- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A stroke is an acute neurological deficit attributed to an acute focal injury of the brain, spinal cord, or retina by either a vascular occlusion (ischaemia) or haemorrhage.
Stroke is the second most common cause of death globally and is one of the leading causes of disability.1
Aetiology
The aetiology of a stroke is either ischaemic or haemorrhagic, with ischaemic stroke being the more common (being responsible for 71% of stroke globally).1
Ischaemic stroke
Large vessel atherosclerosis
Large vessel atherosclerosis is a common cause of ischaemic stroke.1 The buildup and subsequent rupture of atherosclerotic plaques leads to the occlusion of the blood supply. In Western populations, the most common site of atherosclerosis is the internal carotid artery, but the circle of Willis (a common source in Asian patients), vertebral arteries, and the aortic arch may also be sources.2
Small vessel occlusion
Small vessels are penetrating arteries that branch off large arteries of the circle of Willis to supply the deep subcortical and brainstem structures.1 These are responsible for lacunar strokes. These vessels lose blood supply due to a process called lipohyalinosis (narrowing due to exposure to high blood pressure), or an atheroma at the origin of the vessel may occlude blood flow.3
Cardioembolic ischaemic stroke
Cardioembolic ischaemic strokes occur when a piece of debris from the heart shoots off into the cerebral vasculature. The most common cause is atrial fibrillation.4 Other possible emboli are from endocarditis, venous clots that bypass pulmonary circulation through a patent foramen ovale (PFO), another septal defect, or a thrombus forming in an akinetic segment of a ventricle.5,6,7
Other rarer causes are as follows:
- Arterial dissection may cause a thrombus to form because tearing the intimal layer exposes the subintimal vessel surface that allows a clot to form.1 This is the most common cause in younger patients.
- Non-atherosclerotic arterial wall disease: vasculitis (inflammation of a blood vessel can lead to vessel narrowing) and vasoconstriction (drugs/cocaine, or reversible cerebral vasoconstriction syndrome).1,8,9
- Non-inflammatory vasculopathy: genetic conditions that cause narrowing of arteries, such as Moyamoya disease or fibromuscular dysplasia, are very rare causes of ischaemic stroke.10, 11
- Haematological disorders can make people more likely to have blood clots form. These may be inherited conditions such as sickle cell or homocystinuria, or acquired conditions such as leukaemias.12
- Cryptogenic: in over 25% of cases of ischaemic stroke, no cause of the stroke is found 13.
Haemorrhagic stroke
Haemorrhagic stroke refers to bleeding into the brain substance itself rather than the extra-parenchymal bleeds such as extradural and subdural haemorrhages.
The most common causes of intracerebral haemorrhage (ICH) are:
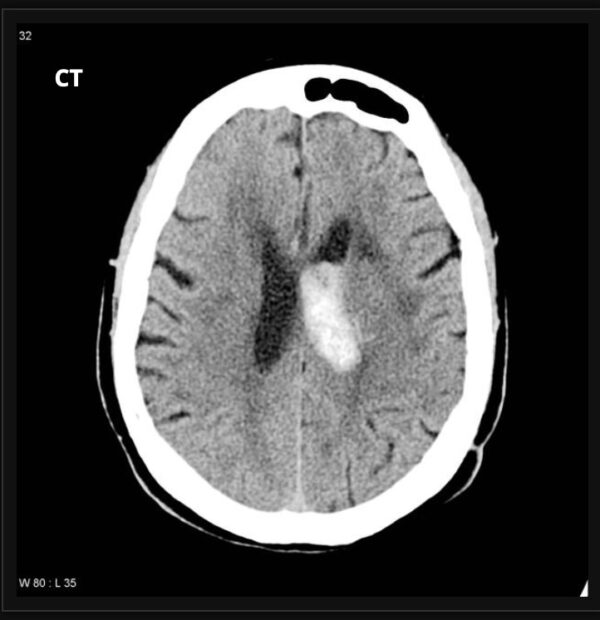
- Hypertension: hypertensive damage to small penetrating blood vessels branching off the MCA is the most common cause of intracerebral haemorrhage.14 This stereotypically leads to basal ganglia or thalamic haemorrhages (Figure 1).15
- Cerebral amyloid angiopathy: Amyloid deposition around blood vessels weakens blood vessel walls, making them liable to rupture.16 This tends to cause bleeding into the lobes rather than the deep matter of the brain (Figure 2).
