not clear – please feel free to interrupt and ask me.”
Make sure to check the patient’s understanding at regular intervals throughout the consultation and provide opportunities to ask questions (this is often referred to as ‘chunking and checking’).
Patient’s ideas, concerns and expectations
A key component of counselling involves exploring a patient’s ideas, concerns and expectations (often referred to as ICE).
Asking about a patient’s ideas, concerns and expectations can allow you to gain insight into how a patient currently perceives their situation, what they are worried about and what they expect from the consultation. It can sometimes be challenging to use the ICE structure in a way that sounds natural in your consultation, but we have provided some examples for each of the three areas below.
Ideas
- “Have you heard of steroids?”
- “What do you know about steroids?”
- “Do you know what steroids are used for?”
Concerns
- “Is there anything, in particular, that’s worrying you about taking steroids?”
Expectations
- “What were you hoping to get from our discussion today?”
- “Is there anything, in particular, you would like me to discuss or focus on today?”
Tip: Establishing the patient’s ideas, concerns and expectations early in the consultation will enable you to focus on the factors that matter most to the patient. This will increase the quality of the consultation and further build rapport between you and the patient.
Patient history
Although the purpose of this station is to counsel the patient, it is a good idea to gather a quick, focused history early in the consultation.
This should include an exploration of the patient’s symptoms and management of their condition, including trials of previous medications, their impact, compliance and adverse effects. Before prescribing any drug, ask about allergies, contraindications and cautions, other medications the patient is taking, smoking and pregnancy.
Systemic corticosteroids treat a wide range of conditions and come in various formulations with different treatment plans. Identifying the condition and the indication for starting corticosteroids in each patient is important.
Conditions treated with systemic corticosteroids
Rheumatological conditions:
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Polymyalgia rheumatica
- Temporal (giant cell) arteritis
- Sarcoidosis
Gastrointestinal:
- Crohn’s disease
- Ulcerative colitis
Respiratory
Other
- Organ transplants
Understanding the patient’s care so far will help you tailor any advice and personalise the information for their situation.
Allergies
Ask the patient if they have any known allergies. If the patient has had a drug reaction previously, ask about the features and severity of the reaction.
An individual’s drug allergy status should be documented in their medical records, and this information should be kept distinct from the details of any adverse drug reactions.1
- “Are you allergic to any medications?”
- “Have you reacted to any medications in the past?”
Contraindications and cautions for steroids
Before prescribing corticosteroids, it is important to screen for any contraindications. Patients with acute systemic infections should not receive corticosteroids, as they can weaken the immune system.2
There are several cautions to consider when prescribing systemic corticosteroids. These include:3,4
- Hepatic impairment
- Unhealed wounds
- Stomach ulcers
- Pre-existing conditions such as heart failure, hypertension, diabetes mellitus or epilepsy
- History of mental health problems: corticosteroids can exacerbate emotional instability or psychotic tendencies
“Do you know of any reasons why you may not be able to take steroids?”
“Before starting corticosteroid treatment, we must know if you have any medical conditions. This includes conditions like diabetes, epilepsy, high blood pressure, or problems with your liver, heart, kidneys or stomach ulcers. Do you have any of these conditions?”
Pregnancy and breastfeeding
If appropriate, ask the patient if there is any chance they are pregnant or are currently breastfeeding. Corticosteroids may be prescribed during pregnancy if the benefits outweigh the risks. This is decided on a patient-by-patient basis, considering the mother’s medical needs and potential risk to the foetus.
However, prolonged or repeated courses of steroids during pregnancies may have adverse effects on fetal growth.
In breastfeeding women, prednisolone is usually recommended as it has a lower transfer rate to breast milk and is considered safe for the infant. Infants should be monitored for signs of adrenal insufficiency if the mother takes doses above 40mg.2,5
“Is there any chance you are pregnant, or are you currently breastfeeding?”
Drug history2
An accurate drug history is essential to identify potential drug interactions.
Patients should avoid taking steroids with NSAIDs (e.g. ibuprofen) as this increases the risk of stomach or duodenal ulceration and bleeding. However, if a patient needs to take both medications, a proton pump inhibitor (PPI) can be prescribed to reduce this risk.
