- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The invention of antibiotics had a profound impact on healthcare. In 2021, over 26 million antibiotic prescriptions were dispensed in the United Kingdom.1,2
The topic of antimicrobial resistance has been gaining traction.3 As such, knowledge of antibiotics is essential to improve antimicrobial stewardship. This article will explore antimicrobial stewardship and commonly prescribed antibiotics by drug groups. We will also discuss example drugs within groups, common indications, mechanism of action, side effects and key points.
Antimicrobial stewardship
Key principles of antimicrobial stewardship include:
- When prescribing, follow basic prescribing principles
- Ask for allergies and other medications, including over-the-counter and herbal medicines
- Write an indication for antibiotics on prescription, especially for in-patient (hospital) prescribed antibiotics
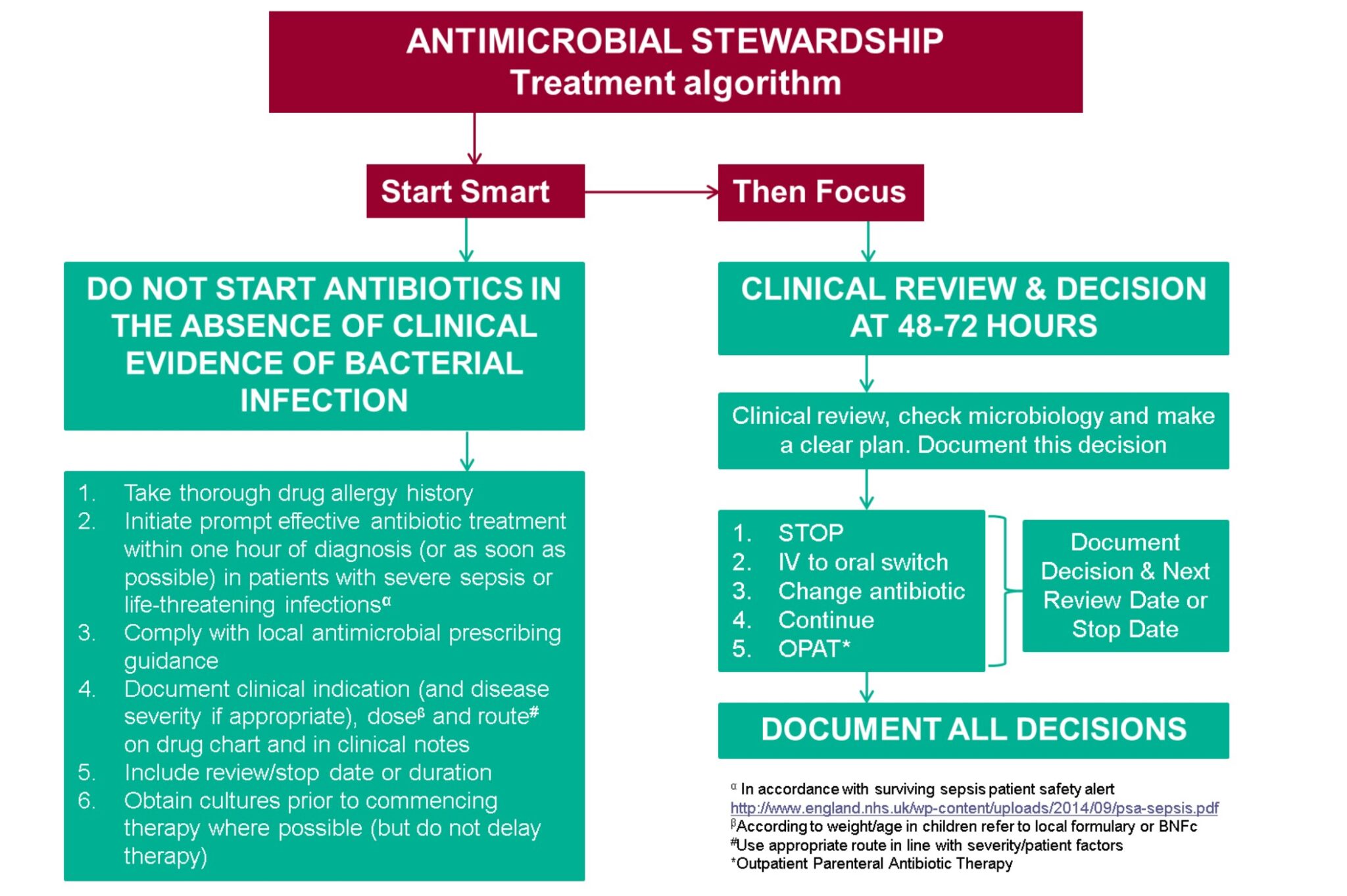
- Document a clinical review and decision date before commencing hospital antibiotics. Clinical review and decision are made 48-72 hours after starting an antibiotic. Decisions include: stopping antibiotics, switching from IV to the oral route, changing antibiotics, continuing antibiotics or discharge with outpatient antibiotic therapy – this guidance is known as ‘Start Smart – Then Focus’.4
Penicillins
Examples of penicillins include amoxicillin, flucloxacillin, phenoxymethylpenicillin and co-amoxiclav.