Other causes of ICH are:
- Bleeding disorders: patients may have spontaneous bleeds due to an underlying bleeding disorder.14
- Drugs: anticoagulants increase the risk of spontaneous as well as traumatic bleeding.17 Sympathomimetic agents such as cocaine may also cause ICH.14
- Vascular malformations: various blood vessel problems such as cavernous angiomas and arteriovenous malformations may predispose to ICH.14
A subarachnoid haemorrhage is a further form of haemorrhagic stroke but with very different management priorities, and patients are normally cared for in neurosurgical units.
Risk factors
Physiological risk factors for stroke include:18
- High BMI
- High fasting plasma glucose
- High systolic blood pressure
- High LDL cholesterol
- Kidney dysfunction
Other risk factors include:18
- Tobacco smoking: including second-hand smoking
- Low physical activity
- Diet: high in sodium and red meat, low in fruit/ vegetable/ whole grains
- Alcohol consumption
- Environmental: air pollution, low ambient temperatures, lead exposure
Clinical features
History and examination are crucial in the identification of a stroke. For more information, see the Geeky Medics guide to stroke and TIA history taking.
History
The history should aim to establish the likelihood of a stroke through the following features:
- A focal neurologic deficit
- A persistent neurologic deficit
- A deficit that has come on acutely during the previous week (particularly less than 24 hours before presentation)
- No history of head trauma.
If all 4 of these factors are present, there is a 4 in 5 chance that the patient has had a stroke.
If 1-3 of these factors are present, the probability of stroke is increased above the baseline 10%, but it’s uncertain. If none of these 4 factors are present, the probability of a stroke is about 3 in 200.
Eligibility for thrombolysis
Key features to establish when considering eligibility for thrombolysis include:
- Time from onset of symptoms
- The time the patient was last known to be unaffected
- If the patient was asleep, whether they woke up with a deficit
- Do they have any conditions that might preclude thrombolysis, such as malignancy, recent surgery, or medical problems that mean they are usually on anticoagulants?
Stroke mimics
Assess for features which may suggest a stroke mimic (see the section on differential diagnoses):
- Is there any evidence that there was any seizure activity?
- Is there any headache indicating this could be a migraine or giant cell arteritis?
- Have they had longstanding issues to indicate that this could be a space-occupying lesion?
- Is there evidence or a history of malnutrition that could indicate Wernicke’s encephalopathy as a possibility?
- Is there a possibility there may be underlying endocarditis or an acute aortic syndrome which has precipitated the neurological symptoms?
Clinical examination
The most sensitive signs of a stroke outside of a hospital are facial droop, arm drift, and abnormal speech. 19 This explains why we have public awareness campaigns for FAST. These are good red flags a patient may have had a stroke, but these are not definitive once the patient reaches the hospital (i.e. they are a good screening tool but not diagnostic).
Examination within a hospital aims to identify a pattern of normal and abnormal findings to identify a possible affected vascular territory in ischaemia, as well as define stroke severity. The NIHSS scoring system guides the examination.
Differential diagnoses
Anything which disturbs neuronal function is a potential differential diagnosis of stroke. The brain is quite heterogeneous in its response to insults, and so a global insult may cause focal neurology.
Differential diagnoses to consider in the context of stroke (‘stroke mimics’) include:
- Todd’s Paresis: neuronal hypofunctioning following a seizure
- Hypoglycaemia: neurons need glucose to function, so lack of glucose will cause lack of function
- Old stroke: a new physiological insult can cause reappearance of old stroke symptoms
- Hemiplegic migraine/migraine aura: migraine is a brain disorder that changes the way neurons function
- Brain tumours or other space-occupying lesions: Local compression from lesions may cause focal neurology
- Hypertensive encephalopathy: a rare condition where chronically high blood pressure can cause cerebral blood vessel damage
- Functional neurological disorder: can present with stroke-like symptoms
- Central nervous system infection: either a cerebral abscess or encephalitis
- Wernicke’s encephalopathy: ataxia from Wernicke’s may be mistaken for a posterior circulation stroke
Investigations
Initial (‘front door’) investigations
Relevant initial investigations in the context of stroke include:
- Blood sugar: hypoglycaemia can be a very convincing stroke mimic.
- CT head: All patients with a suspected stroke should have an urgent CT-head; its purpose is mainly to rule out an intracerebral haemorrhage (in early ischaemic strokes, the CT-head appearances are usually normal).
- CT Angiogram and CT Perfusion: CT angiography and CT perfusion are further modalities which can establish eligibility for thrombolysis and thrombectomy. Patients eligible for thrombectomy should have CT-A immediately.20 However, not all hospitals in the UK have access to CT perfusion studies.
