- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
This article provides an overview of the common paramedic drugs, as detailed in the Joint Royal Colleges Ambulance Liaison Committee (JRCALC) guidelines.1 Additional information has been included from a variety of sources, including the British National Formulary.2
Each ambulance trust or organisation will have local variations to the medications carried or guidance for administration. Additional paramedic drugs or specific patient group directives (PGDs) may be available. Additional drugs or preparations may be available for advanced paramedics.
This article does not replace the need to consult JRCALC or local policy before administration. It is not intended to present a complete list of contraindications or cautions. Additional caution should be taken when dealing with patients at higher risk of complications, such as children, the elderly and those with renal or hepatic disease.
Safe drug administration
Before administering a drug, it is best practice to check and cross-check (with another person) the following:
- Right patient
- Right drug
- Right route
- Right dose
- Right time
- Indications
- Contraindications and cautions
Activated charcoal
Activated charcoal is given to treat oral poisoning or oral drug overdose.
It is a form of charcoal that has been treated to make it more porous. When ingested, it remains in the gastrointestinal tract, allowing it to adsorb the ingested toxin and prevent it from being absorbed into the body.3
Where an overdose or poisoning has been intentional, the patient may decline to take the activated charcoal. However, this should not be assumed, and activated charcoal should be offered to all patients following an oral drug overdose.
Administration
- Oral (suspension)
- Must be administered within one hour of ingestion unless advised otherwise by Toxbase or the National Poisons Information Service
- It can be mixed with soft drinks to aid consumption
Key considerations
- Not effective with some substances, such as metal salts and ethanol
Adrenaline
Adrenaline 1:1,000
This concentration of adrenaline (1mg/ml) is given to treat anaphylaxis or life-threatening asthma.
Adrenaline stimulates alpha and beta adrenoreceptors which increases heart rate and contractility, causes vasoconstriction, relieves bronchospasm and suppresses histamine.4 This is useful in anaphylaxis to reduce swelling in the airways and raise blood pressure. In life-threatening asthma, it is given for its bronchodilatory effects.
Anaphylaxis
Anaphylaxis is a severe allergic reaction characterised by:
- Sudden onset and rapid progression of symptoms (most reactions occur over several minutes)
- Life-threatening airway and/or breathing and/or circulation problems
- Skin and/or mucosal changes (flushing, urticaria, angioedema): although these can be subtle or absent in up to 20% of reactions
Administration
Key considerations
- Beware of severe hypertension in patients on non-cardioselective beta-blockers (e.g. propranolol)
- Not to be confused with adrenaline 1:10,000, used in cardiac arrest
Adrenaline 1:10,000
This concentration of adrenaline (1mg/10ml) is given in cardiac arrest or for patients who are hypotensive after return of spontaneous circulation (ROSC).
Adrenaline stimulates both alpha and beta adrenoreceptors, which causes vasoconstriction. This increases peripheral resistance, enhancing myocardial and cerebral blood flow. This increases the chance of achieving ROSC and helps to maintain blood pressure.
Administration
- Intravenous or intraosseous
- Cardiac arrest non-shockable rhythm: administer the first dose once IV/IO access is achieved
- Cardiac arrest shockable rhythm: administer the first dose after three shocks
Key considerations
- Not to be confused with adrenaline 1:1,000, used in anaphylaxis and asthma
For more information, see the Geeky Medics guide to pre-hospital advanced life support (ALS).
Amiodarone hydrochloride
Amiodarone is given in cardiac arrest, where the patient is in a shockable rhythm.
Amiodarone is an antiarrhythmic, lengthening cardiac action potential and prolonging the QT interval. It blocks sodium and potassium channels and reduces electrical irritability of the cardiac muscle. This may help restore the heart to a normal rhythm.