For patients on immunosuppressive doses of corticosteroids, live vaccines (e.g. polio, MMR and BCG) should be avoided. These vaccines should be postponed for at least 3 months after the patient stops taking high-dose steroids, as they may develop a life-threatening infection.6
Other medications which may interact with systemic corticosteroids include:2
- Anticoagulants
- Anticonvulsants
- Diabetes medication
- HIV medication and protease inhibitors
Corticosteroids can increase the chance of hypokalemia when prescribed with other potassium-lowering medications. Medications which reduce potassium levels include diuretics, laxatives, bronchodilators, insulin and digoxin.8
“Are you currently taking any regular medications or over-the-counter medicines?”
What are corticosteroids?
Corticosteroids, or steroids, are medications used to reduce inflammation and suppress the immune system in various conditions.5
Corticosteroids are produced naturally in the cortex of the adrenal gland, regulated by the hypothalamic-pituitary-adrenal (HPA) axis. They are involved in many physiological processes, including stress and immune response, inflammation, and electrolyte levels.
Systemic corticosteroids are administered orally or by injection and affect multiple systems in the body. Localised corticosteroids are applied topically, as drops, inhaled, or through intra-articular injection, targeting a specific area.
Common systemic corticosteroids include dexamethasone, hydrocortisone, fludrocortisone, and prednisolone.
Systemic corticosteroids can be used in the treatment of autoimmune disease (e.g. inflammatory bowel disease, inflammatory arthritis, autoimmune hepatitis or systemic lupus erythematosus), allergic inflammatory disorders (e.g. anaphylaxis, asthma or eczema), corticosteroid replacement therapy (e.g. adrenal insufficiency or hypopituitarism) and in some cancer treatments.6,8
Make it clear to the patient that corticosteroids differ from anabolic steroids used illegally by some people to build muscle mass.3
“Corticosteroids, commonly just called steroids, are medications used to reduce inflammation or ‘dampen down’ your immune system. They are commonly used to treat a range of conditions such as asthma, rheumatoid arthritis, and skin conditions like eczema.”
How do systemic corticosteroids work?8,9,10
There are two classifications of corticosteroids:
- Glucocorticoids: potent inhibitors of inflammation
- Mineralocorticoids: influence water and electrolyte balance
Corticosteroids have several different modes of action. They are glucocorticoid receptor (GR) agonists altering the gene expression of cells. This reduces the inflammatory response by down-regulating pro-inflammatory and up-regulating anti-inflammatory mediators. They have an immunosuppressive effect by reducing circulating immune cells.
They can also have mineralocorticoid activity, stimulating sodium resorption and water retention with selective potassium excretion by the kidneys.
Synthetic corticosteroid drugs have different glucocorticoid and mineralocorticoid actions, which is important in clinical use. For example, dexamethasone has almost purely glucocorticoid effects and is used to reduce inflammation (e.g. croup). In contrast, fludrocortisone has mineralocorticoid effects and causes sodium and water retention. Therefore, it is used to treat postural hypotension.
“Corticosteroids work by reducing inflammation or suppressing your immune system. They do this by changing how some cells behave. This reduces swelling, redness and pain from inflammation.”
How to take steroids
Systemic steroids are available in various forms, including tablets, liquids, powders, and injectables, but they are most commonly prescribed as a tablet.
Steroids should be taken at the same time(s) each day, usually in the morning. This is because steroids can cause insomnia, and taking them in the morning mimics the body’s normal circadian rhythm.2,5
Oral steroids should be taken with or soon after a meal, typically breakfast, as they can irritate the stomach. Patients should take all their prescribed tablets in a single administration. Sometimes, this is a significant number of tablets. For example, if a patient is prescribed a daily dose of 40mg of prednisone, they would need to take eight 5mg tablets.7
Duration of treatment
The duration of treatment varies depending on the condition. Some patients may require long-term corticosteroids (months to years).
The doses of steroid can be adjusted based on the patient’s response to the therapy and the severity of the condition.
