- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A 54-year-old woman attends the emergency department with a headache and vomiting. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
- Headache
- Vomiting
History
Presenting complaint
“I’ve got the most awful headache and feel really sick”
History of presenting complaint
Where is the pain?
“At the back of my head”
When did it start and what were you doing when it started? Have you hit your head at all recently?
“It came on suddenly around 2 hours ago while I was just sat at my desk. It felt like someone had hit me round the back of the head, but I haven’t hit my head at all”
Can you describe the pain?
“Awful, intense ache”
Does the pain go anywhere else?
“I can feel it going down into my neck”
Have you noticed any weakness?
“No”
Have you had any changes to sensation in your body? Or any new, abnormal sensations?
“No”
Have you had any loss of vision?
“No”
Did you lose consciousness at all?
“No”
Have you been sick with the headache?
”I’ve been sick 3 times since it started.”
Do bright lights make the pain worse?
“Yes, the bright lights in here are bothering me”
Do you have any neck pain?
“Yes, it feels really sore”
Have you had a fever? Or felt chills?
“No”
How long did it take to reach maximum intensity?
“It got as bad as it is now within around 30 seconds.”
Have you had similar headaches previously?
“I’ve never had anything like this before in my life”
Have you had any analgesia?
“I’ve had paracetamol but that hasn’t helped.”
Does the headache change with position?
“Nothing really makes any difference to it”
What would you score the pain out of 10?
“Definitely a 10/10”
Note that this history is focused on an acute headache. In chronic or recurrent headaches, other factors are important to consider, such as frequency and triggers for the headaches.
Headache red flags
For more information on red flags, see the Geeky Medics guide to headache history taking.
| Red flag | Status |
| Symptoms of raised intracranial pressure | Present |
| Focal neurological symptoms such as limb weakness or sensory change, visual loss, or speech deficit | Absent |
| A sudden-onset severe headache | Present |
| History of head trauma | Absent |
| Symptoms of meningeal irritation | Present |
| Fever and/or petechial rash | Absent |
| Acute severe eye pain or monocular visual loss/redness | Absent |
| Temporal artery tenderness | Absent |
Clinical examination
- Cranial nerve examination
- Upper and lower limb neurological examination
- Assess the Glasgow Coma Score (GCS)
- Fundoscopy
- Given the patient’s vomiting, you may also wish to examine the gastrointestinal system
Examination findings
- Cranial nerve examination normal
- Upper and lower limb neurological examinations normal
- GCS 15/15 (E4V5M6)
- Fundoscopy normal
- Abdominal examination normal
Assess for signs of meningism:
- Nuchal rigidity (neck stiffness and restricted movement, not just painful movement): present
- Kernig’s sign (resisted extension of the knee when knee and thigh held at 90 degrees): absent
- Brudzinski’s sign (flexion of the neck causing flexion of the hips whilst laying supine): present
Investigations
A plain CT head is the most important test to arrange in the emergency department.
If the initial CT is normal and doesn’t show any contraindications, a lumbar puncture should be considered to obtain CSF for microscopy, culture, and sensitivity (MC+S), protein, glucose, and xanthochromia testing.
Diagnosis
Some of the most likely possible diagnoses are listed below using the VINDICATE model:
- Vascular: subarachnoid haemorrhage, intracerebral haemorrhage
- Infective: CNS infection including viral or bacterial meningitis, encephalitis, abscess
- Neoplastic: CNS tumour (primary or metastatic)
- Degenerative
- Idiopathic: acute angle-closure glaucoma, primary headache disorder (e.g. migraine, cluster headache)
- Congenital: obstructive hydrocephalus
- Autoimmune: vasculitis
- Traumatic: traumatic brain injury
- Endocrine: hypertensive crisis
CT head
Here is an image from the CT head of this patient:
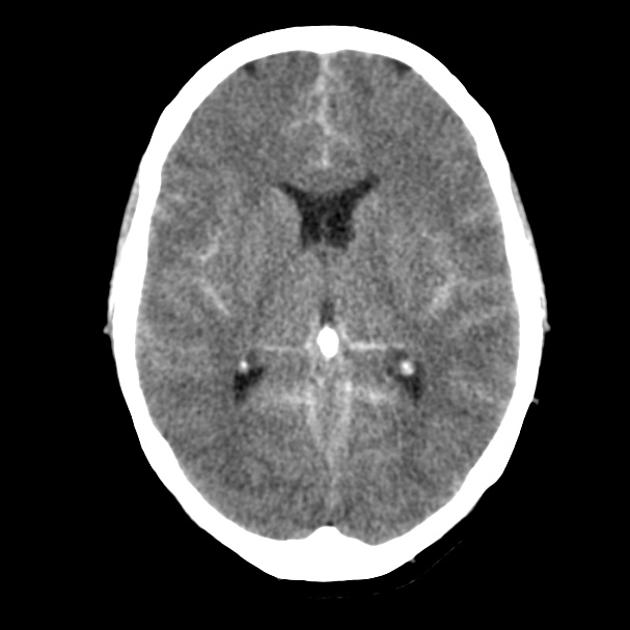
Subarachnoid haemorrhage (SAH) is the most likely diagnosis in this patient presenting with a thunderclap headache and vomiting, and hyperdense material in the subarachnoid spaces in keeping with acute blood is seen on the CT head.
While trauma is the most common cause of subarachnoid haemorrhage (SAH), aneurysm rupture is the most common cause of atraumatic SAH. Less common causes include vasculitis and bleeding from arteriovenous malformations.
Management
Nimodipine is a calcium channel blocker that, unlike amlodipine, has shown benefit in reducing the risk of vasospasm in subarachnoid haemorrhage. A standard regime is 60mg every 4 hours for 21 days.
Aspirin is sometimes used in patients following endovascular treatment of aneurysms but should not be given to patients with bleeding before this.
Depending on the type, location and size of the aneurysm, options include interventional neuroradiological procedures such as coiling and surgical procedures such as clipping of the aneurysm.
Other surgical procedures may be required, such as inserting an external ventricular drain (EVD) to manage hydrocephalus.
Complications
- Hydrocephalus
- Vasospasm
- Hyponatraemia
- Re-bleeding
- Seizures
- Neurological deficit
Editor
Dr Jess Speller
References
- Radiopaedia.org, Cuete, D. Subarachnoid haemorrhage. Case study image. Published May 2013. Available from: [LINK]
- BMJ. Effect of oral nimodipine on cerebral infarction and outcome after subarachnoid haemorrhage: British aneurysm nimodipine trial. 1989 Mar 11; 298(6674): 636–642.
- Kopitnik, T.; Samson, D. Management of subarachnoid emergency. Journal of Neurology, Neurosurgery, and Psychiatry. 1993. 56: 947-959. Available from: [LINK]
- British Association for the Study of Headache. BASH Guidelines 2019. Available from: [LINK]




