- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Obesity is a metabolic disease defined as an excessive accumulation of body fat that poses a risk to an individual’s health. It is caused by prolonged imbalance where energy intake exceeds energy expenditure.1,3
According to World Health Organisation (WHO), obesity is a global epidemic, with 4 million people dying annually due to the disease. In the UK, 1 in 4 adults and 1 in 5 children are obese.2
Body mass index (BMI) is the most widely accepted measurement of obesity, with individuals with a BMI of more than 25 classed as overweight or obese.3 Alternative measurement tools include waist circumference and waist-to-height circumference.
Aetiology
The cause of obesity is complex and multifactorial. The main factors contributing to obesity are behavioural/lifestyle-related, age, medications, hormonal issues, and genetics.3,5
In simple terms, obesity is caused by an energy imbalance between calorie intake and expenditure over a prolonged period.4
Risk factors
The main risk factors for obesity include poor diet and lack of physical activity.
Other risk factors include:3,6
- Underlying medical conditions: Cushing’s syndrome, polycystic ovarian syndrome (PCOS), hypothyroidism and growth hormone deficiency
- Medications: antidepressants (tricyclics, monoamine oxidase inhibitors, mirtazapine, atypical antipsychotics) and corticosteroids
- Socio-economic status: access to healthy food, education about healthy diet
- Mental health: depression, eating disorders (e.g. binge eating disorder, emotional eating)
- Genetics: rare genetic conditions, such as Prader-Willi syndrome and Bardet-Biedl syndrome, can result in obesity
Although genetics has been shown to play a role in regulating body weight, behavioural and environmental factors are deemed the main contributors to obesity.5
Metabolic syndrome
Metabolic syndrome is a term used to describe a group of risk factors including hypertension, hyperglycaemia, excess fat around the waist, and hypercholesterolemia. It increases the likelihood of developing diabetes, stroke, and heart disease.7
Clinical features
A thorough history and examination are crucial to assess the cause of obesity and investigate for associated co-morbidities.
The main feature of obesity is excess body fat and weight above average for an individual’s height.
Other clinical features are non-specific, including:
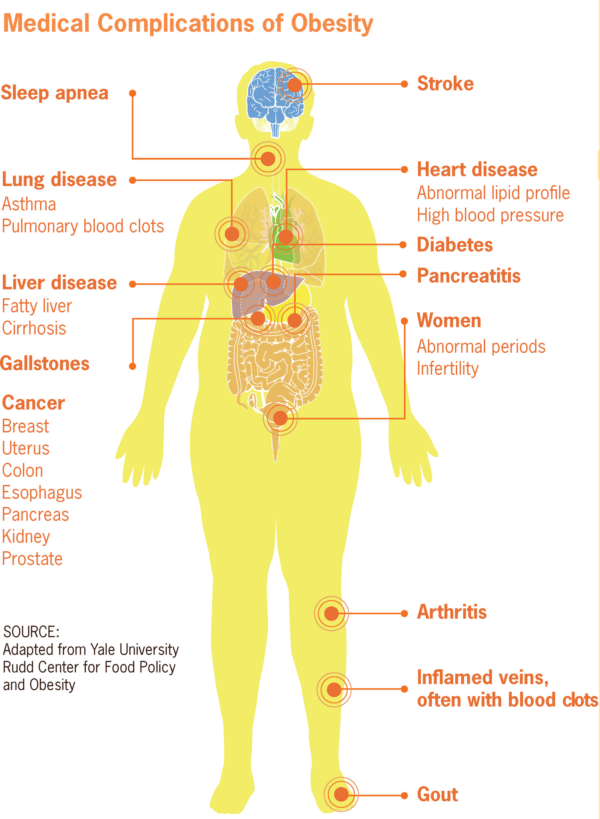
- Breathlessness
- Sleep apnoea
- Skin problems (e.g. intertrigo), increased risk of skin infections
- Osteoarthritis
- Hypertension, diabetes, and hyperlipidaemia.8
History
Important areas to cover in the history include:9,10
- Body weight history: current weight, recent changes to weight and previous weight loss attempts
- Dietary history: current meals, frequency, quantity of meals
- Physical activity history: previous physical activity, current physical activity, actual and perceived barriers to increasing physical activities
- General medical history: medical conditions (e.g. hypertension/diabetes, eating disorder screen, mental health, sleep pattern)
- Medication history
- Family history: obesity, cardiovascular disease, PCOS
- Social history: alcohol, smoking history, recreational drug use
- Socio-economic and cultural history: occupation, living situation, history of trauma.9,10
Discussing weight in the consultation
Individuals who are overweight may be sensitive about discussing weight. Patients do not want clinicians to assume all their problems are weight related. It is important to listen to and address the patient’s concerns especially if their presenting complaint is not weight related.
