- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Crohn’s disease is a chronic, relapsing-remitting, non-infectious inflammatory disease of the gastrointestinal tract.
It is a type of inflammatory bowel disease (IBD), an umbrella term which also includes ulcerative colitis (UC).1
Patients typically present between 20-40 years old, and Crohn’s disease has an incidence of around 10-20/10000/year.2
Aetiology
The aetiology of Crohn’s disease is still unclear. However, it is thought to be an inappropriate immune response to an environmental trigger in a genetically susceptible individual.
Around 15% of affected people have a first-degree relative with the disorder. However, it is important to remember that it is most likely caused by a combination of genetics, environment and lifestyle factors.3
Crohn’s disease can affect a patient anywhere from the mouth to the anus:1
- 80% of patients have evidence of small bowel disease, most commonly occurring in the distal ileum (terminal ileitis)
- 25% of patients suffer from perianal disease
Pathophysiology
Chronic inflammation leads to pathophysiological changes, which can be seen microscopically (on histology) and macroscopically (on endoscopy).
Microscopic features
Histological features include inflammatory infiltration, characterised by lymphoid hyperplasia and non-caseating granulomas. Transmural inflammation is also seen.
Macroscopic features
Initially, small superficial ulcers (aphthous ulcers) form due to inflammation. Over time, they become deep and serpiginous, giving the mucosa its classical cobblestone appearance, which can be seen on endoscopy. There may be bowel wall thickening, fistulae and fissures.
Risk factors
Risk factors for Crohn’s disease include:4
- Family history
- Cigarette smoking
- Previous infectious gastroenteritis
- NSAID usage
- A diet high in refined sugar and low in fibre
Clinical features
History
Typical symptoms of Crohn’s disease include:1,2
- Abdominal pain: most commonly in the right lower quadrant (terminal ileum) and peri-umbilical regions
- Diarrhoea: bloody or non-bloody, may be accompanied by mucus, and nocturnal diarrhoea may occur
- Perianal pain/itching: if perianal disease
