- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A 32-year-old woman who is currently pregnant presents to the birth unit due to reduced fetal movements. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
- Normal pregnancy and antenatal care
- Pregnancy risk assessment
- Reduced/change in fetal movements
History
Presenting complaint
“Sorry but please could I be seen by someone, my baby isn’t moving as much and I’m really worried.”
History of presenting complaint
How far along are you in this pregnancy?
“I am 32 weeks and 2 days (32+2) today”
When did you first notice a change in the baby’s movements?
“He hasn’t moved much since I woke up today, which is unusual as he’s usually most active in the morning”
Are baby’s movements reduced in nature, frequency, or both?
“Both, but mostly in nature”
Have there been any significant bumps or knocks to your abdomen recently?
“My four-year-old daughter jumped on me when I was lying on the couch yesterday evening. I didn’t think much of it at the time, but it did hurt!”
Have you had any fluid loss/leaking from down below?
“No”
Have you noticed any bleeding on wiping, or on your underwear?
“No”
Have you experienced any painful tightenings or abdominal pain?
“No, just occasional Braxton-Hicks tightenings, which are normal for me”
Have you noticed any other unusual symptoms today, including headache or abdominal pain?
“No, I otherwise feel well”
Other parts of the history
What number pregnancy is this for you, including miscarriages and terminations?
“This is my fourth pregnancy. I had my daughter three years ago, and an early miscarriage last year. I also had a surgical termination when I was 19.”
Who is looking after you in in this pregnancy?
“I am seeing a group practice midwife this pregnancy.”
Have you ever had any obstetric or gynaecological procedures performed?
“I had a laparoscopy for endometriosis 5 years ago”
Are your cervical screening tests up to date?
“Yes, my last test was two years ago, and was normal.”
Is this the first time you’ve noticed a change in baby’s movements in this pregnancy?
“Yes, this is the first time”
Did you need any help conceiving this pregnancy, such as with IVF?
“No, we fell pregnant the natural way”
Do you smoke or use any other substances?
“No, never”
How has this pregnancy been progressing? Have you had any trouble with your blood pressure (such as pre-eclampsia) or blood sugar (such as gestational diabetes)?
“I was quite nauseous in my first trimester but other than that I’ve been well. My glucose test was normal, and my blood pressure has always been on the lower side of normal”
Were any issues identified on your first-trimester screening, or on any tests in this pregnancy?
“Not that I know of, my first-trimester screening was reassuring, and as far as I know, there haven’t been any other issues”
When was your last ultrasound?
“My last ultrasound was my morphology scan, at 19 weeks”
During your consultation, you should also be aware of and note other risk factors for an adverse outcome, including ethnicity, advanced maternal age, and increased BMI.
Clinical examination
- Maternal observations, particularly blood pressure
- Measurement of symphyseal-fundal height
- Abdominal palpation, particularly feeling for uterine tone and any pain on palpation of the fundus
- Targeted maternal physical examination (depending on the presence or absence of associated symptoms)
A speculum or internal examination is generally not required to assess reduced fetal movements unless the clinical history raises concern for antepartum haemorrhage or rupture of membranes.
Examination findings
Observations
- HR 65
- BP 110/75
- T 36.7oC
- RR 14
- Oxygen saturation 97% on air
- Symphyseal-fundal height 31cm
- Longitudinal lie
- Fundus soft and non-tender
- No uterine activity noted on palpation
Investigations
Cardiotocography (CTG) is the most appropriate first-line investigation and should be performed on all women presenting with reduced fetal movements after 23 weeks gestation (prior to 23 weeks, fetal heart auscultation is performed instead of CTG).
All women who present with reduced fetal movements should at least receive a CTG as part of their assessment.
The Kleihauer-Betke (Kleihauer) test tests for fetal-maternal haemorrhage (FMH).
It is an acid elution test that detects and quantifies the presence of fetal haemoglobin within red blood cells in maternal circulation, indicating that fetal blood cells have crossed the placental interface. In reduced fetal movements (such as this case) a positive Kleihauer is associated with increased fetal morbidity and mortality, with underlying causes including placental abruption.
