- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Intracranial haemorrhage is a term that covers several conditions in which there is bleeding within the brain. They typically occur following head injuries, and they can be differentiated depending on where the bleeding accumulates:
- Extradural haematoma (EDH)
- Subdural haematoma (SDH)
- Subarachnoid haemorrhage (SAH)
- Intracerebral haemorrhage (ICH)
Intracranial haemorrhages are diagnosed via a CT head scan. Identifying the different types of intracranial haemorrhage is a common exam question. This article summarises the key differences between each condition.
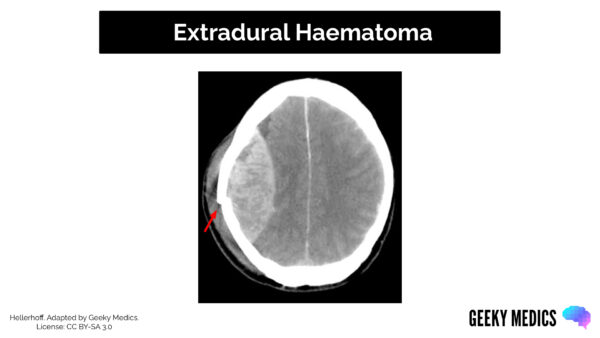
Extradural haematoma
Location
An extradural haematoma is defined as an acute haemorrhage between the dura mater and the inner surface of the skull.
Aetiology
EDHs are most common in adult males aged 20-30 and are generally caused by skull trauma in the temporoparietal region. The majority are caused by rupture of the middle meningeal artery (MMA) as it lies beneath the pterion – an anatomical landmark on the skull that is vulnerable to fracture following head trauma.
Clinical features
Typical clinical features of an EDH include headache, nausea, vomiting and confusion. They often have an immediate loss of consciousness followed by a period of lucidity. There is then a progressive decline in consciousness over the next few hours.
Depending on the size of the bleed, clinical examination may show:
- Reduced Glasgow Coma Score (GCS)
- Cranial nerve deficits
- Upper motor neurone syndrome
- Cushing’s triad: bradycardia, hypertension and deep/irregular breathing
CT scan appearance
Features of an EDH on a CT scan may include:
- Bi-convex “lemon-shaped” mass
- Midline shift
- Brainstem herniation
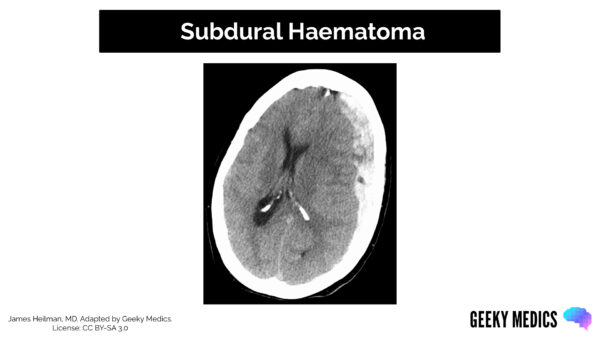
Subdural haematoma
Location
A subdural haematoma is defined as a haemorrhage between the dura mater and arachnoid mater of the brain.
Aetiology
SDHs also generally occur following head trauma or a fall and are more common in older patients, those at increased risk of falls and those with coagulation abnormalities (through coagulopathy or anticoagulant use).
The bleeding typically comes from the rupture of the bridging cranial veins after a blow to the temporal side of the head.
A SDH can be defined as acute (<3 days), subacute (3-21 days) or chronic (>21 days).
Clinical features
Typical clinical features of SDH include headache, nausea, vomiting and confusion. Patients may present with drowsiness or poor balance and tend to gradually deteriorate over the hours following the injury.
Depending on the size/location of the bleed, clinical examination may show:
- Reduced Glasgow Coma Score (GCS)
- Cranial nerve deficits
- Limb weakness or sensory disturbance
- Ataxia
- Seizures
CT scan appearance
Features of SDH on a CT scan may include:
- Crescent “banana-shaped” mass
- An acute SDH will have a hyperdense (bright white) appearance
- A chronic SDH will have a hypodense (black/grey) appearance
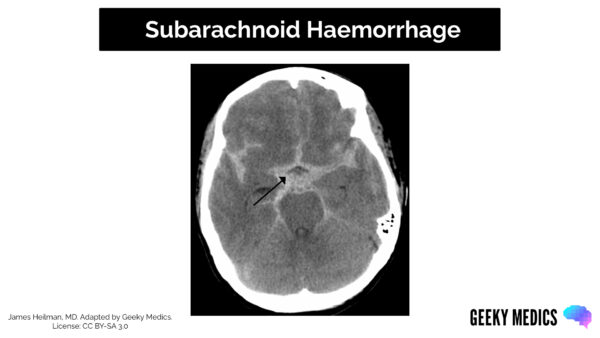
Subarachnoid haemorrhage
Location
A subarachnoid haemorrhage is defined as a haemorrhage into the subarachnoid space between the arachnoid mater and pia mater. It is considered a subtype of haemorrhagic stroke.