Administration
- Intravenous or intraosseous
- Administer after the third and fifth shocks
Key considerations
- Not administered if the patient is in a non-shockable rhythm (e.g. asystole)
Aspirin
Aspirin is given to treat suspected myocardial infarction or ischaemia. It is also administered for suspected transient ischaemic attack (TIA) where symptoms have fully resolved.
Aspirin is an antiplatelet that prevents thromboxane formation, therefore reducing platelet aggregation. In a myocardial infarction, this can reduce the size of a developing blood clot and enhance clot breakdown to decrease damage to the heart.5
Aspirin is given after a TIA as the majority are caused by blood clots, and it has been proven to reduce the risk of further strokes.6
Administration
- Oral (tablet)
- A 300mg dose should be given even if the patient has already taken a smaller prescribed dose (e.g. 75mg) that day
Key considerations
- Not given to children under 16 as it may precipitate Reye’s syndrome, which can be fatal
- Not given to those with clotting disorders or active gastrointestinal bleeding
Atropine sulphate
Atropine is given to treat symptomatic bradycardia with a heart rate below 40, hypotension, arrhythmias, inadequate perfusion or bradycardia following the return of spontaneous circulation (ROSC).
Atropine is an antimuscarinic that inhibits acetylcholine receptors and blocks vagal activity. This suppression of the parasympathetic nervous system allows the sympathetic nervous system to predominate, raising the heart rate.7
A higher dose of atropine is also administered as an antidote for nerve agent poisoning (follow specific guidance for these specialist situations).
Administration
- Intravenous or intraosseous
Key considerations
- Not given in hypothermia
- Not given to patients who have received a heart transplant
- Only given in myocardial infarction if bradycardia is causing perfusion problems due to the risk of tachycardia increasing myocardial oxygen demand
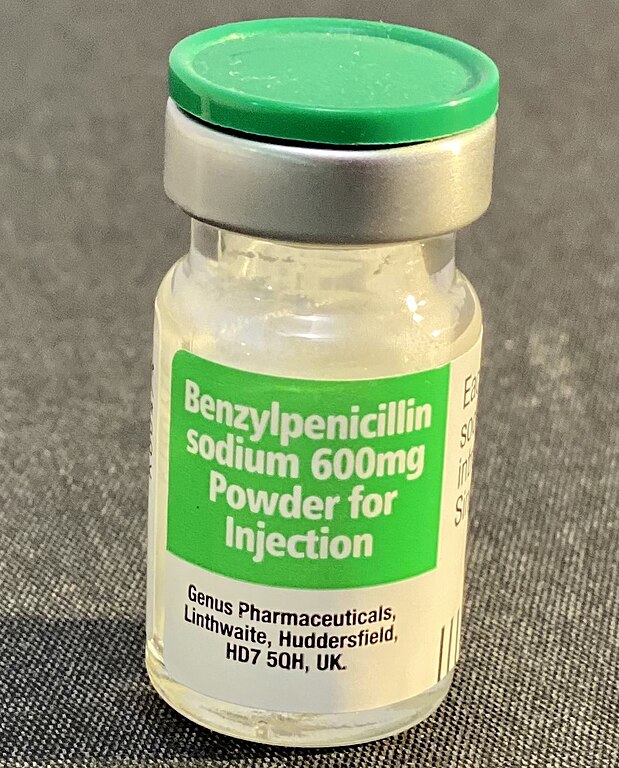
Benzylpenicillin sodium
Benzylpenicillin is given to treat suspected meningococcal disease (meningitis), where there is either a non-blanching rash or signs of meningococcal septicaemia.
Benzylpenicillin is a narrow-spectrum antibiotic. It interferes with bacterial cell wall synthesis and can penetrate the cerebrospinal fluid when the meninges are inflamed.
Administration
- Intravenous, intraosseous or intramuscular
- It comes in powder form and must be dissolved in water for injection (Figure 1)
Key considerations
- Penicillin allergy is commonly reported; however, few people are truly allergic.8 Administration is only contraindicated if the reaction is likely to be severe
Chlorphenamine
Chlorphenamine is given to treat symptoms of allergic reactions if causing the patient distress.
