- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
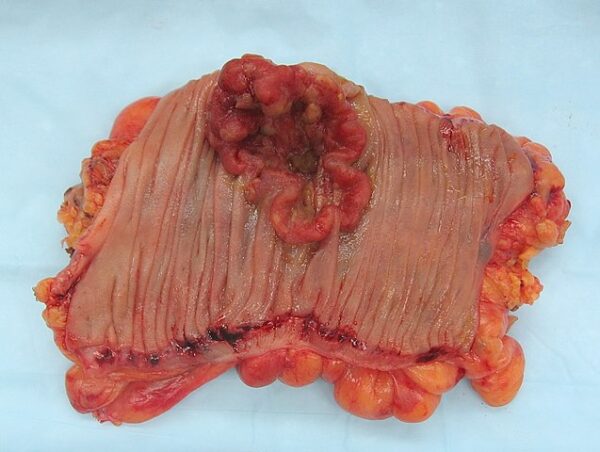
Colorectal cancer is caused by abnormal cell growth in the large intestine (caecum, colon, rectum). Adenocarcinoma is the most common type of colorectal cancer (in >95% of cases).1,2
Around 40,000 new colorectal cancers are diagnosed each year in the UK, and up to a quarter of these are diagnosed following screening. A full-time GP is likely to diagnose approximately one person with colorectal cancer every year.3
The 5-year survival is usually good, and it is a treatable cancer, but this is determined by the stage at which the diagnosis is made and what treatment options are available to individual patients.
Aetiology
Most colorectal tumours arise from pre-cancerous polyps. The normal colorectal epithelium can transform into an adenoma, which can finally become invasive and metastasise.
Alteration in mechanisms involved in DNA repair and cell proliferation results in the formation of discrete adenomas.
The chromosomal instability (CIN) pathway accounts for approximately 85% of adenocarcinoma transitions. It includes suppression of the tumour suppressor genes APC and TP53, the activation of the oncogenes BRAF and KRAS, and chromosome 18 alteration.7.8
Risk factors
Genetic risk factors include:5
- Family history: heritable factors represent up to 35% of colorectal cancer
- Polyposis syndromes (5-10% of cancers): hereditary non-polyposis colorectal cancer (HNPCC) (Lynch syndrome) and familial adenomatous polyposis (FAP)
Lifestyle/environmental factors include:
- Low fibre diet
- Physical inactivity
- Obesity
- Smoking
- Alcohol
Medical risk factors include:6
- Inflammatory bowel disease
- Acromegaly
- Previous history of colorectal cancer
- Diabetes mellitus
Clinical features
Patients with colorectal cancer may be asymptomatic and only diagnosed following screening. Alternatively, patients may present in primary care with red flag features (e.g. change in bowel habit, rectal bleeding) requiring urgent investigation and referral.
Some patients may present acutely with complications related to advanced disease (e.g. bowel obstruction or perforation).
History
Typical symptoms of colorectal cancer may include:
- Change in bowel habit: diarrhoea or constipation (persistent and unexplained)
- Rectal bleeding: fresh red or darker red, mixed in with the stool or on the toilet paper, at the beginning or end of defecation, every time or intermittently
- Abdominal pain
- Abdominal bloating
- Tenesmus
- Unexplained weight loss (suggests advanced disease)
- Fatigue/breathlessness (symptoms of anaemia)
Some patients with colorectal cancer may present with an unexplained deep vein thrombosis.
Other important areas to cover in the history include:
- Past medical history: to identify risk factors for colorectal cancer (e.g. IBD) or hereditary polyposis syndromes
- Family history
Clinical examination
Patients with rectal cancer may have a rectal mass on PR examination.
In advanced disease, there may be an abdominal mass on abdominal examination.
Other general clinical features may include:
- Cachexia
- Signs of anaemia
- Lymphadenopathy
NICE urgent suspected cancer referral
NICE advises performing faecal immunochemical testing (FIT) in patients with red flag features:
- Change in bowel habit
- Abdominal mass
- Iron deficiency anaemia
- Age >40 with unexplained weight loss and abdominal pain
- Age <50 with rectal bleeding and abdominal pain or weight loss
- Age >50 with unexplained rectal bleeding, abdominal pain or weight loss
- Age >60 with anaemia
If the FIT is positive (>10 micrograms of haemoglobin/gram of faeces), the patient should be referred on an urgent suspected cancer (two-week wait) referral pathway.10
Differential diagnoses
Colorectal polyps
Colorectal polyps are often asymptomatic and may be found incidentally during colonoscopy.
Larger polyps are rare but may present with similar symptoms to colorectal cancer (e.g. small amount of blood in stool, change in bowel habit).
Polyps are usually harmless, but in a small number of cases, they can undergo malignant transformation. Polyps are usually removed while having a colonoscopy (polypectomy).
Inflammatory bowel disease (IBD)
IBD (such as Crohn’s disease and ulcerative colitis) may present with similar symptoms to colorectal cancer, including changes in bowel habit, blood in stool, mucus in stool, abdominal pain, weight loss and anaemia.
