- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A 26-year-old man presents to the medical assessment unit with pain on inspiration. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
- Pain on inspiration
- Chest pain
History
Presenting complaint
“It’s this pain in my chest, it’s really bothering me especially when I take a breath.”
History of presenting complaint
Where is the pain?
“It’s right in the middle of my chest”
Did anything happen to trigger the pain? Did it come on suddenly or gradually?
“It started suddenly this morning, but I can’t think of anything that set it off. I didn’t hit my chest or do anything!”
What kind of pain is this? (e.g. sharp, aching, burning) Is it continuous or intermittent?
“It’s sharp and always there.”
Does the pain move anywhere else?
“No, not that I’ve noticed, it’s just in my chest.”
Are there any other symptoms that seem associated?
“I’ve been a bit short of breath for the last couple of days”
Does anything make it better or worse?
“It gets worse when I breathe in. It catches my breath and is really sharp. I tried paracetamol but that didn’t really help.”>
On a scale of 1-10, how bad is the pain?
“The pain is about 6 out of 10 at its worst.”
Have you experienced chest pain in the past?
“No, I’ve never had anything like this before.”
Other parts of the history
Past medical and surgical history
- Do you have any medical conditions?
- Have you ever been admitted to the hospital before?
- Have you had any operations before?
“I’ve got asthma, it was pretty bad when I was young and I was admitted to the hospital a few times, but it doesn’t cause me much bother now.”
Medication history/allergies
- Does he take any regular medication?
- Does he have any allergies?
“I have a pink and blue inhaler and montelukast tablets for my asthma, but that’s it. I come out in a bit of a rash if I have penicillin.”
Family history
- Do any medical problems run in the family?
“Just asthma.”
Clinical examination
Examination findings:
- HR 112, RR 22, BP 118/64, Oxygen saturation 94% on air, Temperature 36.5oC
- Bilateral expiratory wheeze on auscultation
- Reduced air entry on the right
- Normal heart sounds
- No peripheral oedema
- Calves are soft and non-tender
Investigations
ECG
The patient’s ECG is shown below:
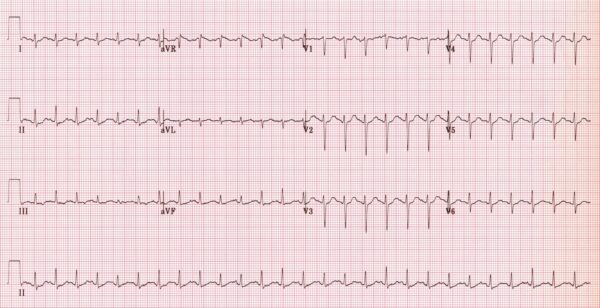
Sinus tachycardia
Diagnosis
- Pulmonary embolism
- Pneumothorax
- Musculoskeletal pain
- Pneumonia
- Pleural effusion
- Pleuritis
- Pericarditis
- Myocardial infarction
- Trauma
Chest X-ray
The patient’s chest X-ray results are shown below.
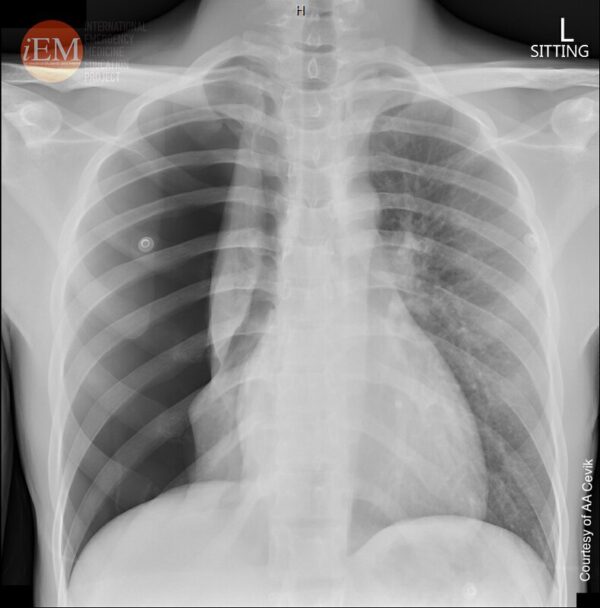
He has a large, secondary pneumothorax.
Pneumothoraces can be primary or secondary depending on whether the patient has an underlying lung disease.
They can be small or large, depending on the distance from the parietal pleural edge (ribs) to the visceral pleural edge (lung) at the level of the hilum. A distance of 2cm is the cut-off value.
Management
The best option would be a Seldinger intercostal chest drain. As per the British Thoracic Society’s management of pneumothorax guideline large secondary pneumothoraces should be managed with a chest drain2.
Seldinger drains are smaller and better tolerated by patients than surgical chest drains, and are usually sufficient.
Complications
Those who need a referral to cardiothoracic surgeons can be divided into those with failed “medical” therapy and those with a high risk of harm from further pneumothorax.
Failure of “medical” therapy is usually due to a persistent air leak. The pneumothorax hasn’t resolved despite drainage and additional low-flow suction on the drain.
Those at high risk of harm from further pneumothorax include those who have had bilateral pneumothoraces, pregnant women, and professional divers or airplane pilots.
Editor
Dr Jess Speller
References
- theSimTech. Sinus Tachycardia. Available from: [LINK]
- Emergency Medicine Clinical Images and Video. Spontaneous Pneumothorax. License: [CC BY-NC-SA].
- MacDuff et al. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax. Published in 2010. Available from: [LINK]
- Patient.co.uk. Pneumothorax. Published 2022. Available from: [LINK]