Chlorphenamine is an antihistamine that blocks the effects of the chemical histamine released due to a hypersensitivity reaction. It reduces the adverse effects of histamine, such as localised inflammation, urticaria and excessive mucus.
Administration
- Intravenous, intramuscular or oral
- It has a sedative effect, and patients should not drive following administration
Key considerations
- Only given in anaphylaxis after the administration of adrenaline and if the patient is stable
Dexamethasone
Dexamethasone is given to treat croup, a common upper respiratory condition in children, typically between 6 months and 3 years.9
Croup causes inflammation in the upper airways. Dexamethasone is a corticosteroid which decreases vasodilation and capillary permeability whilst inhibiting the accumulation of inflammatory cells. It has been shown to reduce symptoms of croup within two hours and shorten hospital stays.10
Administration
- Oral
- Tablets should be mixed thoroughly with water, milk or juice
Key considerations
- Causing distress when administering the medication should be avoided due to the risk of airway compromise
Diazepam
Diazepam is used for seizures where the convulsions are prolonged, repeated or suspected to be eclamptic. It is also used to treat symptomatic cocaine toxicity.
Diazepam is a benzodiazepine that facilitates gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter which prevents seizure-causing activity in the central nervous system.11 It has broad anticonvulsant, anxiolytic, sedative, muscle relaxant, and amnesic properties which can reverse the effects of cocaine.
Administration
- Intravenous, intraosseous or rectal
- A half dose should be administered to frail patients
- Rectal administration should only be used if rapid intravenous access is not achievable
Key considerations
- Use with caution where there has been use of alcohol, opioids or other central nervous system depressants due to the risk of respiratory depression
- Caution should be taken with extrication due to the risk of significant hypotension
Furosemide
Furosemide is given to treat pulmonary oedema and/or respiratory distress in acute heart failure.
Furosemide is a diuretic that inhibits the reabsorption of sodium and chloride in the kidneys resulting in more water being excreted. This helps reduce fluid build-up in the lungs due to heart failure, reducing any subsequent respiratory distress.
It has an effect within 30 minutes and may cause the patient to need to pass urine more urgently, so the practicalities of this may need to be considered.
Administration
- Intravenous
- Administer slowly over 2 minutes
Key considerations
- Not given to patients in cardiogenic shock
- Not given to children
- Furosemide can cause potassium to be excreted leading to hypokalaemia which may cause cardiac arrhythmias
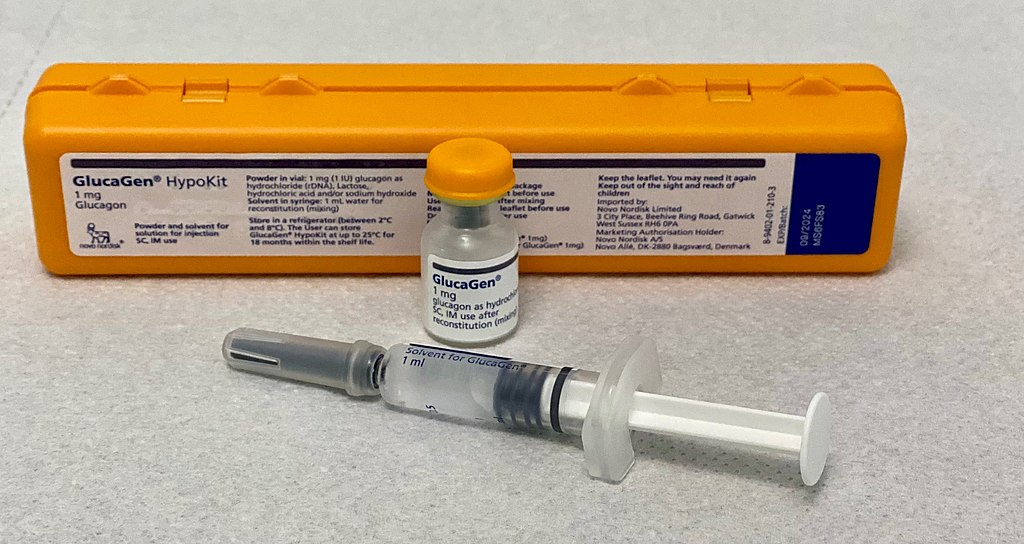
Glucagon
Glucagon is given to reverse hypoglycaemia when other routes are not possible.