IBD may also present with extra-intestinal features which would not be seen commonly in colorectal cancer (e.g. erythema nodosum, ophthalmic symptoms and MSK symptoms).
Other cancers
Other cancers may also present with generic red flag symptoms (e.g. weight loss).
Haemorrhoids
Haemorrhoids are swollen vascular mucosal cushions within the anal canal. They are either external or internal, depending on their location in the anal canal. External haemorrhoids are often painful and itchy. Internal haemorrhoids may have a degree of prolapse.
Haemorrhoids often present with bright red rectal bleeding, which is often associated with defecation. The diagnosis is made through history and physical examination.
Coeliac disease
Coeliac disease may present with features similar to colorectal cancer, including diarrhoea, iron deficiency anaemia, and weight loss.
However, patients may have a family history of coeliac disease, associated autoimmune conditions, and extra-intestinal features (e.g. dermatitis herpetiformis).
Investigations
Bedside investigations
Relevant bedside investigations include:
- Weight/BMI: to quantify weight loss
Laboratory investigations
Relevant laboratory investigations include:
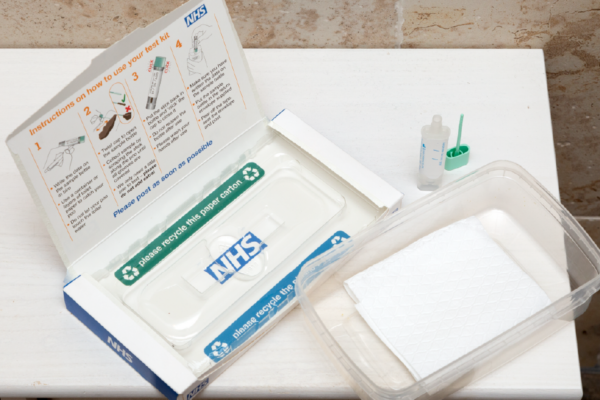
- Stool faecal immunochemical testing (FIT): used to detect small amounts of blood in the faeces, which could indicate colorectal cancer. It is usually performed in primary care and is part of the bowel cancer screening programme.
- Full blood count: to identify anaemia (usually microcytic if iron deficiency)
- Iron studies: to identify iron deficiency
- Urea and electrolytes: as a baseline before investigations or treatment
- Inflammatory markers (CRP/ESR):
- Liver function tests: as a baseline before investigations or treatment
- Tissue transglutaminase: to investigate for coeliac disease
More specialist tests may include:
- Carcinoembryonic antigen (CEA): used for monitoring treatment and disease progression, not used for screening or diagnosis
- Genetic testing (including HNPCC, FAP and others): if there are specific concerns regarding these hereditary conditions
Colonoscopy
Colonoscopy with biopsy is the gold-standard diagnostic test (sometimes, if rectal bleeding is present, a flexible sigmoidoscopy with biopsy is offered).
CT colonography is used for those for whom colonoscopy is unsuitable (patient or technical factors).
If a suspicious lesion is located, it is biopsied and tattooed (unless rectal or caecal).
Imaging
Relevant imaging investigations include:
- CT chest, abdomen and pelvis: patients with suspected colorectal cancer at colonoscopy or CT colonography will require completion CT to look for staging
- MRI pelvis: those with suspected rectal cancer will require an MRI pelvis for further staging
Further imaging may be suggested at a multidisciplinary team (MDT) meeting.
Bowel cancer screening
The NHS Bowel Cancer Screening Programme aims to identify bowel cancer at an early stage when treatment is more likely to be successful:16
- In Scotland, screening is offered every two years to people aged 50–74
- In England, Wales, and Northern Ireland, screening is offered every two years to people aged 60–74
- In some areas of England, one-off flexible sigmoidoscopy (Bowelscope) screening is offered to people aged 55
Patients receive an invitation letter and a stool FIT test kit. Results are sent by letter within two weeks of receipt of the completed kit, and the GP is informed of the results electronically. The results of the screening test may then result in a colonoscopy or the need for repeat tests.
Diagnosis
Staging
Colorectal cancer can be staged using the tumour, node and metastasis (TNM) staging system:
- Tumour: degree of intestinal wall invasion
- Nodes: lymph node involvement
- Metastasis: presence of distant metastases
The Dukes staging system was previously used. However, this has been largely replaced by the TNM system.
Management
Following the diagnosis of colorectal cancer, a multidisciplinary team (MDT) composed of colorectal surgeons, radiologists, oncologists, and nurse specialists will review investigation results alongside past medical history to discuss treatment options.
Treatment options for colorectal cancer include:
- Surgery
- Radiotherapy
- Chemotherapy
- Targeted therapy (based on biomarkers/immunotherapy)
Often, patients will have surgery alongside radiotherapy or chemotherapy. The surgery offered depends on the size, location, and metastases.
Surgical management
Surgical intervention for colorectal cancer can be curative or palliative.