Despite the topic’s sensitivity, as clinicians, it is important to address the subject of obesity as it can have serious health implications.
Start the conservation about weight in a non-judgemental and respectful manner. Questions which can be helpful include:
- “Could I check your weight and height today before you leave”
- “You mentioned knee pain, this may be related to excess weight. Would you like to talk about this to see if we can help you feel better?”
Clinical examination
Clinical examination should include:
- Measurement of BMI: calculated by dividing an individual’s weight (kg) by height squared
- Central obesity: measured using a waist-to-height ratio or waist circumference
BMI is a rapid and inexpensive method that uses body weight and height to determine if an individual is healthy. An individual who falls within the overweight or obese category is at an increased risk of health conditions such as heart disease or diabetes.
Despite its usefulness, BMI as a single health unit is flawed. This is because BMI does not account for body composition and cannot differentiate between body fat and muscle mass.25 For example, a bodybuilder with high muscle mass and low body fat can be classed as obese or overweight based on their BMI alone.6
An alternative preferred measurement of obesity is waist circumference or waist-to-height circumference. This measures a person’s central obesity or abdominal fat, which is a better determinant of future health risks than BMI. A waist circumference above 94cm in males and 80 cm in females is deemed high risk.21,25
When used in isolation, BMI and waist-to-height circumference are not perfect health measurements. However, within the clinical setting, they are practical and useful in identifying patients who are obese. 23,24
Calculating BMI
BMI is calculated by dividing a person’s weight (kg) by the square of their height (m). Individuals who fall into the BMI category of 25 to 29.9 and above are classed as overweight and obese:9
- Healthy weight: BMI of 18.5-24.9 kg/m2
- Overweight: BMI of 25-29.9 kg/m2
- Obesity class I: BMI of 30-34.9 kg/m2
- Obesity class II: BMI of 35-39.9 kg/m2
- Obesity class III: BMI of 40 kg/m2 or greater
5 A’s counselling approach
The 5 A’s counselling approach is a useful mnemonic for counselling patients about weight in a general primary care environment:9,13
Assess: identify patient at risk
Ask: “Before you leave could I check your weight today?”
Advise: “One of the best ways to lose weight is with support and {insert name of weight management service} is available today. I can refer you now if you are willing to give it a go?”
Assist in establishing interventions and securing goal attainment:
- The patient receives advice positively: inform the patient of the next steps
- Receptive but non-committal about a referral: show acceptance of the patient’s wishes and acknowledge their concerns
- If the patient does not want to engage accept their decision and re-offer support if they change their mind.
Actions: Make the referral, document the conversation, follow up with the patient
Investigations
Individuals with obesity are at risk of developing other health conditions such as hypertension, heart disease, and diabetes.
Laboratory investigations
Relevant laboratory investigations may include:9
- Fasting blood glucose: diabetes
- Lipid profile: hyperlipidaemia
- Liver function tests (LFTs): non-alcoholic fatty liver disease
- Thyroid-stimulating hormone (TSH): hypothyroidism
- Urea and electrolytes (U&Es): chronic kidney disease
Specific tests such as dexamethasone suppression test for Cushing’s syndrome, TSH for hypothyroidism, and ultrasound for polycystic ovarian syndrome can be requested if an underlying disease process is suspected.9,11
Management
Obesity is managed by weight loss, with a target of a 5-10% reduction in body weight.9 Management of obesity can be categorised into non-surgical and surgical.