Common indications
Community and hospital-acquired pneumonia (amoxicillin), cellulitis (flucloxacillin), otitis media, sinusitis, group A streptococcal infection and rheumatic fever (phenoxymethylpenicillin).5
Amoxicillin is used to treat Helicobacter pylori infections in combination with other medications.
Mechanism of action
Penicillins are beta-lactam antibiotics.6 They inhibit enzymes called penicillin-binding proteins responsible for bacterial cell wall synthesis. This results in bacterial cell death.
Some bacteria have developed antibiotic resistance by producing beta-lactamase, an enzyme that inhibits the activity of penicillins. Co-amoxiclav contains amoxicillin and clavulanic acid. Clavulanic acid is a beta-lactamase inhibitor which counters the impact of beta-lactamase.
Side-effects
Penicillins are usually well tolerated, although the most common side effects are gastrointestinal-related (e.g. diarrhoea and vomiting).5
Some patients may have hypersensitivity towards penicillin, resulting in skin rashes or reactions. It is important to let patients know that mild to moderate reactions can be treated by taking an antihistamine. However, if they develop severe rashes or breathing difficulties, this may be an anaphylactic reaction, and they should seek medical attention immediately.7
Clostridium difficile
Some antibiotics are known to cause Clostridium difficile infection.8 This is due to the disruption of the natural gut flora and causes diarrhoea. The antibiotics that cause C. diff infection are known as the 4Cs:
- Co-amoxiclav
- Clindamycin
- Cephalosporins
- Ciprofloxacin
Stool samples should be requested if C. diff is suspected.9 First-line management is a 10-day course of oral vancomycin with increased fluid intake (e.g. oral rehydration salts).
Key points
Consider CURB-65 or CRB65 scoring when prescribing antibiotics for community-acquired pneumonia.10 These scoring systems are used to determine pneumonia’s severity. A score of 2 or more or 1 or more on CURB-65 or CRB65 may warrant hospital admission rather than community oral antibiotics.
Infectious mononucleosis, also known as glandular fever or kissing disease, is caused by the Epstein-Barr virus. This infection is commonly misdiagnosed as it presents similar to tonsillitis, resulting in antibiotics being prescribed (e.g. phenoxymethylpenicillin).
The use of penicillin in infectious mononucleosis is known to result in a widespread maculopapular rash (Figure 2).11 The exact mechanism is unknown, and antibiotics should be stopped if this occurs.

Tetracyclines
Examples of tetracyclines include doxycycline, lymecycline and oxytetracycline.
Common indications
Common indications for tetracyclines include:5
- Acne vulgaris
- Chlamydia
- Lyme disease
- Rosacea
- Atypical pneumonia (mycoplasma pneumonia)
Mechanism of action
Tetracyclines are bacterial protein synthesis inhibitors.6 Their primary mechanism of action is reversible inhibition of bacterial 30S ribosomal subunit. Inhibition effectively blocks the translation of mRNA into bacterial protein.
Side-effects
Like other antibiotics, a common side effect of tetracyclines is gastrointestinal disturbances.5 Photosensitivity is increased when taking tetracyclines, and patients should be advised to reduce exposure to sunlight and UV (e.g. tanning beds).
