- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Idiopathic intracranial hypertension (IIH), also known as benign intracranial hypertension or pseudotumour cerebri, is defined as raised intracranial pressure in the absence of intracranial mass or hydrocephalus (an abnormal increase in CSF volume). This causes headaches and significant visual disturbances.
IIH is a rare condition that affects up to two in 100,000 people, mainly affecting obese women of childbearing age.1 In the UK, the incidence is approximately 4.7 per 100,000 people, and its growth parallels obesity.2
Aetiology
The underlying cause of IIH remains unknown. IIH in adults is highly associated with female sex and obesity.3
Pathophysiology
Cerebrospinal fluid (CSF) is a clear fluid in the subarachnoid spaces and ventricles that cushions the central nervous system against the surrounding bones. It is secreted by the choroid plexus in the lateral, third, and fourth ventricles. CSF absorption mainly occurs via the arachnoid granulations when pressure exceeds the venous pressure in the sinus.
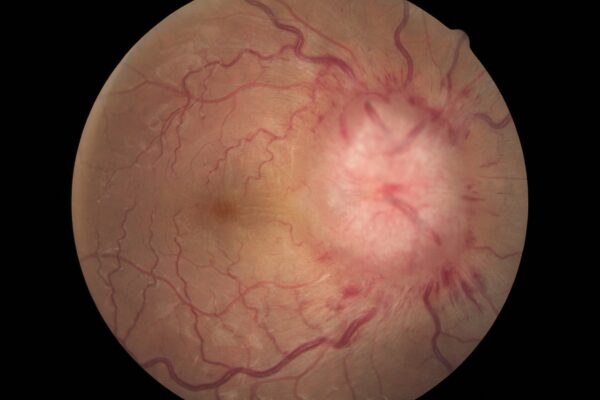
The intracranial subarachnoid space extends from the optic nerve to the back of the eyes. Increased CSF pressure compresses the thin walls of retinal veins as they cross extensions of subarachnoid spaces to enter the optic nerve.
This causes congestion of retinal veins, bulging forward of optic discs and oedema of the discs, known as papilloedema. Persistent papilloedema can lead to optic atrophy and irreversible blindness.
Several mechanisms have been proposed to explain the increased intracranial pressure in IIH, but the pathophysiology remains unclear:4,6
- Overproduction of CSF
- Outflow obstruction
- Raised pressure in venous sinuses
- Dysfunction in the glymphatic pathway
- Hormonal alteration
Risk factors
IIH may happen to any age group or sex, but it more commonly affects people with the following risk factors:4-6
- Obesity (often associated with recent weight gain)
- Female sex
- Medications including combined contraceptive pills, tetracyclines, vitamin A, retinoids, lithium, thyroxine, nitrofurantoin
Clinical features
History
Symptoms of IIH are usually chronic and progressive and include:2,4-6
- Headache: the most common clinical presentation of IIH. Usually non-specific and diffuse, and sometimes associated with nausea/ vomiting and retrobulbar pain.
- A pressure-like sensation behind the eyes, typically worsens on bending forward or Valsalva manoeuvres.
- Transient visual loss/blurring of vision: usually lasts <30 seconds, followed by full vision restoration to baseline.
- Pulsatile tinnitus: a pulse-synchronous sound classically described as a unilateral “whooshing” sound exacerbated by lying flat.
- Visual disturbance: commonly affecting the peripheral visual field, photopsia, and photophobia, flashes & visual obscuration.
- Ocular motility disturbance: horizontal diplopia is reported by one-third of IIH patients, and 10-20% of them are related to cranial nerve sixth palsy (as a false localising sign)
Clinical examination
All patients with suspected IIH should undergo a comprehensive neurological examination, which includes cranial nerves examination (particularly second, third, fourth and sixth cranial nerves), upper limb and lower limb examination to exclude other causes of raised intracranial pressure.