Non-surgical
Initial management of obesity includes lifestyle changes such as encouraging regular exercise, healthy eating, alcohol recommendations and smoking cessation and therapy focused on behavioural changes.9
Alternatively, drug treatment can be offered to individuals who cannot lose weight through dietary changes and have a BMI of 30kg/m2 or 27kg/m2 with co-morbidities.8.9
In the UK, orlistat and liraglutide are the only medications approved by National Institute for Health and Care Excellence (NICE) to aid weight loss. They are recommended alongside a reduced calorie diet and increased exercise activity.5,9
Orlistat is taken orally and works by preventing the absorption of dietary fat.15 Side effects include flatus with oily spotting and loose stools.16
Liraglutide is a glucagon-like peptide-1 (GLP-1) analogue and a diabetic drug used to treat weight loss. It works by delaying gastric emptying and inducing early satiety resulting in an overall reduction in calorie intake and weight loss. Side effects include nausea, vomiting, diarrhoea, and in rare cases, pancreatitis (<1%) and thyroid (papillary) cancer.5,17
In a clinical trial, participants on liraglutide lost an average of 12% or more of their body weight compared to the placebo group.18
Surgical
Bariatric surgery is weight loss surgery used to treat individuals who are severely obese and have a BMI of ≥40 kg/m2 or a BMI between 35-40 kg/m2 with co-morbidities such as type 2 diabetes or hypertension.9,19
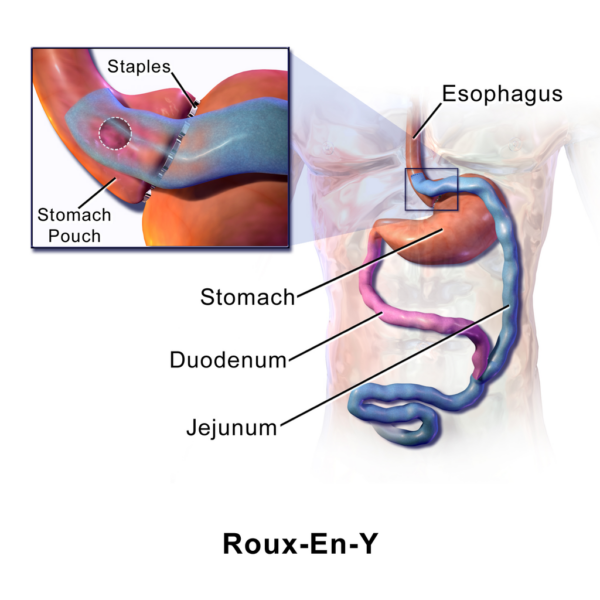
The most common types of bariatric surgery include the Roux-en-Y gastric bypass, sleeve gastrectomy, and gastric bypass.20
Weight loss surgery results in significant weight loss. Long-term maintenance of weight loss requires a commitment to healthy lifestyle changes.6
Pre- and post-operative care involves input from a multi-disciplinary team of surgeons, dieticians, and a psychologist. The role of the team is to ensure a patient is suitable for surgery and supported throughout their weight loss journey.
Preoperative requirements include blood tests to identify nutritional deficiencies and a diet to shrink the liver before surgery.
Long-term follow-up is required to monitor nutritional deficiencies and co-morbidities and provide dietary and physical activity advice. 3,26
Like any surgical procedure, there are risks such as anaesthetic risks, wound infection, and pulmonary embolism. The risks specific to bariatric surgery include acid reflux, nausea and vomiting, malnutrition, and a condition known as dumping syndrome.
Dumping syndrome
Dumping syndrome describes a group of symptoms caused by food rapidly emptying or being ‘dumped’ from the stomach into the small intestines. This results in undigested food within the small intestine that the body finds difficult to absorb. Symptoms include sweating, bloating, abdominal cramps/pain, diarrhoea, and nausea.27
Complications
Obesity is associated with increased mortality and morbidity.