Aetiology
SAH is typically an arterial bleed and can be associated with trauma or may be spontaneous – this article will now focus on spontaneous SAH.
Spontaneous SAHs are caused by:
- Intracranial aneurysms: 70%
- Arteriovenous malformations (AVM): 10%
- Unknown/rare aetiology: 20%
Risk factors for spontaneous SAH include:
- Hypertension
- Smoking
- Family history
- Autosomal dominant polycystic kidney disease (ADPKD)
- Age > 50 years
- Female sex
Clinical features
Most aneurysms are asymptomatic until they rupture. Typical clinical features of a ruptured aneurysm are a sudden onset, severe headache (“thunderclap headache”), nausea and vomiting and photophobia.
Clinical examination may show:
- Reduced Glasgow Coma Score (GCS)
- Neck stiffness
- Kernig’s sign: inability to extend the knee due to pain when the patient is supine and the hip and knee are flexed to 90o
CT scan appearance
Features of a SAH on a CT scan may include:
- Hyperdensity around the circle of Willis
- Hyperdensity in the subarachnoid space
A CT angiogram may be used to help identify the presence of an aneurysm.
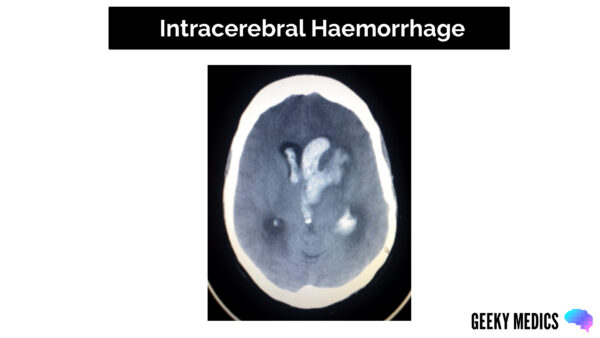
Intracerebral haemorrhage
Location
An intracerebral haemorrhage (also referred to as a haemorrhagic stroke) involves bleeding from a ruptured blood vessel. Depending on the exact location, it can be intraparenchymal (within the brain tissue) and/or intraventricular (within the ventricles).
Aetiology
Most ICHs occur due to small vessel disease (generally related to hypertension) but can also occur due to haemorrhagic transformation of an ischaemic stroke, vascular malformations or tumours.
Clinical features
The clinical features of an ICH will vary according to the blood vessel that ruptures, with sudden onset of neurological symptoms. Symptoms often include headache, nausea and vomiting, slurred speech and altered level of consciousness.
Clinical examination findings will depend on the vessel affected, but may include:
- Reduced Glasgow Coma Score (GCS)
- Limb weakness
- Sensory disturbance
- Visual disturbance
- Ataxia
CT scan appearance
Features of an ICH on CT scan include:
- Hyperdensity within brain parenchyma or ventricles
The location of the bleed and symptoms will depend on the blood vessel affected:
- Anterior cerebral arteries supply the anteromedial cerebrum
- Middle cerebral arteries supply the majority of the lateral cerebrum
- Posterior cerebral arteries supply the posterior cerebrum
Summary
Table 1. Types of intracranial bleeding
| Extradural haematoma | Subdural haematoma | Subarachnoid haemorrhage | Intracerebral haemorrhage | |
| Location | Between skull and dura mater | Between dura and arachnoid mater | Between arachnoid and pia mater | Within brain parenchyma or ventricles |
| Aetiology | Rupture of middle meningeal artery on temporal surface of the skull | Rupture of bridging cranial veins | Rupture of a berry aneurysm | Haemorrhagic stroke |
| Clinical features |
|
|
|
|
| CT scan appearance | Biconvex “lemon-shaped” hyperdensity | Crescent “banana-shaped” hyperdensity | Hyperdensity around circle of Willis | Hyperdensity within brain parenchyma |