A full ophthalmic examination should include visual acuity, colour vision, pupils, visual field assessment and fundoscopy.
Common clinical findings in IIH include:4-7
- Papilloedema, typically bilateral and symmetrical, is the hallmark sign of IIH; the severity of papilloedema can be graded using the Modified Frisén Scale
- Enlargement of blind spot
- Peripheral visual field defects can involve central visual field defects in the advanced stage, or in concurrent macular disease
- Horizontal diplopia can occur among patients with non-localising neurological sixth cranial nerve palsy
- Otherwise, a normal neurological examination
Differential diagnoses
IIH is usually a diagnosis of exclusion. Therefore, in the assessment of a patient with raised intracranial pressure, secondary causes of intracranial hypertension should be considered:4-6
- Intracranial mass lesions (e.g. space-occupying lesions, tumours, abscesses)
- Increased CSF production (e.g. choroid plexus papilloma)
- Reduced CSF absorption (e.g. arachnoid granulation adhesions post-meningitis, subarachnoid haemorrhage)
- Obstruction of venous outflow (e.g. venous sinus thrombosis, jugular vein compression, neck surgery)
- Malignant hypertension
- Obstructive sleep apnoea
Investigations
Relevant investigations include:4-7
- MRI/CT: to exclude secondary causes of raised intracranial pressure
- Lumbar puncture: to assess CSF opening pressure taken with the patient lying in a lateral decubitus position. The diagnosis is based on an elevated opening pressure greater than 250 mmH2O and a normal CSF constituent.
Other investigations to exclude other secondary causes of raised intracranial pressure include:
- Blood pressure: to exclude malignant hypertension, which is defined as systolic blood pressure >= 180mmHg or diastolic blood pressure >= 120mmHg
- Magnetic resonance venogram of head: to rule out venous thrombosis
- Perimetry: to assess visual fields
- Ocular coherent tomography (OCT): to measure the thickness of the retinal nerve fibre layer and quantify the progress of papilloedema
Diagnosis
The diagnosis of IIH can be made using the modified Dandy Criteria:4
- Signs and symptoms of raised intracranial pressure
- Absence of localising findings of neurological examination (except for sixth cranial nerve palsies)
- Normal cerebrospinal fluid composition
- Absence of deformity, displacement or obstruction of the ventricular system and otherwise normal neuroimaging studies
- No other cause of increased intracranial pressure present
Management
The management of IIH focuses on treating underlying disease, preserving vision, and reducing headache morbidity.7
Conservative management
Weight loss is disease-modifying and reduces intracranial pressure and papilloedema in IIH patients.
Any causal factor that causes raised intracranial pressure should be eliminated or treated appropriately. For example, medications which increase the risk of IIH, as listed above, should be discontinued.
Medical management
Pharmacotherapy is usually considered for patients with mild to moderate symptoms. Acetazolamide, a carbonic anhydrase inhibitor, is believed to reduce the rate of CSF production and is the first-line medical management for IIH.4,7
If acetazolamide is inefficient or not tolerated by the patient, other options include:
- Topiramate acts as a weak carbonic anhydrase inhibitor and can suppress appetite, causing weight loss. However, women patients should be counselled regarding the side effects, including cognitive suppression, depression, and teratogenetic risks.1,4,7