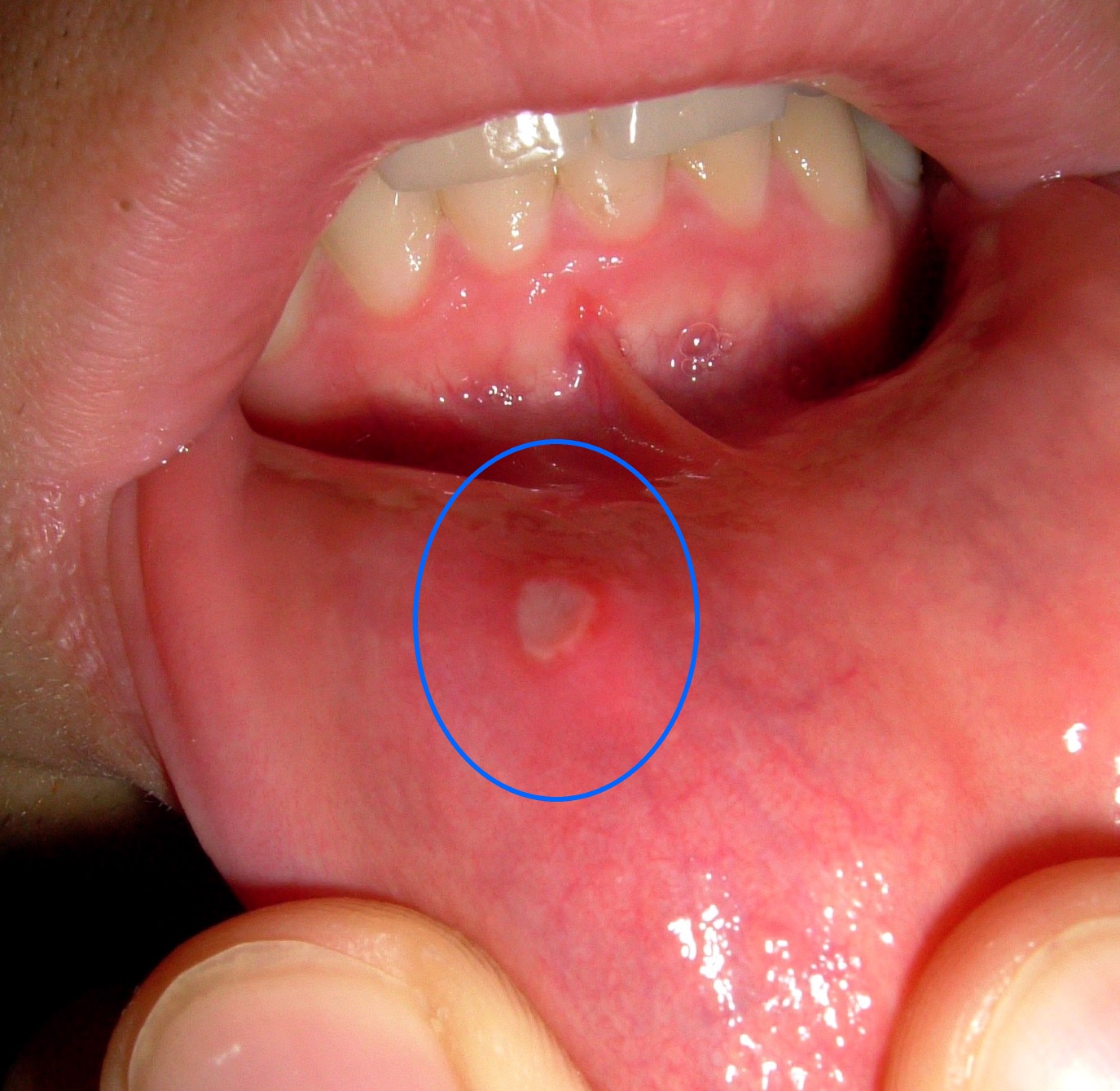
- Oral ulceration (aphthous ulcers) (Figure 1)
- Nausea and vomiting
- Fever
- Fatigue
- Weight loss
Other symptoms may relate to the extra-intestinal manifestations of Crohn’s disease.5
Extra-intestinal manifestations of Crohn’s disease
Extraintestinal manifestations in Crohn’s disease include:
- Musculoskeletal: enteropathic arthritis
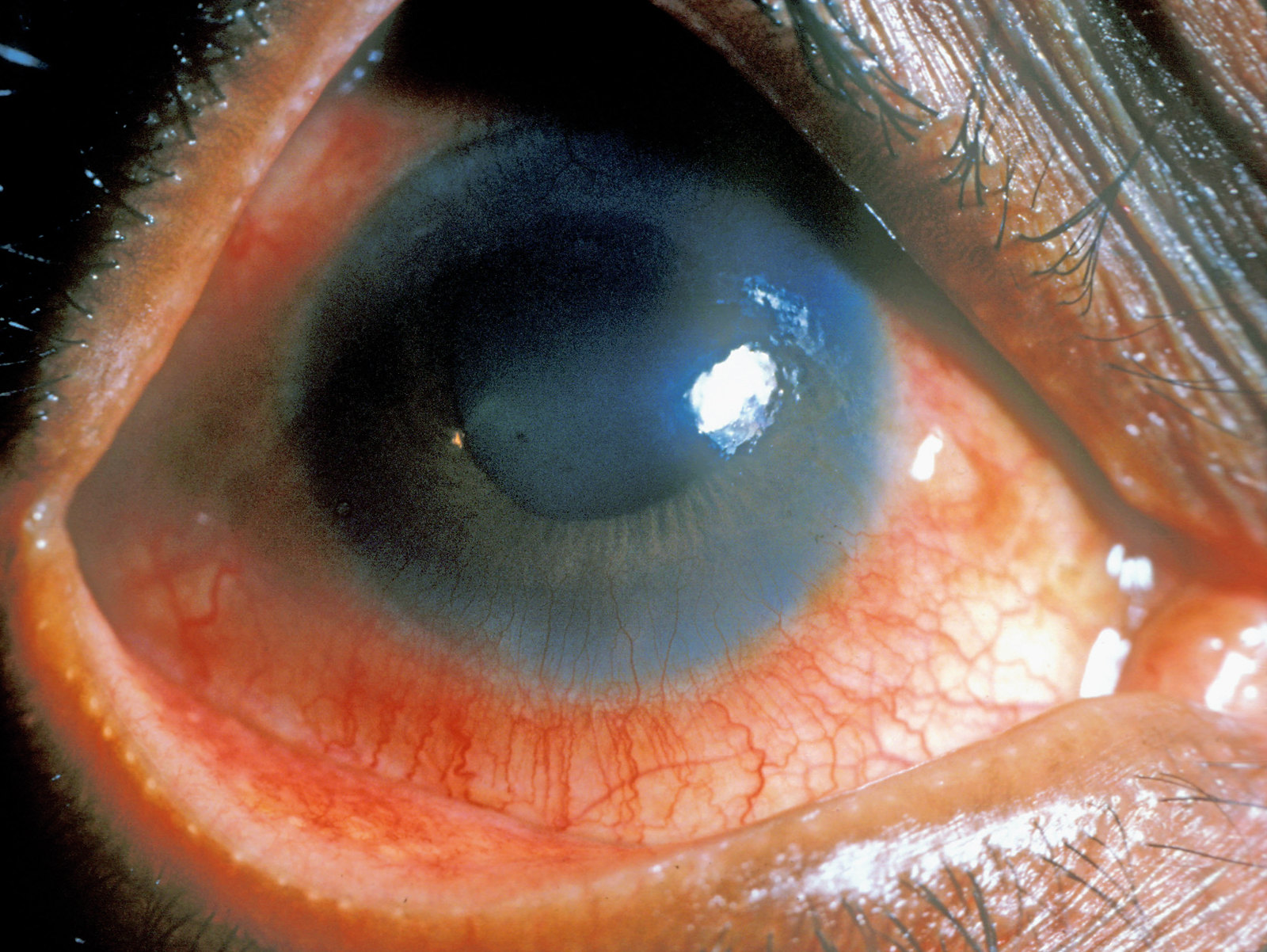
- Eyes: episcleritis, uveitis (Figure 2) and conjunctivitis
- Skin: erythema nodosum (Figure 3) and pyoderma gangrenosum
- Hepatobiliary: primary sclerosing cholangitis, fatty liver disease and gallstones
- Renal: nephrolithiasis
- Haematological: anaemia, B12 deficiency and thromboembolism
Clinical examination
Typical clinical findings on examination include:1
- Abdominal tenderness or mass
- Perianal tenderness or pain, anal or perianal skin tags, fissure, fistula or abscess
- Features of anaemia (e.g. pallor, fatigue and conjunctival pallor)
- Joint pain
- Clubbing
- Oral lesions: aphthous ulcers
Differential diagnoses
Differential diagnoses to consider include:4
- Ulcerative colitis
- Infectious colitis
- Pseudomonas colitis
- Diverticular disease
- Irritable bowel syndrome (this is a diagnosis of exclusion)
- Radiation colitis
Crohn’s disease vs. ulcerative colitis
Table 1. A summary of the key differences between Crohn’s disease and ulcerative colitis.
| Crohn’s disease | Ulcerative colitis | |
| Location | Whole gastrointestinal tract | Colon (mainly rectum) |
| Type of lesion | Transmural inflammation | Superficial ulcers |
| Characteristic pattern | Skip lesions | Continuous lesions |
| Microscopic findings | Non-caseating granulomas | Crypt abscesses |
| Macroscopic findings | Cobblestone appearance | Friable mucosa |
| Complications |
|
|
| Treatment options |
|
|
Investigations
A diagnosis of Crohn’s disease is made based on features of the clinical history and endoscopic findings. However, it is important to exclude any other causes of colitis and diarrhoea first.2
Laboratory investigations
Relevant laboratory investigations include:1
- Full blood count: anaemia, leucocytosis, thrombocytosis
- Liver function tests: hypoalbuminaemia