Glucagon is a hormone that converts glycogen to glucose in the liver. This glucose can then be released into the bloodstream and utilised by the body.
Hypoglycaemia
Hypoglycaemia should always be considered in patients presenting with a reduced level of consciousness. It presents with autonomic features (early) and neurological features (late).
Autonomic features of hypoglycaemia include:
- Sweating
- Palpitations
- Tremor
- Hunger
Neurological features of hypoglycaemia include:
- Confusion
- Drowsiness
- Behavioural changes
- Speech abnormalities
- Incoordination
Administration
- Intramuscular
- Typically comes in a kit containing a vial of glucagon and a pre-filled syringe of water, which should be mixed before administration
Key considerations
- It can take up to 15 minutes to take effect and is short-lived, so follow-up treatment (e.g. carbohydrates) is required
- Less effective for patients with a history of starvation, hepatic disease, the very young, older people or those who have recently used glucagon already
- Contraindicated in pheochromocytoma, a rare type of neuroendocrine tumour
Glucose 10%
10% glucose is given to reverse hypoglycaemia, when oral glucose administration is impossible and rapid clinical improvement is required. It should also be given if patients have not responded to the administration of IM glucagon after 10 minutes.
Administration provides direct delivery of glucose to the systemic circulation.
Administration
- Intravenous or intraosseous
- Glucose and saline fluid bags are commonly confused as they are clear fluids – STOP and CHECK before administration
Key considerations
- It must not be given by intramuscular or subcutaneous injection
- Intraosseous administration should be avoided if possible due to the risk of osteomyelitis
Glucose 40% oral gel
40% glucose is given to reverse hypoglycaemia in a conscious patient without choking or aspiration risk.
Administration provides delivery of glucose to the systemic circulation through buccal absorption.
Administration
- Buccal
- Squeeze the gel into the mouth between the teeth and gums
Key considerations
- Risk of choking in patients with altered level of consciousness; it can be administered by soaking a gauze swab and placing it between the patient’s lip and gum
Glyceryl trinitrate
Glyceryl trinitrate (GTN) is given to relieve cardiac chest pain (due to angina/myocardial infarction) and chest pain due to cocaine toxicity. It is also used in acute heart failure with ischaemia or uncontrolled hypertension.
Administration
- Sublingual
- Give a tablet or spray under the patient’s tongue and close the mouth
Key considerations
- Not given when systolic blood pressure is below 90mmHg in cardiac chest pain or below 110mmHg in acute heart failure
- Not given to patients who have taken sildenafil (Viagra) in the previous 24 hours
Hydrocortisone
Hydrocortisone is given for severe or life-threatening asthma and chronic obstructive pulmonary disease (COPD) exacerbations. It is also given to treat or prevent adrenal crises in patients with adrenal insufficiency.
In asthma and COPD, there is inflammation within the airways. Hydrocortisone is a steroid which inhibits the accumulation of inflammatory cells and prevents tissue response to inflammatory processes.13
In an adrenal crisis, hydrocortisone replaces a lack of cortisol and restores blood pressure, blood sugar, cardiac synchronicity and volume.
Patients with adrenal insufficiency (e.g. Addison’s disease) may have a personal supply of hydrocortisone for use in an emergency, which can be given if readily available.