The Kleihauer test is also used in other circumstances in pregnancy, particularly to calculate the dose of Anti-D required following sensitising events where a mother has a Rhesus negative blood group.
CTG output
The patient’s CTG output is shown below.
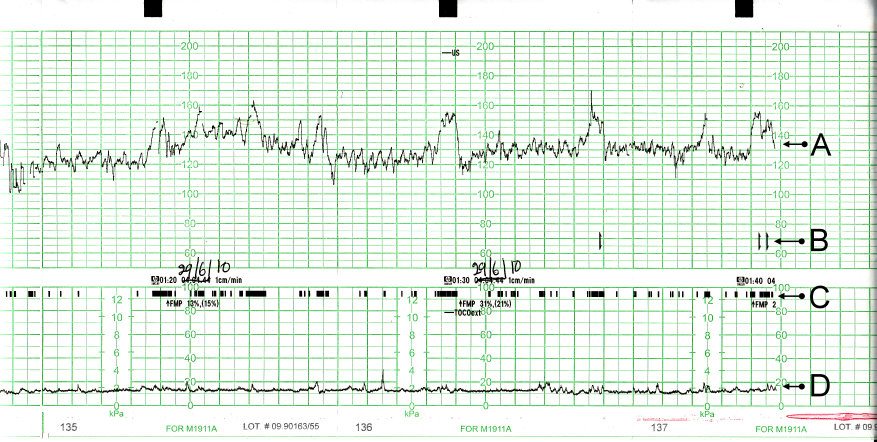
The acronym DR C BRAVADO can be used to systematically approach a CTG:
- Define risk (DR): This pregnancy is low-risk, however, the patient has presented with reduced fetal movements, which increases her risk of a complication
- Contractions (C): No uterine activity is seen on tocography
- Baseline rate (BR): 125-130bpm
- Accelerations (A): Present
- Variability (Va): ~10bpm
- Decelerations (D): None seen
- Overall impression (O): This is a reassuring antenatal CTG appropriate for a 32-week fetus. Note that the CTG is detecting fetal movements (indicated by the small black lines on the tocography component of the trace) and that Sarah is clicking the button attached to the CTG machine to indicate that she is feeling these (indicated by the “[” markers on the trace)
In the CTG above, A shows the fetal heartbeat, B shows the movements felt by the mother, C represents fetal movement and D shows uterine activity.
Diagnosis
- Fetal death in utero (FDIU), particularly if a woman reports absent fetal movements
- Placental insufficiency and fetal growth restriction
- Fetal-maternal haemorrhage (which may be acute or chronic), such as associated with trauma or massive placental abruption
- Other causes of fetal compromise, including TORCH infections
Other causes can include fetal sleep and the effect of maternal medications (such as following a general anaesthetic). In the vast majority of cases, no specific cause for reduced movements is found.
Management
In the absence of other risk factors, the patient can be discharged home with a plan for routine follow-up in the antenatal clinic.
Some guidelines recommend also offering an outpatient ultrasound, but this is not urgent. Otherwise, specific management for this episode of reduced fetal movements is not required. It is very important to counsel the patient to seek care again if she experiences further episodes of reduced fetal movements.
At 39+5 weeks, the patient will be at term. Reduced fetal movements in late pregnancy are generally considered an indication to offer induction of labour or caesarean section delivery because of a known association with placental dysfunction and stillbirth.
This is an individualised decision and should be discussed with a senior obstetric clinician.
Editor
Dr Jess Speller
References
- PhantomSteve. CTG image. License: [CC BY-SA].
- Stillbirth Centre for Research Excellence. Reduced fetal movements clinical practice guideline. Published in 2019. Available from: [LINK]
- King Edward Memorial Hospital. Decreased fetal movement clinical practice guideline. Published in 2018. Available from: [LINK]
- NHS. Reduced fetal movement in pregnancy guidelines. Published in 2019. Available from: [LINK]