Tetracyclines cause tooth discolouration, enamel hypoplasia and deposit in growing bones. For these reasons, they are typically contraindicated in children <12.
Key points
Tetracyclines should not be prescribed to:5
- Pregnant women (tetracyclines are teratogenic)
- Women are breastfeeding, as they are secreted into breast milk
- Children <12
Tetracyclines are susceptible to chelation, making them less effective.12 They commonly interact with antacids that contain magnesium, aluminium, calcium and sodium bicarbonate. They also interact with calcium and iron supplements. Patients should be advised to separate taking tetracyclines and antacids or iron supplements by two to three hours.
Some indications, such as chlamydia, have a loading dose of 200mg followed by a maintenance dose of 100mg. Patients should be counselled specifically on this (e.g. two tablets or two 100mg capsules once daily followed by one tablet or one 100mg capsule once daily). Always check the BNF before prescribing.
A rare but important risk of tetracyclines is idiopathic intracranial hypertension (IIH).13 Symptoms and signs of IIH include headache, blurred vision and papilloedema. Tetracyclines should be stopped if IIH is diagnosed.
Macrolides
Examples of macrolides include azithromycin, clarithromycin and erythromycin.
Common indications
Macrolides have similar indications as penicillin antibiotics.5 Macrolides are typically used as 2nd-line alternatives to penicillin antibiotics when a patient has an allergy. Macrolides (clarithromycin) are used to treat pertussis (whooping cough).
Clarithromycin is used to treat H. pylori infections with other medications.
Mechanism of action
Macrolides are bacterial protein synthesis inhibitors.6 Their primary mechanism of action is the reversible inhibition of bacterial 50S ribosomal subunit. Inhibition effectively blocks the translation of mRNA into bacterial protein.
Side-effects
Macrolides are well-tolerated. Patients may complain of gastrointestinal disturbance.5 Macrolides are known to cause QT-interval prolongation.
Key points
Clarithromycin and erythromycin inhibit CYP3A4.5,14 These enzymes metabolise other medications, thereby increasing levels of other medications in the body.
A common example is warfarin, with clarithromycin and erythromycin leading to increased INR and an increased risk of bleeding. INR levels should be closely monitored, and the warfarin dose may need to be reduced.
There is an increased risk of rhabdomyolysis when clarithromycin or erythromycin are given with a statin. Concurrent use should be avoided, and statins should be stopped during treatment with these antibiotics.
Macrolides are useful 2nd line alternatives to penicillin antibiotics if there are allergies or contraindications.
Macrolides are known to cause QT-interval prolongation. Caution and close monitoring are advised when using other medications with the same effect. These medications include SSRIs, amiodarone, antipsychotics and quinolone antibiotics.
Quinolones
Examples of quinolones include ciprofloxacin and levofloxacin.
Common indications
Ciprofloxacin, as eye drops or eye ointments, is often used in eye conditions such as bacterial conjunctivitis and corneal ulcers.5 Ciprofloxacin eye drops can also treat acute otitis externa.
Quinolones are also sometimes used in lower respiratory tract infections (LRTIs). Ciprofloxacin is useful against Pseudomonas aeruginosa, an infection that can occur in cystic fibrosis patients.
Quinolones are also used for urinary tract infections (mainly ofloxacin) and gastrointestinal infections (e.g. Shigella, Campylobacter, Salmonella).
Quinolones are the first line for prostatitis (NICE recommends a 14-day course of quinolones).
Ciprofloxacin is used as the prophylactic treatment of contacts with patients affected with meningococcal meningitis.
Mechanism of action
Quinolones act by inhibiting bacterial DNA synthesis.6 They are DNA gyrase (topoisomerase II) and topoisomerase IV inhibitors.
Quinolones are effective against aerobic gram-negative bacteria. These bacteria are common causative organisms in urinary tract and gastrointestinal infections.
Side-effects
Quinolones commonly cause gastrointestinal disturbances, other side effects include:5
- Neurological: quinolones are known to lower seizure thresholds and should be used cautiously in patients with or at risk of seizures
- Musculoskeletal: quinolones damage muscle tendons, putting patients at risk of tendon rupture
- Cardiovascular: quinolones prolong the QT interval and can risk the development of arrhythmias
Key points
The key points of quinolones are related to their side effects.