Administration
- Intravenous or intramuscular
- Give slowly over at least 2 minutes when administering intravenously
Key considerations
- It may cause a burning or stinging sensation
Ibuprofen
Ibuprofen is given for mild to moderate pain, particularly from musculoskeletal causes, as part of the first steps in the analgesic ladder.14 It can also be used for pyrexic patients with associated discomfort.
Ibuprofen reduces prostaglandin and brings an analgesic, antipyretic and anti-inflammatory effect.
Administration
- Oral
- It should be given after the patient has eaten
Key considerations
- Taking ibuprofen in large doses or for a long time can increase stomach acid and irritate the stomach lining, causing problems such as gastric ulcers
- There are several contraindications and cautions for ibuprofen, particularly related to renal and gastrointestinal factors
Ipratropium bromide
Ipratropium bromide is given to treat severe asthma, exacerbations of COPD or an expiratory wheeze.
Ipratropium bromide is an anticholinergic that blocks the activity of muscarinic receptors, helping to relax smooth muscle. This causes bronchodilation and fewer secretions in the airways to relieve respiratory symptoms. It has a particular benefit in COPD or for children suffering from acute asthma.
Beta-2 agonists (such as salbutamol) generally work more quickly in asthmatic patients and are typically administered before ipratropium bromide.
Administration
- Nebulised with 6-8 litres per minute oxygen
- In COPD, limit oxygen-driven nebulisation to 6 minutes to reduce the risk of type 2 respiratory failure (JRCALC advise a further 6 minutes can be given if indicated)
Key considerations
- In an emergency, it should be given whilst en route to a suitable receiving hospital
- Protect the eyes from the mist, as it can cause visual problems and worsen glaucoma
Methoxyflurane (Penthrox®)
Methoxyflurane is given to treat moderate to severe pain in adult patients with traumatic injuries.
Methoxyflurane is an analgesic which can be used as a non-opioid alternative or in conjunction with morphine for very severe pain. It is believed to reduce pain signal conduction across gap junctions.
Administration
- Inhaled
- Ensure the charcoal filter is fitted to the inhaler before administration
- Relief begins after 6–8 breaths and continues for several minutes
- Each dose lasts approximately 30 minutes
Key considerations
- Not given to patients with liver or kidney disease, respiratory depression or cardiovascular instability
- Not given to patients with history or family history of severe reactions to inhaled anaesthetics
Metoclopramide hydrochloride
Metoclopramide is given to treat nausea and/or vomiting or to prevent these symptoms following the administration of opiates (e.g. morphine).
Metoclopramide is an anti-emetic that blocks central and peripheral dopamine-2 receptors, reducing vomiting or the feeling of nausea.
Administration
- Intravenous or intramuscular
- Give slowly over 3 minutes when administering intravenously
Key considerations
- It must not be given in the same syringe as, or mixed with, morphine sulphate
Midazolam
Midazolam is given for seizures where the convulsions are prolonged or repeated.
Midazolam is a benzodiazepine with anticonvulsant, anxiolytic and sedative properties. It can be administered more quickly than diazepam with similar effectiveness, therefore is preferred over intravenous diazepam for the initial treatment.15
Administration
- Buccal
- The patient may have midazolam prescribed, and the clinician must follow the prescriber’s instructions; otherwise, a PGD is required
- Usually effective within 5 minutes, the sedative effect decreases after 15 minutes
Key considerations
- Give with caution where there has been use of alcohol, opioids or other central nervous system depressants due to the risk of respiratory depression
Misoprostol
Misoprostol is given for post-partum haemorrhage (PPH) or a confirmed miscarriage under 24 weeks pregnant with life-threatening bleeding. It is the first-line drug for PPH in pre-eclampsia or hypertension, as syntometrine is contraindicated.
Misoprostol binds to smooth muscle cells in the uterine lining to increase the strength and frequency of contractions. This helps reduce blood loss from uterine blood vessels.