Patient factors (e.g. age, medical history, weight, and overall health) are considered when determining the appropriate dose and duration of treatment. The goal is to use the lowest effective dose for the shortest time to control the patient’s symptoms and minimise side effects.7, 10
“The duration of steroid treatment and the dose prescribed will depend on how well your body responds to the treatment, as well as the nature and severity of the condition being treated. Although steroids are very effective, we try to use them for the shortest possible time and at the lowest dose. This reduces the risk of any side effects.”
Missed doses
Patients who forget a dose should take it as soon as they remember. However, if it is the next day or time for their next dose, they should not take two doses to compensate for the forgotten dose.3
“If you forget to take your steroid at the prescribed time, take it as soon as you remember. However, if it’s almost time for your next dose, skip the missed dose and resume your regular dosing schedule. Do not take an extra dose to make up for a missed dose.”
Steroid monitoring
Before patients start long-term systemic corticosteroid treatment, baseline tests should be performed:2,10
- Blood pressure, body weight, and BMI measurements
- Eye examination to assess for cataracts or glaucoma
- Blood tests: HbA1c, triglycerides, and potassium levels
Patients should be screened for adverse effects at follow-up:2
- Regular blood pressure and body weight checks
- An eye examination every 6-12 months to monitor for cataracts and glaucoma
- Triglycerides and potassium levels one month after initiation and then every 6-12 months
- HbA1c 1 month after initiation after treatment, then every 3 months
“Before starting steroids, you will need some baseline tests like your blood pressure, weight and an eye examination. You will also need a blood test to check your blood sugar and electrolyte levels.”
“When you are taking steroids, we will review you regularly. It is important to monitor your blood pressure, blood sugar and weight.”
What are the side effects of steroids?
Like all medications, there are side effects associated with steroids. Some side effects are more severe than others. Educating patients about the signs associated with serious side effects is essential.
Patients are more likely to experience side effects if they are on higher doses, taking steroids for longer than 3 weeks or have repeated short courses.
Common short-term side effects include:3,7,10,11
- Sleep disturbance and insomnia
- Weight gain: this can be due to increased appetite and water retention
- Mood changes
Long-term side effects
Prolonged use of corticosteroids can have serious long-term side effects, including:3,7,10,11
- Cushing’s syndrome
- Osteoporosis: increased risk of fractures
- Proximal muscle weakness
- Hypertension
- Hyperglycaemia and diabetes
- Increased risk of infection
- Adrenal insufficiency (see below)
- Peptic ulceration
- Cataracts
- Mental health problems: depression, psychosis, delirium or suicidal thoughts
Cushing’s syndrome
Cushing’s syndrome occurs because of prolonged exposure to excess glucocorticoids.
Typical clinical features of Cushing’s syndrome include:
- Truncal obesity
- Buffalo hump
- Supraclavicular fat pads
- Moon facies
- Proximal muscle wasting
- Bruising
- Peripheral oedema
- Acne
For more information, see the Geeky Medics guide to performing a Cushing’s syndrome examination.
“Steroids can have both short-term and long-term side effects. Some common short-term side effects include trouble sleeping, increased appetite causing weight gain, indigestion, and mood changes making you feel irritable or short-tempered.”
“If you take steroids for a long time, you may be at risk of more serious side effects like muscle and bone weakness, stomach ulcers, mental health problems, and increased risk of infections.”
“Corticosteroids can also increase your risk of developing diabetes, hypertension, and cataracts. If you have any concerns or notice new symptoms while taking steroids, it’s important to seek advice. We will be reviewing you regularly whilst you are on treatment, and we will monitor for any side effects,”
“Most short-term side effects resolve after steroid treatment is stopped.”
Steroid withdrawal & adrenal insufficiency2,3,7
When patients take steroids for more than 3 weeks, it can cause adrenal insufficiency or suppression. Sudden withdrawal of steroids can precipitate an adrenal crisis, which can be life-threatening.
Patients should be informed of the signs of adrenal insufficiency:
- Feeling extremely tired and weak
- Nausea and vomiting
- Abdominal pain
- Diarrhoea
- Dizziness
- Loss of appetite and weight loss
If patients are to stop steroids, the dose should be reduced gradually, as this allows the body to resume the natural production of steroids.