Quinolones should be avoided in women who are pregnant or breastfeeding.5 They are also contraindicated in patients with glucose-6 phosphate dehydrogenase (G6PD) deficiency.
MHRA advice
The Medicines and Healthcare Products Regulatory Agency (MHRA) has released a drug safety update warning about the risks of quinolones. A patient information sheet has been developed for patients prescribed quinolone antibiotics. This includes information on the symptoms of rare but serious side effects.
Trimethoprim and sulphonamides
Co-trimoxazole is trimethoprim and sulfamethoxazole (a sulphonamide).
Common indications
Trimethoprim is a first-line antibiotic for uncomplicated urinary tract infections (UTIs), with alternatives being nitrofurantoin and amoxicillin.5 It is also used for catheter-associated UTIs, acute pyelonephritis, acute prostatitis, acute diverticulitis, acne resistant to other antibiotics, shigellosis and respiratory tract infections.
Co-trimoxazole can be given as treatment and prophylaxis of Pneumocystis jirovecii infections which may occur in immunosuppressed patients, for example, due to human immunodeficiency virus (HIV). It is occasionally used in hospital-acquired pneumonia, acute exacerbation of COPD, leg ulcer infections and moderate and severe diabetic foot infections.
Mechanism of action
Bacteria require folate for DNA synthesis but cannot use external sources of folate.6 Trimethoprim is a dihydrofolate reductase inhibitor. This enzyme is responsible for bacterial folate synthesis. Thereby, trimethoprim reduces bacterial growth.
Trimethoprim has a broad spectrum of activity against gram-positive and gram-negative organisms, particularly Escherichia coli. However, its clinical usefulness is limited to the widespread development of bacterial resistance.
Sulfonamides, such as sulfamethoxazole, also impair bacterial folate synthesis. Combined with trimethoprim, folate synthesis will be completely inhibited, so they are bactericidal.
Side-effects
The most common side effects of trimethoprim are gastrointestinal disturbance and skin rashes.5
There is restricted use of sulfonamides due to them commonly causing anaphylactic reactions, erythema multiforme and drug fever. This rarely occurs with trimethoprim. Due to folate antagonism, they can impair haematopoiesis, resulting in megaloblastic anaemia, leucopenia, and thrombocytopenia. There is also a risk of hyperkalemia and renal impairment.
Key points
Trimethoprim is teratogenic in the first trimester of pregnancy as it is a folate antagonist, which can cause cardiovascular defects and oral clefts in a foetus.5 They are generally avoided during pregnancy, with nitrofurantoin used as an alternative (however, nitrofurantoin is not advised in the third trimester or when breastfeeding).
Trimethoprim combined with potassium-elevating drugs (e.g. aldosterone antagonists, ACE inhibitors and ARBs) can increase the risk of hyperkalemia.
Avoid using other folate antagonists alongside trimethoprim, such as methotrexate, and medications that increase folate metabolism, such as phenytoin, due to adverse haematological effects.
Nitrofurans
The most common example of a nitrofuran is nitrofurantoin.
Common indications
Nitrofurantoin is commonly used as a first-line treatment for uncomplicated lower urinary tract infections, with the alternatives being trimethoprim and amoxicillin.5 It can also be used for catheter-associated UTIs, severe chronic recurrent UTIs, pregnancy first/second trimester UTIs, and as prophylaxis of UTIs.
Mechanism of action
Nitrofurantoin is reduced to its active form with nitrofuran reductase found in bacterial cell walls. The resultant active metabolite impairs bacterial DNA, causing cell death.6
Nitrofurantoin is active against gram-negative organisms such as Escherichia coli, and Gram-positive organisms like Staphylococcus saprophyticus, commonly responsible for UTIs. Nitrofurantoin achieves therapeutic levels in the urine via renal excretion. Its bactericidal effect is optimal in acidic environments, such as urine.
Side-effects
Gastrointestinal upset is the most common side effect of nitrofurantoin.5 It may also cause hypersensitivity reactions and discolouration of the urine to dark yellow or brown. Less commonly, prolonged use can cause hepatitis, pneumonitis, pulmonary fibrosis and peripheral neuropathy. There is also the risk of haemolytic anaemia in neonates.