Administration
- Sublingual or rectal
Key considerations
- It must only be given if the haemorrhage cannot be controlled with uterine massage
- Do not administer before the birth of the baby or if there is any suspicion that the foetus or embryo is in the uterus
Morphine sulphate
Morphine is given to treat pain, as one of the latter steps in the analgesic ladder, and is the analgesic of choice for suspected myocardial infarction. There are additional times when morphine may be used for patients at the end of life, in liaison with palliative care teams or senior clinical support.
Morphine is a strong opioid analgesic which blocks the transmission of pain signals to the central nervous system. It also has vasodilatory, sedative and euphoric effects. Its effects on the central nervous system can also cause respiratory depression.
Morphine is a class A controlled drug held under strict medication management procedures.
Administration
- Intravenous, intraosseous, intramuscular, subcutaneous or oral
- Administer slowly and titrate to effect up to the maximum initial dose
- Smaller doses should be considered for patients under 50kg or those who are frail
Key considerations
- Not given to patients with systolic blood pressure less than 90mmHg
- Not given to patients with respiratory depression, and great caution should be taken in patients with any respiratory problems or chest injuries
- Not given to patients with head injuries with a significantly impaired level of consciousness
Naloxone hydrochloride
Naloxone is given for opioid/opiate toxicity to reverse respiratory depression.
Naloxone is an opioid antagonist and binds to opioid receptors.
Patients recently exposed to high-potency preparations of opioids, such as those used in veterinary medicine or anaesthetics, should be administered naloxone urgently, even if asymptomatic.
Opioid overdose triad
The typical clinical triad of opioid overdose is:
- Decreased level of consciousness
- Respiratory depression
- Pin-point pupils (miosis)
Administration
- Intravenous, intraosseous, intramuscular, subcutaneous or intranasal
Key considerations
- In opioid-dependent patients, it may precipitate violent withdrawal symptoms, including cardiac arrhythmias. Titrate the dose to leave the patient in a ‘groggy’ state
Nitrous oxide (Entonox®)
Nitrous oxide is given to treat moderate to severe pain as part of the medial steps in the analgesic ladder, including during labour.
Nitrous oxide has an analgesic action by activating opioid receptors in the midbrain.
Administration
- Inhaled
- Self-administered, and the effects rapidly wear off once administration is halted
Key considerations
- May be harmful in body cavities, as it will expand and increase the pressure
- Not administered for a suspected pneumothorax, severe head injuries with impaired consciousness, decompression sickness (the bends), suspected intestinal obstruction or if the patient has had a recent intraocular gas injection

Ondansetron
Ondansetron is given to treat nausea and/or vomiting or to prevent these symptoms following the administration of opiates (e.g. morphine).
Ondansetron is an anti-emetic that blocks 5HT-3 serotonin receptors centrally and in the vagus nerve to block triggers from the gastrointestinal tract.16
Administration
- Intravenous or intramuscular
- Give slowly over 2 minutes when administering intravenously
Key considerations
- Not given to those with congenital long QT syndrome
- Give with caution to those with existing prolonged QT intervals, especially when on other prolonging medications
- It must not be given in the same syringe as, or mixed with, morphine sulphate
Oxygen
Oxygen is given to treat significant illnesses or injuries requiring supplemental oxygen or if the patient is hypoxaemic.
Oxygen assists in reversing hypoxia by raising the concentration of inspired oxygen. Oxygen is essential for cell metabolism and normal tissue physiological functioning.
Administration
- Inhaled
- Once administered, titrate for target saturation within the 94–98% range
- The target saturation range for patients with COPD is 88-92%, or as specified on an alert card
- Patients with suspected carbon monoxide poisoning should be administered high-flow oxygen regardless of saturation reading
Key considerations
- In patients with conditions that cause hypercapnia, such as COPD, there is a risk that higher doses can cause type 2 respiratory failure
- Be careful of the fire and explosive hazard of oxygen and safety measures related to the cylinder
For more information, see the Geeky Medics guides to oxygen administration and oxygen prescribing.