- Chest X-ray: a baseline chest x-ray is very important as the patients are at high risk of aspiration.
- ECG: catching an episode of AF or future episodes of AF may alter the patient’s long-term management. There may also be demand-induced myocardial ischaemia or centrally-mediated changes.
- Blood tests: U&E, LFTs, and pregnancy testing
A basic swallow assessment should be done at the front door.
Subacute investigations
Further relevant investigations include:
- 24-hour ECG recording (’24-hour tape’): to identify any episodes of atrial fibrillation, the duration of the tape (24h – 7 days) may vary
- Carotid dopplers: to identify carotid stenosis, patients with greater than 50% occlusion on the side of the stroke may be eligible for carotid endarterectomy.
- MRI: if an overt infarct cannot be identified on CT, an MRI can be performed. MRI can also help distinguish old strokes from new strokes using diffusion-weighted imaging.
- Lumbar puncture: for suspected subarachnoid haemorrhage (if CT normal) or CNS infection
- Echocardiogram: to identify a cardiac source of emboli
Stroke in younger people
Young stroke bloods are done in people under 50 who may have a rarer cause of stroke:
- Vasculitis screen (ANAs and ANCAs)
- Haematological causes of stroke: sickle cell, PCV, HIIT, homocysteine, antithrombotic deficiency (Protein C/S)
- HIV and syphilis
Diagnosis
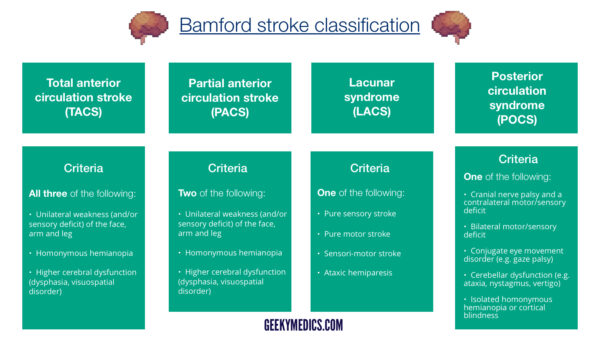
The diagnosis of a stroke relies on the history of symptom onset (i.e. is the history of an acute deficit in keeping with a vascular event) and the neurological deficit the patient has correlating with a neuroanatomical territory (like the Bamford classification).
This information is hopefully backed up by radiological data (i.e. proof of ischaemia or haemorrhage on MRI or CT). However, imaging doesn’t always provide all the answers, so it is important to still take a good history and know the neuroanatomy of the various stroke syndromes!
Management
The key to initial stroke management is identifying whether there is a bleed or ischaemia. After managing this in an acute setting, the priority is to identify why the bleeding or blockage happened in the first place. If we know this, we can modify the underlying risk factors to ensure the patient does not have another stroke.
Immediate management
For more information, see the Geeky Medics guide to the acute management (ABCDE approach) of a suspected stroke.
Ischaemic stroke
Immediate management for ischaemic stroke includes:
- Thrombolysis: thrombolysis involves the administration of a tissue plasminogen activator (tPA), such as alteplase or tenecteplase, to break down a clot. This is given within 4.5 hours or may be given up to 9 hours after stroke (see Royal College of Physicians criteria)
- Thrombectomy: thrombectomy involves using interventional radiology techniques to retrieve the clot and can be performed up to 24 hours after the stroke.
- Aspirin: 300mg aspirin can be started immediately or after 24 hours if thrombolysis has been given. Patients can continue on this for up to 2 weeks but sometimes may stop earlier (for example, if the stroke is due to atrial fibrillation, patients may start anticoagulants before the 2 weeks have elapsed)
- Decompressive hemicraniectomy: in some circumstances where there is a large area of the MCA territory infarction, resulting oedema in the infarcted tissue can cause raised intracranial pressure and require hemicraniectomy.
Haemorrhagic stroke
Immediate management for haemorrhagic stroke includes:
- Anticoagulant reversal: this can be achieved with vitamin K, prothrombin complex concentrate, or specific reversal agents, depending on the anticoagulant being taken
- Blood pressure control: if elevated, patients’ systolic blood pressure should be lowered to 130 and 140mmHg for up to a week after a bleed to prevent haematoma expansion
- Neurosurgical intervention: to evacuate a haematoma
Initial ward care
All patients with acute stroke should be admitted to an acute or hyperacute stroke unit (often called ASU or HASU). The multidisciplinary care provided in these units is associated with a significant improvement in survival.21
Medical issues in this phase are primarily aspiration risk and blood sugar control in diabetic patients, as well as managing VTE risk. Fever may occur following a stroke due to hypothalamic dysfunction. This can be managed with paracetamol, but infectious causes of fevers should also be ruled out.
