- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A 34-year-old man is referred to the medical assessment unit with a cough, chest pain and a fever. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
- Breathlessness
- Chest pain
- Cough
- Fever
History
Presenting complaint
“My chest really hurts. I’ve had this horrible cough and feel really feverish”
History of presenting complaint
Chest pain
Where is the pain?
“It feels like it’s at the bottom of my ribs on the left”
When did the chest pain start?
“It started about 2 weeks ago, I thought it was because I’ve been coughing so much but it also hurts when I breathe in“
Can you describe the pain?
“It’s quite a sharp pain when I cough or breathe in deeply“
Does the pain spread anywhere else?
“No“
Has the pain worsened?
“I think so, it didn’t use to hurt when I breathed in but now it does“
Does anything make it better?
“Not really, but I try to take shallow breaths to avoid it“
Does anything make it worse?
“Breathing deeply or coughing“
How would you rate the pain on a scale of 0 – 10?
“It’s probably around a 7/10“
Cough
When did the cough start?
“The cough started about 3 weeks ago while I was in India visiting family, since I got it last week it’s been getting worse”
Is the cough constant or does it come and go?
“It’s pretty constant but has been getting worse at night when I go to bed”
Is there anything that triggers the cough or anything that makes the cough better?
“The cough is always there but it gets worse when I lie down and gets slightly better when I’m upright”
Do you bring up any sputum when you cough or is it dry/tickly?
“At first I wasn’t bringing anything up but over the last week I’ve been bringing more and more mucus”
What colour is the mucus you’re bringing up?
“It started clear but now it’s green”
Have you ever coughed up any blood?
“Maybe? Yesterday the mucus was dark red, but that only happened once”
For more information, see the Geeky Medics guide to cough history taking.
Shortness of breath
When did you start getting short of breath?
“Since the cough started, I’ve been getting short of breath but over the last week it’s gotten worse”
Is there anything that makes the shortness of breath worse?
“When I lie down it gets really bad, I’ve had to start using more pillows to go to bed”
Other symptoms
Have you had a wheeze?
“No”
Have you had any tiredness?
“Yes absolutely, I’m not sleeping as well and I’ve started having really feverish sleep”
Have you had a fever or night sweats?
“Both, I feel like I go hot and cold a lot, and recently I’ve been waking up drenched in sweat”
Have you had any weight loss?
“I think I’m looking thinner which is quite worrying because I’ve only been feeling ill for a few weeks!”
Have you had any change in taste or smell?
“No”
Have you had contact with anyone else with similar symptoms?
“Not that I know of, but I met a lot of family in India who I don’t know very well”
Have you had any recent foreign travel?
“Yes, I was in India visiting family a few weeks ago, and I was there for 2 weeks”
For more information, see the Geeky Medics guide to respiratory history taking.
Other parts of the history
Past medical and surgical history
- Do you have any medical problems?
“I was diagnosed with HIV 3 years ago, but nothing else”
Medication history/allergies
- Do you take any regular medication?
- Do you have any allergies?
“I’m on antiretrovirals for HIV but forgot to take them while I was in India. I don’t have any allergies”
Family history
- Do any medical problems run in the family?
“Not that I know of”
Social history
- Do you live with anyone?
- Do you work currently?
- Are you up to date with vaccinations?
- Have you been vaccinated for tuberculosis (TB)?
- Do you smoke?
- Do you drink alcohol?
- Do you use recreational drugs?
“I live alone and work in IT. I think I’m up to date with my normal vaccinations but I’m not sure about TB, I don’t think I’ve had a vaccine for that. I don’t drink or smoke and I’ve never taken drugs”
Clinical examination
Examination findings
Inspection
- No scar
- No chest wall deformity
Palpation
- Trachea central
- Mildly reduced expansion on the left side
Auscultation
- Crackles on the left side
- Reduced air entry on the lower left side
- Decreased vocal fremitus on lower left side
Percussion
- Stony dull percussion on the lower left side
Investigations
This patient is presenting with pleuritic chest pain and shortness of breath, making a chest X-ray the most appropriate initial investigation.
- Full blood count: for infection markers
- Urea and electrolytes: renal function, electrolyte abnormalities
- CRP: infection marker
- Liver function tests and coagulation
- CD4 count: HIV activity (considering the patient had a pause in his anti-retroviral medication)
- Hepatitis serology
- Arterial blood gas: to assess oxygenation
- D-dimer: to help rule out pulmonary embolism
Chest X-ray
The patient’s chest X-Ray is shown below.
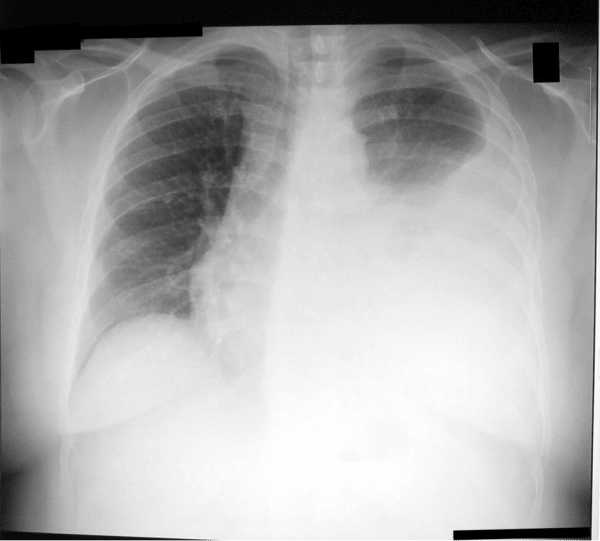
Dense opacity pleural effusion in the left lung.
Diagnosis
Pleural fluid aspiration should be performed and analysed with the following:
- Appearance: purulent (infection), bloody (malignancy, PE, trauma)
- Biochemistry: protein, LDH, glucose
- Microbiology: Gram stain, culture
- Cytology
Light’s criteria distinguishes between exudative and transudative pleural effusions. The fluid is exudate if one or more of the following criteria are met:
- Pleural fluid protein divided by serum protein is >0.5
- Pleural fluid LDH divided by serum LDH is >0.6
- Pleural fluid LDH is >⅔ the upper limit of the laboratory normal value for serum LDH
Management
- Smaller pleural effusions: observation
- Larger pleural effusions: aspiration or chest drain insertion
- Heart failure: diuretics
- Infection: antibiotics
Diagnosis
After further investigations, the patient is diagnosed with tuberculosis.
Rifampicin, isoniazid, pyrazinamide, and ethambutol are the antibiotics used to treat tuberculosis.
Complications
Ethambutol
Isoniazid
Editor
Dr Jess Speller
References
- Clinical Cases. Left-sided pleural effusion. License: [CC-BY-SA].
- S. Crane and C. Wearmouth for RCEM Learning. Pleural Effusion. Published in 2011. Available from: [LINK].
- R. Light et al. Pleural Effusions: The Diagnostic Separation of Transudates and Exudates. Published in 1972. Available from: [LINK].
- Patient Info. Tuberculosis. Published in 2019. Available from [LINK].
- NICE. Tuberculosis. Published in 2016. Available from [LINK].