- Bone profile: hypocalcaemia
- Iron studies: normal or may demonstrate iron deficiency
- Serum B12 / folate: normal or low
- Inflammatory markers (CRP and ESR): elevated
Stool testing
Faecal calprotectin is a sensitive marker of gastrointestinal inflammation and can help distinguish inflammatory bowel disease (IBD) from non-inflammatory gastrointestinal conditions (e.g. irritable bowel syndrome). It is raised in Crohn’s disease and can be used as a marker of disease activity.
Sending a stool microscopy, culture and sensitivity (MC&S) is important to exclude infection (e.g. Clostridium difficile).
Gastrointestinal endoscopy
Colonoscopy and biopsy is the preferred way to diagnose Crohn’s disease. It is used to assess the colon and the terminal ileum.
An upper gastrointestinal endoscopy is used to assess for gastroduodenal disease.
Endoscopic features of Crohn’s disease
Macroscopic features of Crohn’s disease on endoscopy include:
- Cobblestone appearance: small superficial ulcers
- Skip lesions
- Oedema
- Hyperaemia
- Aphthous ulcers
- Rose thorn ulcers: deep penetrating linear ulcers seen around a stenosed terminal ileum.
Microscopic histology features include:
- Transmural involvement with non-caseating granulomas
- Lymphoid hyperplasia
Imaging
Imaging is used in acute presentations (e.g. to identify complications) and to assess the progression of Crohn’s disease.
Relevant imaging investigations include:
- Abdominal X-ray: may identify bowel dilatation and perforation in acute settings
- Abdominal ultrasound: can be used to assess bowel thickening, free-fluid or abscess formation
- CT abdomen: usually used in the acute setting and to assess for complications (especially extra-mural complications)
- MRI small bowel/pelvis: can be used for ‘disease mapping’; assesses the extent of inflammation in the small bowel or fistulae formation
Management
Management of Crohn’s disease aims to induce remission and maintain remission.9
Management plans are usually complex and require the patient to be under the care of a gastroenterologist, with the support of specialist nurses. Treatment plans are dependent on disease severity, co-morbidities and the presence of any complications.