Some patients may develop seizures and require antiseizure medications.
Blood pressure control doesn’t tend to be a huge issue in ischaemic stroke as there is very limited evidence of improvement in long-term prognosis after the first 6 hours.22 However, in ICH, patients should have strict BP control to have a blood pressure of <150 systolic for 7 days 23. BP should be maintained <185/110 for 24 hours in patients who have received intravenous thrombolysis.
Intermittent pneumatic compression is used for VTE prophylaxis for patients with reduced mobility after stroke.
In patients not known to have atrial fibrillation/flutter, cardiac rhythm monitoring should be performed for at least 24 hours, ideally as an inpatient
Management of underlying cause
The following should be considered for people who are inpatients with an ischaemic stroke:
- Endarterectomy if a carotid vessel is occluded by >50% on the side where a stroke has happened.24, 25 Endarterectomy should be done “as soon as possible”, ideally within a week.20, 26
- Cardiological or surgical intervention if there’s evidence that a cardiac lesion (such as endocarditis) is the cause of the stroke
Long term care
Long-term care for stroke focuses on rehabilitation from the neurological deficit, which requires multidisciplinary team input. Physiotherapists tend to manage weakness, occupational therapists will manage cognitive issues and any changes needed at home, and speech and language therapists will manage swallowing and speech issues.
Long-term medical care focuses on reducing the risk of subsequent strokes by modifying the risk factors. The underlying aetiology of the bleeding or ischaemia will drive the ongoing management. Given the numerous causes of stroke, the following is not exhaustive, but it encapsulates an overview of the management of the most common risk factors recommended in the 2023 RCP national stroke guideline:20
- Blood pressure: people with stroke or TIA should aim to have a clinic systolic blood pressure < 130mmHg
- Lipids: high-intensity statins (e.g. 80mg atorvastatin) should be started for atherosclerotic strokes
- Antiplatelets: after two weeks of 300mg aspirin, ischaemic stroke without evidence of AF should have 75mg clopidogrel OD long term. 75mg aspirin OD can be used if the patient cannot tolerate clopidogrel
- Anticoagulation: oral anticoagulation with a DOAC can be used after the initial aspirin if the cause of an ischaemic stroke is suspected to be AF
- Lifestyle factors: smoking, diet, and alcohol intake should also be addressed
Complications
Complications of stroke include:
- Aspiration events: due to swallowing dysfunction, it is common for stroke patients to aspirate, which increases their risk of pneumonia
- Long-term neurological deficit may occur when the patient does not recover from their stroke
- Seizures may occur in the acute phase, or some patients may go on to develop post-stroke epilepsy
- Cerebral oedema can occur if an acute ischaemic infarct is large enough. This may require neurosurgical intervention (a decompressive hemicraniectomy)
- Obstructive hydrocephalus can occur after haemorrhagic strokes, particularly in the posterior fossa, as the 4th ventricle can be compressed
- Ischaemic stroke can undergo haemorrhagic transformation
- Further stroke: once patients have had one stroke, they are vulnerable to having another, especially in the first few days after an event
Key points
- Stroke is an acute neurological deficit due to a vascular cause
- The aetiology of ischaemia is most commonly large vessel atherosclerosis, and the aetiology of haemorrhage is most commonly hypertensive blood vessel change
- Clinical features are determined by the neuroanatomical location of the stroke, which in ischaemic strokes can be assessed using the Bamford classification
- Investigations rely on imaging to assess for ischaemia and haemorrhage but also establish the underlying cause of the stroke
- Management can be segmented into hyperacute (thrombolysis and anticoagulation reversal, for example), short-term (managing complications on the ward), and long-term (risk factor modification and rehabilitation)
- Complications of stroke include haemorrhagic transformation, obstructive hydrocephalus, cerebral oedema and seizures
Reviewer
Dr Jacob Day
Neurology SpR
Editor
Dr Chris Jefferies
References
- Campbell BCV, De Silva DA, Macleod MR, et al. Ischaemic stroke. Nature Reviews Disease Primers. 2019;5(1):70.
- Holmstedt CA, Turan TN, Chimowitz MI. Atherosclerotic intracranial arterial stenosis: risk factors, diagnosis, and treatment. Lancet Neurol. 2013;12(11):1106-14.
- Nah HW, Kang DW, Kwon SU, Kim JS. Diversity of single small subcortical infarctions according to infarct location and parent artery disease: analysis of indicators for small vessel disease and atherosclerosis. Stroke. 2010;41(12):2822-7.