Obesity-related complications include cardiovascular disease (e.g. hypertension, coronary heart disease), dyslipidaemia, diabetes, stroke, obstructive sleep apnoea, and cancer.8
Key points
- Obesity is a metabolic disease defined as an excessive accumulation of body fat
- Obesity is caused by an energy imbalance between calories intake and expenditure over a prolonged period
- Obesity can be attributed to a poor diet and lack of physical activity
- The tools to measure obesity include body mass index (BMI), waist circumference or waist-to-height ratio
- Obesity is linked with co-morbidities such as hypertension, type 2 diabetes, and cardiovascular disease
- The first line management of obesity is lifestyle changes followed by medication and bariatric surgery
Reviewer
General Practitioner
Editor
Dr Chris Jefferies
References
- Perreault, Leigh and Bessesen, Daniel. Obesity in adults: Etiologies and risk factors. Published in 2022. Available from: [LINK]
- World Health Organisation (WHO). Obesity. World Health Organisation. Published in 2022. Available from: [LINK]
- National Health Service. Obesity. Published in 2019. Available from: [LINK]
- Yoo, Sunmi. Dynamic energy balance and obesity prevention. National Library of Medicine. PubMed Central. Published in 2018. Available from: [LINK]
- Lin, Xihua and Li, Hong. Obesity: Epidemiology, Pathophysiology and Therapeutics. National Library of Medicine. PubMedCentral (PMC). Published in 2021. Available from: [LINK]
- National Health Service, NHS. Metabolic syndrome. NHS. Published in 2019. Available from: [LINK]
- Burridge, Karlijn, et al. Obesity history, physical exam, laboratory, body composition, and energy expenditure: An Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022. ScienceDirect.Published in 2022. Available from: [LINK]
- National Insititute of Diabetes and Digestive and Kidney. NIH. Published in 2017. Available from: [LINK]
- National Institute for Health and Care Excellence (NICE). Obesity: management. Published in 2022. Available from: [LINK]
- National Heart, Lung, and Blood Institute (NIH). NIH. Published in 2022. Available from: [LINK]
- Kinlen, D, Cody, D and O’Shea, D. Complications of obesity. 7, s.l. : QJM: An International Journal of Medicine, Vol. 111; Issue 7. Published in 2018.
- Public Health England. Adult weight management: a guide to brief interventions. Published in 2017. Available from: [LINK]
- Burke, Darla. Healthline: Metabolic Syndrome. Published in 2022. Available from: [LINK]
- Centers for Disease Control and Prevention (CDC). Medical Complications of Obesity. Wikimedia Commons. Published in 2012. License: [Public domain]
- British National Formulary (BNF). Orlistat. Published in 2022. Available from: [LINK]
- Drugs.com. Orlistat. Published in 2022. Available from: [LINK]
- Drugs.com. Liraglutide. Published in 2022. Available from: [LINK]
- National Institute for Health and Care Excellence (NICE). Nice recommends new drug for people living with obesity. Published in 2022. Available from: [LINK]
- Wolfe BM, Kvach E, Eckel RH. Treatment of Obesity: Weight Loss and Bariatric Surgery. Circ Res. 2016 May 27;118(11):1844-55.
- Small P, Mahawar K, Walton P, Kinsman, R. The United Kingdom National Bariatric Surgery Registry: Third Registry Report (2020). Published in 2020. Available from: [LINK]
- British Heart Foundation (BHF). Why your waist matters. Published in 2022. Available from: [LINK]
- Diabetes My Way. Baseline Measurements. Published in 2022. Available from: [LINK]
- British Heart Foundation. What’s the best way to measure body fat? Published in 2022. Available from: [LINK]
- Shmerling R. How useful is the body mass index (BMI)? Published in 2020. Available from: [LINK]
- Basile LM. The problem with BMI. Published in 2021. Available from: [LINK]
- National Institute for Health and Care Excellence (NICE). Obesity: clinical assessment and management. Quality standard [QS127] Published in 2016. Available from: [LINK]
- National Insititute of Diabetes and Digestive and Kidney. Dumping Syndrome. Published in 2019. Available from: [LINK]