Patients should be advised to stop smoking, which can reduce disease activity and the risk of complications.
Inducing remission
Initial monotherapy for inducing remission may include:
- Corticosteroids (e.g. prednisolone, methylprednisolone or intravenous hydrocortisone): used to induce remission in patients with first presentation or a single inflammatory exacerbation in a 12-month period.
- Budesonide: if conventional steroid use is unsuitable, however, it is less effective.
- Aminosalicylates (e.g. sulfasalazine or mesalazine): these cause fewer side effects than corticosteroids and budesonide but are not as effective; they are unsuitable for severe presentations.
Add-on treatment
The following can be added to a corticosteroid after two or more exacerbations in a 12-month period or if the corticosteroid dose cannot be reduced.
- Thiopurines (e.g. azathioprine or mercaptopurine)
- Methotrexate
- Biologics (e.g. infliximab or adalimumab)
Maintaining remission
Maintenance is tailored to the individual based on side effects, disease severity and patient wishes. This might involve no medications.
First-line agents to maintain remission include:
- Azathioprine
- Mercaptopurine
Methotrexate can be used in patients who required it to induce remission.
Surgical management
Indications for surgical management of Crohn’s disease include:10
- Patient choice: patients with ileocaecal disease may be offered medicines or surgery
- Failure of medical management: medications do not improve disease activity or are not suitable
- Development of implications: strictures, abscesses, fistulas, obstruction or perforation
Common surgical management options for Crohn’s disease include:10
- Strictureplasty: widens narrowed areas of the bowel that could lead to obstruction
- Fistula removal: closes, opens, drains or removes a fistula that doesn’t heal with medications
- Abscess drainage
- Colectomy: removes diseased colon, sparing the rectum
- Proctocolectomy: removes diseased colon and rectum
- Ileostomy/colostomy
- Bowel resection: removal of the diseased small or large bowel and connection of the two healthy ends

Complications
Complications of Crohn’s disease include:11
- Psychosocial impact (e.g. on school, work or leisure)
- Intestinal complications: strictures, fistulas, dilatation, perforation and haemorrhage
- Perianal disease
- Anaemia
- Malnutrition, faltering growth or delayed pubertal development
- Cancer of the small and large intestine
Key points
- Crohn’s disease is a form of inflammatory bowel disease that can affect the entire gastrointestinal tract, from mouth to anus.
- Some common risk factors include cigarette smoking and NSAID usage.
- The most common symptoms include abdominal pain, diarrhoea and weight loss; these may be accompanied by systemic features such as fever and fatigue.
- Initial investigations include blood tests (e.g. FBC, iron studies, serum B12 and folate), stool samples (e.g. faecal calprotectin) and imaging.
- A diagnosis is usually confirmed after a colonoscopy and biopsies.
- Key features on endoscopy and histology include a cobblestone appearance, skip lesions, transmural inflammation and lymphoid hyperplasia.
- Management aims to induce and maintain remission. This is usually done via medical management (e.g. corticosteroids, aminosalicylates, thiopurines or biologics); some patients may also require surgery and additional non-medical treatments such as enteral nutrition.
- Complications include perianal disease, bowel obstruction, malnutrition and cancer.
Reviewer
Dr Sarah Hyde
Gastroenterology registrar
Editor
Dr Chris Jefferies
References
- BMJ Best Practice. Crohn’s disease. Published in 2023. Available from: [LINK]
- Ian Wilkinson. Handbook of Clinical Medicine: Crohn’s Disease. Published in 2017. Available from: [LINK]
- Crohn’s & Colitis Foundation. Causes of Crohn’s Disease. Published in 2023. Available from: [LINK]
- NICE. Crohn’s disease. Published in 2020. Available from: [LINK]
- NICE. Crohn’s disease: What are the extra-intestinal manifestations of Crohn’s disease?. Published in 2020. Available from: [LINK]
- Maksim. Aphthous Ulcer. License: [CC BY-SA]
- Community Eye Health. Acute anterior uveitis. License: [CC BY-NC]
- Medicalpal. Erythema nodosum. License: [CC BY-SA]
- NICE. Crohn’s disease: management. Published in 2019. Available from: [LINK]
- WebMD. Surgery for Crohn’s Disease. Published in 2023. Available from [LINK]
- NICE. What are the complications? Published in 2020. Available from: [LINK]