- Link MS, Giugliano RP, Ruff CT, et al. Stroke and Mortality Risk in Patients With Various Patterns of Atrial Fibrillation: Results From the ENGAGE AF-TIMI 48 Trial (Effective Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48). Circ Arrhythm Electrophysiol. 2017;10(1).
- Pruitt AA. Neurologic complications of infective endocarditis. Curr Treat Options Neurol. 2013;15(4):465-76.
- Mas JL, Derumeaux G, Guillon B, et al. Patent Foramen Ovale Closure or Anticoagulation vs. Antiplatelets after Stroke. N Engl J Med. 2017;377(11):1011-21.
- Vaitkus PT. Left ventricular mural thrombus and the risk of embolic stroke after acute myocardial infarction. J Cardiovasc Risk. 1995;2(2):103-6.
- Treadwell SD, Robinson TG. Cocaine use and stroke. Postgrad Med J. 2007;83(980):389-94.
- Ducros A. Reversible cerebral vasoconstriction syndrome. The Lancet Neurology. 2012;11(10):906-17.
- Ihara M, Yamamoto Y, Hattori Y, et al. Moyamoya disease: diagnosis and interventions. The Lancet Neurology. 2022;21(8):747-58.
- Harriott AM, Zimmerman E, Singhal AB, et al. Cerebrovascular fibromuscular dysplasia: The MGH cohort and literature review. Neurol Clin Pract. 2017;7(3):225-36.
- Arboix A, Jiménez C, Massons J, Parra O, Besses C. Hematological disorders: a commonly unrecognized cause of acute stroke. Expert Rev Hematol. 2016;9(9):891-901.
- Dalen JE, Alpert JS. Cryptogenic Strokes and Patent Foramen Ovales: What’s the Right Treatment? Am J Med. 2016;129(11):1159-62.
- Magid-Bernstein J, Girard R, Polster S, et al. Cerebral Hemorrhage: Pathophysiology, Treatment, and Future Directions. Circulation Research. 2022;130(8):1204-29.
- Zafar A, Khan FS. Clinical and radiological features of intracerebral haemorrhage in hypertensive patients. JPMA The Journal of the Pakistan Medical Association. 2008;58(7):356.
- Rodrigues MA, Samarasekera N, Lerpiniere C, et al. The Edinburgh CT and genetic diagnostic criteria for lobar intracerebral haemorrhage associated with cerebral amyloid angiopathy: model development and diagnostic test accuracy study. The Lancet Neurology. 2018;17(3):232-40.
- Tsivgoulis G, Wilson D, Katsanos AH, et al. Neuroimaging and clinical outcomes of oral anticoagulant–associated intracerebral hemorrhage. Annals of neurology. 2018;84(5):694-704.
- Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Neurology. 2021;20(10):795-820.
- Goldstein LB, Simel DL. Is This Patient Having a Stroke? JAMA. 2005;293(19):2391-402.
- Intercollegiate Stroke Working Party. National Clinical Guideline for Stroke for the UK and Ireland. London2023.
- Stephen M, Angus IGR, Ruth JB, et al. Impact and sustainability of centralising acute stroke services in English metropolitan areas: retrospective analysis of hospital episode statistics and stroke national audit data. BMJ. 2019;364:l1.
- Bath PMW, Krishnan K. Interventions for deliberately altering blood pressure in acute stroke. Cochrane Database of Systematic Reviews. 2014(10).
- Anderson CS, Heeley E, Huang Y, et al. Rapid Blood-Pressure Lowering in Patients with Acute Intracerebral Hemorrhage. New England Journal of Medicine. 2013;368(25):2355-65.
- Ferguson GG, Eliasziw M, Barr HWK, et al. The North American Symptomatic Carotid Endarterectomy Trial. Stroke. 1999;30(9):1751-8.
- Barnett HJM, Taylor DW, Eliasziw M, et al. Benefit of Carotid Endarterectomy in Patients with Symptomatic Moderate or Severe Stenosis. New England Journal of Medicine. 1998;339(20):1415-25.
- Kulkarni SR, Gohel MS, Bulbulia RA, Whyman MR, Poskitt KR. The importance of early carotid endarterectomy in symptomatic patients. Ann R Coll Surg Engl. 2009;91(3):210-3.
Image references
- Figure 1. Case courtesy of Frank Gaillard, Radiopaedia.org, rID: 10598
- Figure 2. Case courtesy of Jeremy Jones, Radiopaedia.org, rID: 6153