- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Superior vena cava obstruction (SVCO) can occur due to external pressure, malignant infiltration, or thrombus formation within the vessel.
This obstruction causes reduced venous return to the heart from the head, thorax and upper limbs. It is essential to recognise SVCO as it can cause life-threatening upper airway obstruction.
The most common cause is external pressure from lung cancer, affecting 2-4% of lung cancer patients. This article will focus on SVCO associated with malignancy.1
Aetiology
The superior vena cava (SVC) is found within the middle mediastinum and is surrounded by several important structures, such as the trachea, right bronchus, aorta and pulmonary artery. The SVC drains blood from the head, neck and upper extremities into the right atrium.
The SVC has thin walls, making it prone to obstruction. If the obstruction occurs gradually, collateral circulation is recruited via the azygous, internal mammary, and long thoracic venous systems. This collateral circulation is responsible for some of the symptoms of SVCO (e.g. oedema of the upper body and dilated neck veins).
If the obstruction occurs suddenly, there is no time for collateral circulation to establish, and the presentation can often be life-threatening.
Most cases are due to malignancy, with lung cancer being the most common cancer associated with SVCO.
Risk factors
Risk factors for SVCO include:2
- Lung cancer: particularly small-cell lung cancer
- Lymphoma
- Metastatic disease: particularly breast cancer, colon cancer and oesophageal cancer
- Smoking: due to the increased risk of lung cancer, rather than a direct association
- Central venous catheter use: may be used in cancer patients for the administration of medication
- Radiation to the mediastinum
Clinical features
History
The symptoms of SVCO patients are typically associated with increased venous pressure in the upper body. Typical symptoms may include:
- Breathlessness
- Visual disturbance
- Dizziness
- Headache (worse on stooping)
- Cough
- Swelling of the face, neck and arms
The duration of symptoms can vary depending on how rapidly obstruction of the superior vena cava occurs.
Clinical examination
Typical clinical findings in SVCO may include:
- Localised oedema of the face, neck and upper limbs
- Facial plethora
- Distended neck and chest veins (non-pulsatile)
- Lymphadenopathy (particularly if lymphoma is the cause)
- Hoarse voice: may be due to laryngeal oedema or the underlying malignancy
- Stridor: due to laryngeal oedema or compression
- Cyanosis
- Papilloedema
Pemberton’s sign
The Pemberton manoeuvre may worsen these signs and symptoms. The patient should lift both arms until they touch the side of the face. A positive Pemberton’s sign is the presence of facial congestion, cyanosis and respiratory distress after ~1 minute.
Investigations
In SVCO associated with malignancy, the investigations should focus on diagnosing the condition and identifying the underlying malignancy if not already known.
Imaging
Relevant imaging investigations include:
- Chest X-ray: may show a widening of the superior mediastinum and right hilar prominence to indicate a mediastinal mass