“It’s important to talk to your doctor before stopping steroids. Never stop them suddenly. If you have been taking steroids for a long time, stopping them abruptly can cause a life-threatening condition called an adrenal crisis. This occurs because your body’s natural production of steroids has been switched off.”
“An adrenal crisis can cause symptoms such as tummy pain, feeling sick, dizziness, fever, headache, weight loss or feeling extremely tired and weak. If you experience any of these symptoms, especially if they occur suddenly or severely, seek urgent medical help.”
“When stopping steroids, your doctor will very gradually reduce your dose, allowing your body to start making its own steroids again.”
Steroid emergency card12,13,14
Patients with adrenal insufficiency and steroid dependency at risk of adrenal crisis should always carry a steroid emergency card or medical alert bracelet. This should include patient details, information about the steroid medication and dosage, and emergency contact information.
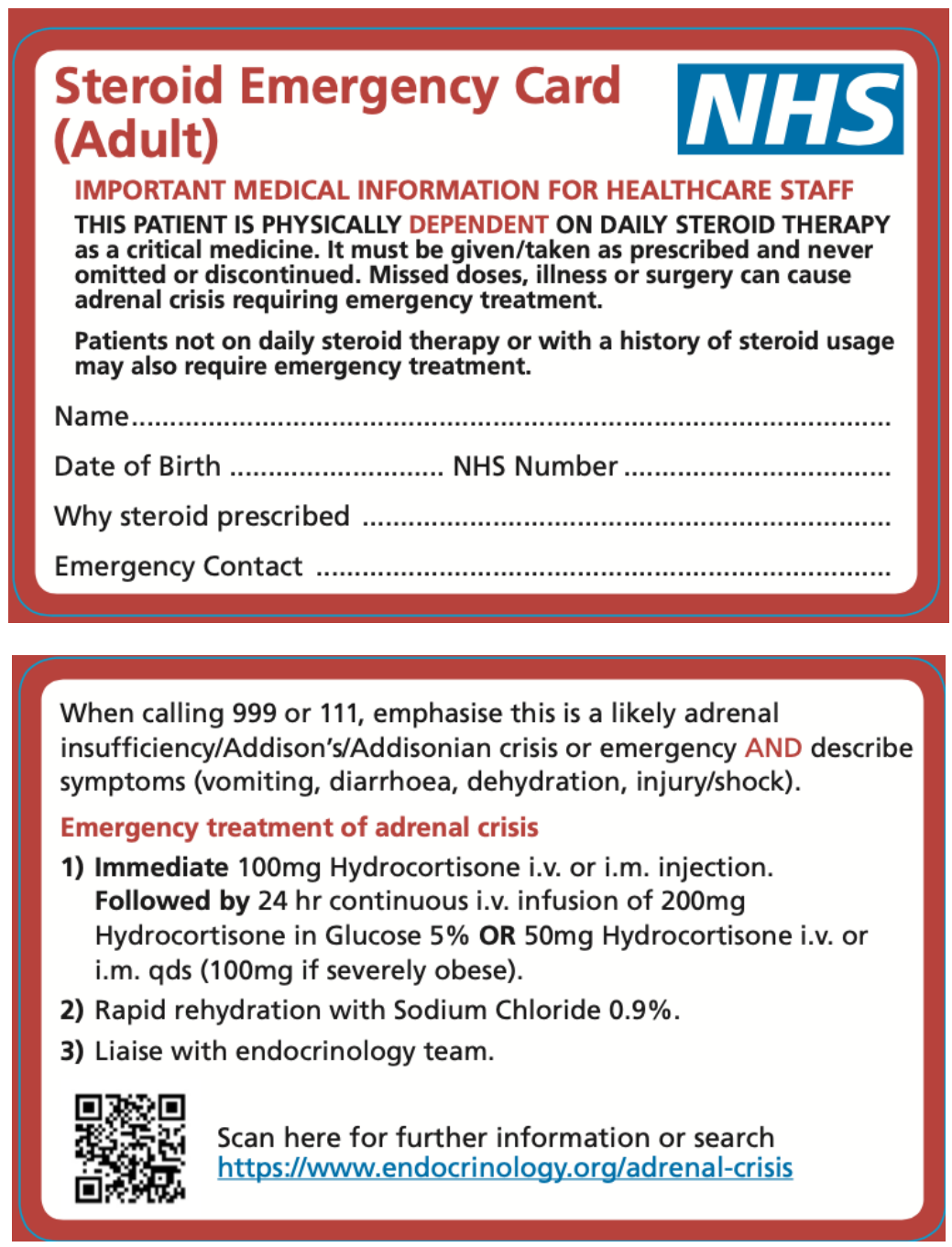
Steroid emergency cards should be issued to patients taking the following doses of cortiosteroids:15
- Prednisolone 5mg per day (or an equivalent steroid) for four weeks or longer (all routes of administration – oral, topical, inhaled or intranasal)
- Inhaled beclomethasone >1000 mcg per day or fluticasone >500mcg/day or higher
Patients should be educated on the importance of carrying the card, as this ensures steroids are never omitted or discontinued, as missed doses or illness can trigger an adrenal crisis.