Paracetamol
Paracetamol is given to treat mild to moderate pain, as part of the first steps in the analgesic ladder (oral form), or for patients in moderate to severe pain (intravenously) to balance opioid requirements. It can also be used for pyrexia with associated discomfort.
Paracetamol activates descending serotonergic pathways and partly inhibits prostaglandin, resulting in an analgesic and antipyretic effect.17 It does not suppress inflammation.18
Administration
- Intravenous or oral
- Give intravenous dose over 15 minutes
Key considerations
- Check whether the patient has taken paracetamol, or paracetamol–containing product, in the past 4 hours or has consumed the maximum cumulative dose in the past 24 hours
Prednisolone
Prednisolone is given to treat moderate, severe or life-threatening exacerbations of asthma or an exacerbation of COPD. It is given when the patient has had no or little improvement to nebulised salbutamol and ipratropium bromide.
Prednisolone is a steroid which inhibits the accumulation of inflammatory cells and prevents tissue response to inflammatory processes, reducing inflammation within the airways.
It has the same indications as hydrocortisone but is used in more moderate cases and taken orally.
Administration
- Oral
Key considerations
- Not given to patients with signs or symptoms of systemic infection
Salbutamol
Salbutamol is given to treat acute asthma attacks, exacerbation of COPD or expiratory wheezing from lower airway causes such as allergy, anaphylaxis or smoke inhalation.
Salbutamol is a beta-2 adrenoceptor agonist. These receptors are abundant in the smooth muscle of the airways, and activation causes relaxation, reducing bronchoconstriction in the medium and smaller airways.
Administration
- Inhaled or nebulised
- In COPD, limit nebulisation to 6 minutes (JRCALC advise a further 6 minutes can be given if indicated)
Key considerations
- Not indicated for bronchiolitis as it provides little benefit
- May cause tachycardia, palpitations or tremors
- Half doses should be used in patients on beta-blockers due to the risk of severe hypertension
Sodium chloride 0.9%
Sodium chloride is given as fluid replacement therapy in various medical and trauma conditions, typically in response to hypotension. It is also used to confirm successful cannulation and as a flush following drug administration.
Sodium chloride is a mixture of salt and water that replaces circulatory volume, raising cardiac output and improving perfusion.
Administration
- Intravenous or intraosseous
Key considerations
- For patients with heart failure, use with caution as it can exacerbate pulmonary oedema
Syntometrine
Syntometrine is given to treat post-partum haemorrhage within 24 hours of delivery or for a confirmed miscarriage with subsequent life-threatening bleeding.
Syntometrine is a combination of ergometrine and oxytocin. It directly stimulates the uterine muscle, causing contraction, which helps prevent blood loss from uterine vessels.
It can be given in addition to misoprostol unless contraindicated, as it reduces bleeding through a different pathway.
Administration
Key considerations
- It must only be given if the haemorrhage cannot be controlled with uterine massage
- Do not administer before the birth of the baby or if there is any suspicion that the foetus or embryo is in the uterus
- Not given in the presence of hypertension or severe pre-eclampsia
Ticagrelor
Ticagrelor is given for myocardial infarction.
Ticagrelor is an antiplatelet that blocks P2Y12 receptors, reducing the size of a developing blood clot to decrease the damage caused during a myocardial infarction.19
Administration
- Oral
Key considerations
- Not given to patients actively bleeding or at increased risk of bleeding, including those that have taken anticoagulant medication within 24 hours
- Not given to those with 2nd or 3rd-degree atrioventricular block or sick sinus syndrome unless they have a pacemaker fitted
Tranexamic acid
Tranexamic acid (TXA) is given for severe traumatic haemorrhage, which may be internal or external. It is also given for post-partum haemorrhage and patients with head injuries with a GCS of 12 or less.