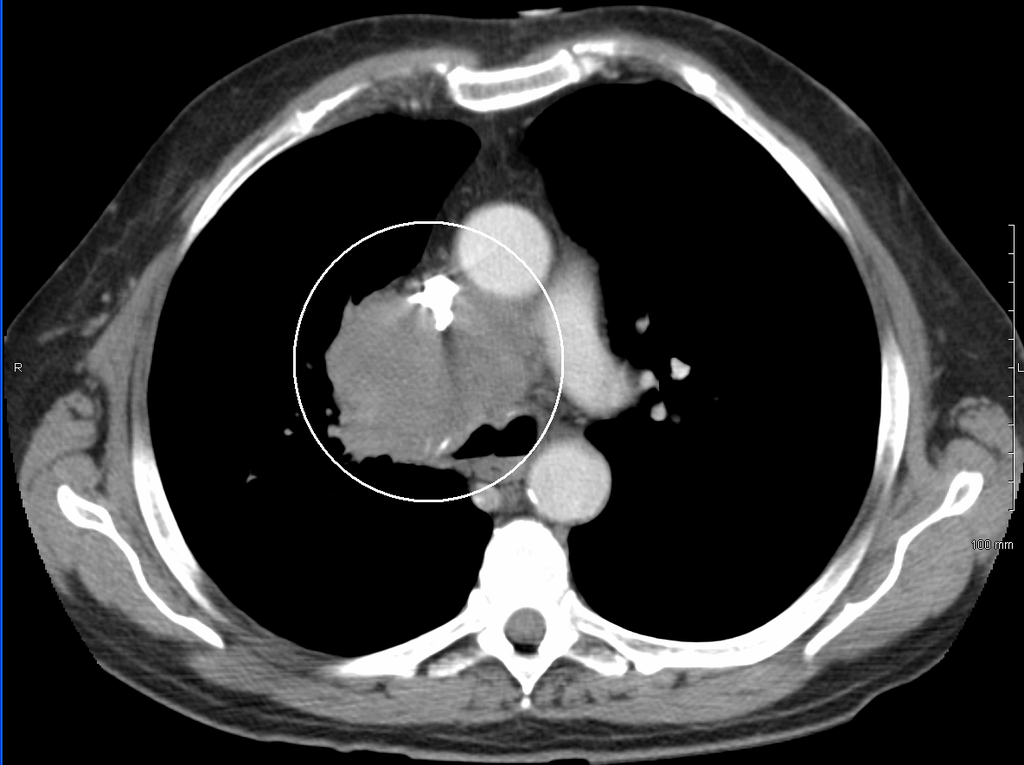
- CT chest with contrast: imaging modality of choice; shows the location and severity of obstruction and may help with identification/staging of underlying malignancy
- Doppler ultrasound: may help to identify the presence of obstruction
Biopsy
If the underlying malignancy is unknown, a biopsy can be performed via bronchoscopy or transthoracic needle aspiration.
Diagnosis
The diagnosis of SVCO can be made clinically for significant symptoms and a likely underlying aetiology. Otherwise, it can be made via a chest CT with contrast.
Management
The management of SVCO will depend on the underlying cause. In SVCO related to malignancy, treatment consists of managing symptoms and underlying cancer.
Initial treatment
Patients with airway obstruction will require emergency treatment:
- Securing the airway (endotracheal intubation, surgical airway)
- Corticosteroids
- Diuretics
- Endovascular stenting
- Radiotherapy
Symptomatic treatment for SVCO includes:
- Elevating the head
- Loosening restrictive clothing
- Benzodiazepines and opioids to relieve breathlessness and agitation
- Oxygen to maintain oxygen saturations if required
Managing the underlying cancer
Management of the underlying cancer may involve:
- Radiotherapy: most cancers associated with SVCO are radiotherapy sensitive
- Chemotherapy
- Corticosteroids: in the case of haematological malignancies
- Surgical resection
Complications
Complications of SVCO include:
- Laryngeal oedema
- Acute upper airway obstruction
Complications related to endovascular stenting include:
- Stent thrombosis
- Stent migration
- Superior vena cava dissection or perforation
- Infection
- Volume overload/acute decompensation of heart failure: due to the sudden increase in venous return after relief of the obstruction
Key points
- SVCO occurs when the normal venous drainage of the superior vena cava is blocked, most commonly due to compression from malignancy
- The most common malignancy associated with SVCO is lung cancer
- Patients will report symptoms of breathlessness, visual disturbance, dizziness and headache which is worse on bending forward
- Typical examination findings include oedema of the face, neck and upper limbs, venous distension and facial plethora
- Diagnosis is via a CT chest with contrast
- If the underlying malignancy is not known, then biopsies should be taken before treatment where possible
- Treatment consists of symptom management, stenting or radiotherapy to relieve the obstruction and management of the underlying malignancy
Editor
Dr Chris Jefferies
References
- Patient.co.uk. Superior Vena Cava Obstruction. Published 2022. Available from [LINK]
- BMJ Best Practice. Superior Vena Cava Syndrome. Published 2023. Available from [LINK]
- Radiopaedia. Superior Vena Cava Obstruction. Published 2023. Available from: [LINK]
- Scottish Palliative Care Guidelines. Superior Vena Cava Obstruction. Published 2019. Available from: [LINK]
Image references
- Figure 1. EMAHkempny. Superior vena cava syndrome. License: [CC BY-SA]
- Figure 2. Herbert L. Fred, MD and Hendrik A. van Dijk. SVCcombo. License: [CC BY]
- Figure 3. James Heilman, MD. SVCCT. License: [CC BY-SA]