“A steroid emergency card is a small card you should always carry if you take regular steroids. This card is important if you become acutely unwell, the healthcare team need to know that you take steroids as stopping or missing a dose could be life-threatening. Always keep it with you at all times and show it to any healthcare professional you see.”
Steroid sick day rules2,12,16
Patients with adrenal suppression cannot produce enough natural steroids to cope with acute stress (e.g. illness, trauma or surgery). Therefore, they must increase their steroid dose to prevent an adrenal crisis. These are called ‘sick day rules’.
Usually, the daily dose is doubled during an acute illness. The increased dose should be continued until the patient recovers, and then the dose is reduced back to the usual maintenance dose.
“When you get sick, your body naturally produces more steroids to help you cope with the stress of the illness. However, if you have been taking steroids for a long time, your body’s natural production of steroids may have been switched off, which can lead to a life-threatening adrenal crisis.”
“To avoid this, it is important to follow sick day rules. If you become suddenly unwell, we may need to increase your steroid dose. Please contact us if you become unwell whilst taking steroids.”.
Closing the consultation
Close the consultation by summarising what you have discussed. This allows you to emphasise the key points of the consultation.
Ask the patient if they have any questions or concerns that have not been addressed.
Finally, thank the patient for their time and offer them a leaflet summarising the key information related to corticosteroids.
Dispose of PPE appropriately and wash your hands.
Reviewer
Holly Elwell
Highly Specialist Pharmacist for Medical Education
Honorary Lecturer in Pharmacology and Prescribing Practice
Editor
Dr Chris Jefferies
References
- Medscape UK. Drug allergy: diagnosis and management. 2014. Available from: [LINK]
- NICE CKS. Scenario: Corticosteroids. 2020. Available from: [LINK]
- NHS. Steroid tablets. 2020. Available from: [LINK]
- NHS. Steroid injections. 2023. Available from: [LINK]
- NHS inform. About Corticosteroids. 2023. Available from: [LINK]
- NHS inform. Cautions, side effects and interactions. 2023. Available from: [LINK]
- Patient.info. Oral Steroids. 2021. Available from: [LINK]
- Nurse Study. Corticosteroids Nursing Considerations. 2023. Available from: [LINK]
- Ramamoorthy S. Cidlowski J. Corticosteroids-Mechanisms of Action in Health and Disease. 2017. Available from: [LINK]
- DermNet. Systemic Corticosteroid. 2016. Available from: [LINK]
- Macmillan. Steroids. 2022. Available from: [LINK]
- Macmillan. Adrenal insufficiency. 2020. Available from: [LINK]
- National Patient Safety Alert. Steroid Emergency Card to Support Early Recognition and treatment of Adrenal crisis in adults. 2020. Available from: [LINK]
- Society for Endocrinology. Steroid Card. 2020. Available from: [LINK]
- Royal College of Physicians. Guidance for the prevention and emergency management of adult patients with adrenal insufficiency. 2020. Available from: [LINK]
- Society for Endocrinology. Steroid Sick Day Rules. 2021. Available from: [LINK]