Key points
Nitrofurantoin should be avoided in pregnant women towards term and infants under three months old.5 It is generally avoided in renal impairment due to the risk of toxicity.
Nitroimidazoles
The most common example of a nitroimidazole is metronidazole.
Common indications
Metronidazole is commonly used to treat dental abscesses and anaerobic infections.5 They also treat protozoal infections such as trichomoniasis (trichomonas vaginalis) and bacterial vaginosis (gardnerella vaginalis).
Metronidazole is used to treat helicobacter pylori (H. Pylori) infection and pelvic inflammatory disease in combination with other medications.
Topical metronidazole is used in the management of rosacea.
Mechanism of action
Metronidazole is passively diffused through the cell wall of susceptible organisms.6 It is then reduced to its active form and results in the formation of a nitroso-free radical. Subsequently, these metabolites interact with DNA resulting in the inhibition of DNA synthesis and DNA degradation.
Aerobic bacteria are not susceptible to metronidazole as they cannot reduce metronidazole to its active form.
Side-effects
The most common side-effect patients have is a gastrointestinal disturbance.5 Patients may complain of a metallic taste when taking metronidazole.
Prolonged or high doses of metronidazole can cause optic neuritis, seizures or peripheral neuropathy.
Key points
Patients should not drink alcohol while on a course of metronidazole (oral, rectal or vaginal) or for 48 hours after finishing the course.5, 15 Metronidazole has a disulfiram-like reaction with alcohol. Metronidazole inhibits aldehyde dehydrogenase resulting in the accumulation of the toxic metabolite acetaldehyde.16 Symptoms with concurrent use include flushing, nausea, vomiting, abdominal pain, headaches, syncope and tachycardia.
Editor
Dr Chris Jefferies
References
- Mikulic, M. Total consumption of antibiotics in England in 2021, by antibiotic group. Published in 2023. Available from: [LINK]
- Mikulic, M. Leading 10 antibacterial drugs dispensed in England in 2022, by number of items. Published in 2023. Available from:[LINK]
- GOV UK. UK 5-year action plan for antimicrobial resistance 2019 to 2024. Published in 2019. Available from: [LINK]
- GOV UK. Antimicrobial stewardship: Start smart- then focus. Published in 2015. Available from: [LINK]
- British National Formulary. Published in 2023. Available from: [LINK]
- Ritter, JM. Flower, RJ, Henderson, G. Loke, TK. MacEwan D. Rang. H. Rang & Dale’s Pharmacology 9th Edition. 2018.
- NHS. Side effects antibiotics. Published in 2022. Available from: [LINK]
- Marwick CA. Yu, N. Lockhart, MC. McGuigan CC. Wiuff, C. Davey, PG. Donnan, PT. Community-associated Clostridium difficile infection among older people in Tayside, Scotland, is associated with antibiotic exposure and care home residence: cohort study with nested case-control. Published in 2013. Available from: [LINK]
- NICE CKS. Diarrhoea – antibiotic associated. Published in 2021. Available from: [LINK]
- NICE CKS. Chest infections – adult. Published in 2021. Available from: [LINK]
- Onodi-Nagy, K. Kinyo A. Meszes, A. Garaczi, E. Kemeny, L. Bata-Csorgo, Z. Amoxicillin rash in patients with infectious mononucleosis: evidence of true drug sensitization, Published in 2015. Available from: [LINK]
- MedlinePlus. Tetracycline. Published in 2017. Available from: [LINK]
- Medsafe. Idiopathic Intracranial Hypertension. Published in 2016. Available from: [LINK]
- NHS Greater Glasgow and Clyde. PostScriptAcute. Published in 2013. Available from: [LINK]
- NHS. About metronidazole. Published in 2021. Available from: [LINK]
- Alonzo, MM. Lewis, TV. Miller, JL. Disulfiram-like Reaction With Metronidazole: An Unsuspected Culpit. Published in 2019. Available from: [LINK]
Image references
- Figure 1. Public Health England. Start Smart – Then Focus – Antimicrobial Stewardship Toolkit for English Hospitals. License: [OGL]
- Figure 2. Matibot. Infectious Mononucleosis and Ampicillin cross-reaction rash. License: [CC BY-SA]