- Furosemide, a loop diuretic, appears to work by producing diuresis and reducing sodium transport in the brain, thereby reducing CSF secretion. It can be given as an adjunct alongside acetazolamide in refractory cases.4,5,6
Therapeutic serial lumbar punctures may have a role as a temporising measure to preserve vision in patients with fulminant IIH awaiting an imminent surgical procedure. However, they are not used as a long-term treatment strategy for IIH due to short-lived effects and negative experiences reported by patients.7,8
Surgical management
Surgical management is essential for IIH patients with rapidly declining visual function or those who failed medical therapy to prevent permanent loss of vision. Surgical options include:8
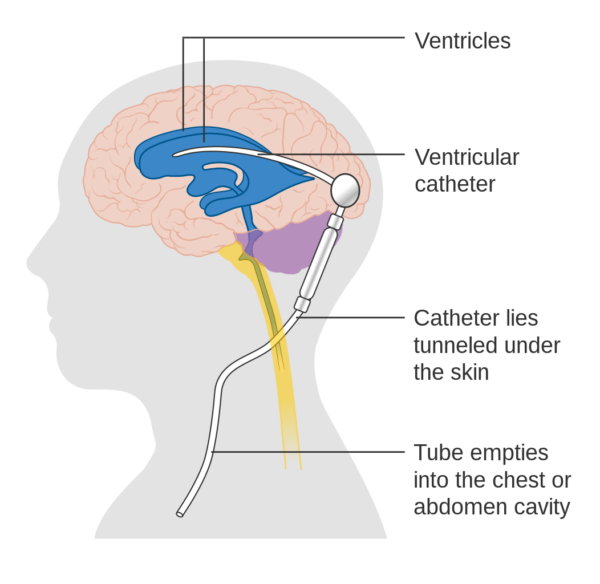
- CSF diversion procedures (ventriculoperitoneal is usually preferred over lumbo-peritoneal, and is the preferred surgical procedure in the UK)
- Optic nerve sheath fenestration (ONSF)
Complications
Permanent visual loss is the main complication, especially in advanced disease presentation. Symptomatic patients with extensive visual field loss and severe papilloedema should be referred for urgent surgical management.
Key points
- Idiopathic intracranial hypertension is a disorder characterised by increased intracranial pressure of unknown cause that predominantly affects overweight women of childbearing age.
- Being overweight and female gender appears to be the main risk factors for IIH.
- Headache and visual alteration are the main symptoms of IIH, while papilloedema and peripheral visual field defects are the primary findings from physical examination.
- Patients with suspected IIH should be urgently referred for neuroimaging to exclude secondary causes of intracranial hypertension.
- Lumbar puncture is mandatory in diagnosing IIH with an opening pressure exceeding 250mmH2O measured in the lateral decubitus position, and normal CSF composition.
- Weight loss reduces intracranial pressure and has shown to be effective in improving papilloedema and headaches.
- Acetazolamide can be prescribed to reduce CSF production in patients with mild to moderate symptoms.
- Irreversible visual loss due to severe papilloedema is the major morbidity in advanced presentations of IIH.
- To preserve vision, acute surgical management (CSF shunt) should be offered to patients with declining visual function.
Reviewer
Dr Mounika Yelisetti
ST3 Neurology
Editor
Dr Chris Jefferies
Reference
- Raoof N, Hoffmann J. Diagnosis and treatment of idiopathic intracranial hypertension. Published Feb 2021. Available from: [LINK]
- Wakerley BR, Mollan SP, Sinclair AJ. Idiopathic intracranial hypertension: Update on diagnosis and management. Published July 2020. Available from: [LINK]
- Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri: population studies in Iowa and Louisiana. Published Aug 1988. Available from: [LINK]
- BMJ Best Practice. Idiopathic intracranial hypertension. [LINK]
- EyeWiki. Pseudotumor cerebri (idiopathic intracranial hypertension). [LINK]
- Wall M. Idiopathic intracranial hypertension. Published Aug 2010. Available from: [LINK]
- European Headache Federation. Guideline on idiopathic intracranial hypertension. Published Oct 2018. Available from: [LINK]
- J Neurol Neurosurg Psychiatry. Idiopathic intracranial hypertension: consensus guidelines on management. Published Jun 2018. Available from: [LINK]
Image references
- Figure 1. DocSee04. Human Right Eye Retina Photo with severe Papilledema. License: [CC BY]
- Figure 2. Cancer Research UK. Diagram showing a brain shunt. License: [CC BY-SA]