Tranexamic acid inhibits the lysine receptor to prevent plasmin from binding, thus helping the body to form and maintain blood clots. When bleeding occurs within the brain, this can increase pressure causing further damage. Tranexamic acid has been shown to reduce deaths from head injuries.20
Administration
- Intravenous, intraosseous or intramuscular
- Administer within 3 hours of injury
- Post-partum haemorrhage may occur up to 24 hours after delivery, and TXA should be given after a uterotonic drug (i.e. misoprostol/syntometrine)
- Give slowly over 10 minutes when administering through intravenous or intraosseous routes
Key considerations
- It must only be administered after any critical interventions, such as airway management or application of a tourniquet
Reviewer
James Green
Paramedic
Editor
Dr Chris Jefferies
References
- Association of Ambulance Chief Executives (AACE), Joint Royal Colleges Ambulance Liaison Committee (JRCALC). JRCALC Clinical Guidelines 2022. Published in 2022.
- National Institute for Health and Care Excellence. British National Formulary. Published in 2023. Available from: [LINK].
- Silberman, J., Galuska, M.A. and Taylor, A. Activated Charcoal. Published in February 2023. Available from: [LINK].
- Resuscitation Council UK. Emergency Treatment of Anaphylaxis. Published in May 2021. Available from: [LINK].
- Elwood, P.C., Morgan, G., Woollard, M. and Beswick, A.D. ‘Time is muscle’: aspirin taken during acute coronary thrombosis. Published in July 2010. Available from: [LINK].
- Rothwell, P.M. et al. Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: time-course analysis of randomised trials. Published in May 2016. Available from: [LINK].
- McLendon, K. and Preuss, C.V. Atropine. Published in September 2022. Available from: [LINK].
- BMJ. Penicillin allergy—getting the label right. Published in August 2017. Available from: [LINK].
- Tidy, C. Croup. Published in August 2021. Available from: [LINK].
- Gates, A. et al. Glucocorticoids for croup in children. Published in August 2018. Available from: [LINK].
- Nicholson, M.W. et al. Diazepam-induced loss of inhibitory synapses mediated by PLCδ/ Ca2+/calcineurin signalling downstream of GABAA receptors. Published in June 2018. Available from: [LINK].
- Castle, J.R. et al. Effect of Repeated Glucagon Doses on Hepatic Glycogen in Type 1 Diabetes: Implications for a Bihormonal Closed-Loop System. Published in September 2015. Available from: [LINK].
- Shorr, R.I., Hoth, A.B. and Rawls, N. Drugs for the Geriatric Patient: Hydrocortisone. Published in 2007.
- National Institute for Health and Care Excellence. Analgesia – mild-to-moderate pain. Published in November 2021. Available from: [LINK].
- McMullan, J., Sasson, C., Pancioli, A. and Silbergleit, R. Midazolam Versus Diazepam for the Treatment of Status Epilepticus in Children and Young Adults: A Meta-Analysis. Published in June 2010. Available from: [LINK].
- Griddine, A. and Bush J.S. Ondansetron. Published in February 2023. Available from: [LINK].
- Anderson, B.J. Paracetamol (Acetaminophen): mechanisms of action. Published in October 2008. Available from: [LINK].
- Graham, G.G. and Scott K.F. Mechanism of Action of Paracetamol. Published in January 2005. Available from: [LINK].
- Teng, R. Ticagrelor: Pharmacokinetic, Pharmacodynamic and Pharmacogenetic Profile: An Update. Published in June 2015. Available from: [LINK].
- Roberts, I. et al. Tranexamic acid to reduce head injury death in people with traumatic brain injury: the CRASH-3 international RCT. Published in April 2021. Available from: [LINK].
Image references
- Figure 1. Whispyhistory. Benzylpenicillin vial. License: [CC BY-SA]
- Figure 2. Whispyhistory. Glucagen with case. License: [CC BY-SA]
- Figure 3. Owain.davies. Entonox cylinder and giving set. License: [CC BY]