In general, patients with rectal cancer receive chemoradiotherapy before surgery (neo-adjuvant), whereas patients with colonic cancer receive chemotherapy after surgery (adjuvant). However, the exact make-up and timing of neo-adjuvant or adjuvant radiotherapy or chemotherapy will be determined at MDT.
Curative
Curative surgical options are numerous, but oncological principles must be followed to ensure a margin-free resection (if curative).
Depending on the MDT outcome, this could be endoscopic resection with techniques such as endoscopic submucosal resection (EMR), trans-anal excision or surgical resection (open, laparoscopic or robotic).
Curative surgical resection involves removing the tumour along with local lymph nodes, with a disease-free margin, whilst ensuring there is adequate blood supply to the remaining bowel.
Depending on the tumour’s location, this will likely involve a segmental resection. The remaining bowel is joined (forming an anastomosis), or a stoma is brought out (ileostomy or colostomy +/- mucus fistula, depending on which part of the bowel is resected).
Palliative
Palliative surgical options include segmental resection (where the aim is not curative) or diversion procedures such as the formation of ileostomy or colostomy. This is usually done for symptomatic relief.
Chemotherapy and radiotherapeutic options are also available for palliative intent.
Complications
Complications of colorectal cancer include:14,15
- Metastasis: the liver is the most common site where colorectal cancer metastases will occur; rectal cancer will most commonly metastasise to the thoracic organs and nervous system
- Bowel obstruction
- Bowel perforation
- Iron deficiency anaemia
- Fistulas
- Complications from treatment (e.g. surgical infection, bleeding etc)
Key points
- Colorectal cancer can be located anywhere from caecum to anus. Most commonly, it is an adenocarcinoma.
- There are multiple risk factors for colorectal cancer.
- Patients presenting with any red flag signs or symptoms require urgent investigation and 2 week wait suspected cancer pathway referral.
- Colonoscopy with biopsy is the gold standard diagnostic test. Bowel cancers are then staged, most commonly using the TNM staging system.
- The NHS runs a national Bowel Cancer Screening Programme to identify early-stage cancers.
- Management under a Multidisciplinary team is tailored to the patient and may include surgery, radiotherapy, chemotherapy, and immunotherapy.
Reviewer
Mr Luke McNickle
ST4 General Surgery
Editor
Dr Chris Jefferies
References
- Cancer Research UK. Types of bowel cancer. Published in 2022. Available from: [LINK]
- Thrumurthy, S. G., Thrumurthy, S. S., Gilbert, C. E., Ross, P., & Haji, A. (2016). Colorectal adenocarcinoma: risks, prevention and diagnosis. BMJ, 354.
- NICE CKS. Gastrointestinal tract (lower) cancers – recognition and referral: Prevalence. Published in August 2023. Available from: [LINK]
- NICE CKS. Gastrointestinal tract (lower) cancers – recognition and referral: Prognosis. Published in August 2023 Available from: [LINK]
- British Society of Gastroenterology. (2020). Guidelines for the management of hereditary colorectal cancer. Available from: [LINK]
- NICE CKS. Bowel screening: People known to be at high risk of bowel cancer. Available from: [LINK]
- Nguyen, L. H., Goel, A., & Chung, D. C. (2020). Pathways of Colorectal Carcinogenesis. Gastroenterology, 158(2), 291-302.
- Malki, A., ElRuz, R. A., Gupta, I., Allouch, A., Vranic, S., & Al Moustafa, A.-E. (2021). Molecular Mechanisms of Colon Cancer Progression and Metastasis: Recent Insights and Advancements. Int. J. Mol. Sci, 22, 130.
- NICE CKS. Gastrointestinal tract (lower) cancers – recognition and referral. Available from: [LINK]
- NICE CKS. Gastrointestinal tract (lower) cancers – recognition and referral: Scenario: Referral for suspected gastrointestinal tract (lower) cancer. Available from: [LINK]
- Cancer Research UK. TNM Staging | Bowel Cancer. Available from: [LINK]
- Bowel Cancer UK. Available from: [LINK]
- NICE. Colorectal cancer: Recommendations. Published in 2020. Available from: [LINK]
- Kow, A. W. C. (2019). Hepatic metastasis from colorectal cancer. J Gastrointest Oncol, 10(6), 1274-1298.
- Riihimäki, M., Hemminki, A., Sundquist, J., & Hemminki, K. (2016). Patterns of metastasis in colon and rectal cancer. Sci Rep, 6, 29765.
- NICE CKS. Bowel screening. Published in 2019. Available from: [LINK]
- NHS. Bowel cancer screening: helping you decide. Available from: [LINK]
- NICE. Quantitative faecal immunochemical testing to guide colorectal cancer pathway referral in primary care: 1 Recommendations. Published in 2023. Available from: [LINK]
Image references
- Figure 1. Emmanuelm. Colorectal cancer, gross appearance of an opened colectomy specimen. License: [CC BY]
- Figure 2. NHS England. NHS bowel cancer screening: helping you decide. License: [OGL]




