- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Thyroid cancer is a malignancy of the thyroid gland. There are 3,900 new thyroid cancer cases diagnosed annually in the UK, making it the 20th most common cancer in the UK.1
Thyroid nodules and goitre are common; many are picked up incidentally on imaging, and most are benign. A nodule is a term used to define a firm lump underneath the skin, usually greater than 1cm. A goitre is a term used to describe a swelling in the neck due to the enlargement of the thyroid gland.
This article will cover the classification, assessment and management of thyroid cancer. You may also be interested in our OSCE guide to performing a neck lump examination.
Aetiology
Anatomy
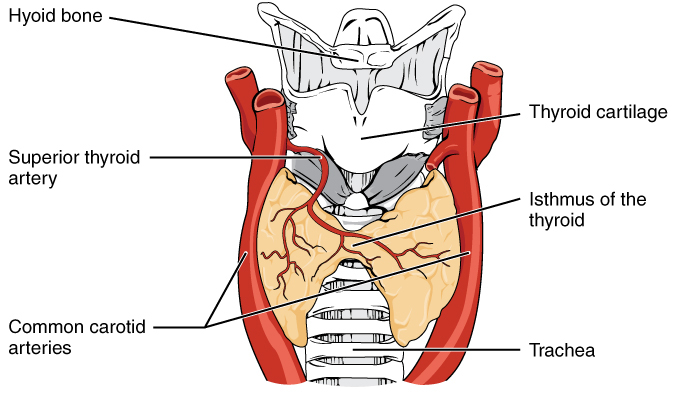
The thyroid gland is an endocrine gland situated in the anterior midline of the neck, just anteroinferior to the larynx. It consists of a right and a left lobe, connected by a central isthmus. The isthmus overlies the second to fourth tracheal rings. It is surrounded by the pre-tracheal fascia in the neck.2
The thyroid gland receives arterial supply from the superior and inferior thyroid arteries, branches of the external carotid artery and the thyrocervical trunk of the subclavian artery, respectively. Occasionally some individuals will have a thyroid ima artery, arising from the brachiocephalic trunk.
Venous drainage of the thyroid gland is via the superior, middle and inferior thyroid veins. The superior and middle veins drain into the internal jugular vein, while the inferior thyroid vein drains into the brachiocephalic vein.3
The thyroid gland receives sympathetic innervation from the sympathetic chain. The sympathetic innervation has vasomotor control of the thyroid gland, but the pituitary gland regulates the secretory function. Lymphatic drainage is to the paratracheal and deep cervical lymph nodes3.
The thyroid gland is an endocrine organ comprising follicular cells and parafollicular cells. Follicular cells produce thyroid hormone (T3/T4) and surround a central colloid. Parafollicular cells are involved in the production of calcitonin, which works to reduce serum calcium.
Classification of thyroid cancer
Thyroid cancers are characterised according to their morphology.
The most common subtype is papillary thyroid cancer (accounting for 90%). This characteristically spreads via lymphatics and can commonly present as a neck node. It is associated with radiation exposure.4
The second most common is follicular carcinoma. This is more likely to present with thyroid swelling and has a haematogenous route of spread.
Medullary thyroid carcinoma is a cancer of the calcitonin cells associated with multiple endocrine neoplasia type 2A (MEN 2A). These patients are more likely to have a family history and may also have other features of MEN 2A (e.g. hypertension secondary to a phaeochromocytoma).4
Anaplastic thyroid carcinoma is an undifferentiated thyroid cancer. It is characterised by aggressive disease and metastases at presentation. It has a poor prognosis, and survival following diagnosis is usually limited to several months only.
Lymphoma is another cancer subtype that can occur in the thyroid gland. This is associated with Hashimoto’s thyroiditis, an inflammatory thyroid disease.
Risk factors
Risk factors for thyroid cancer include:1
- Female sex (the reason for this is unclear)
- Obesity
- Benign thyroid disease (Hashimoto’s, thyroid adenomas, a goitre)
- Radiation exposure (thyroid gland is sensitive to radiation)
- Family history (certain genetic disorders such as multiple endocrine neoplasia)
- Systemic lupus erythematosus (SLE)
Clinical features
History
Typical symptoms of thyroid cancer include:
- Neck lump
- Hoarse voice
- Dysphagia
- Odynophagia
- Dyspnoea
- Stridor
General symptoms may include:
- Weight loss, anorexia
- Lethargy, fatigue
- Diarrhoea
- Bone pain (metastatic disease)
- Pulsatile lesion (metastatic disease)
Clinical examination
All patients with a goitre or neck lump require a full neck examination. If there is concern that the lump arises from the thyroid, a thyroid status examination should be performed.
Typical clinical findings may include:
- General cachexia
- Neck lump
- Thyroid goitre
- Stridor or hoarseness
Assessing thyroid nodules
When assessing a thyroid nodule, features that increase suspicion of malignancy include:
- Age <20 years or >60 years
- Firmness of nodule
- Rapid growth
- Fixed to adjacent structures
- Vocal cord paralysis
- Regional lymphadenopathy
- History of neck irradiation
- Family history of thyroid cancer
Differential diagnoses
Thyroid cancer typically presents as a thyroid lump, hoarseness/voice changes, shortness of breath and/or systemic features (weight loss, anorexia).
These symptoms have a wide range of potential causes which must be considered.
Neck lump
Other possible causes of a neck lump include:
- Benign thyroid disease
- Thyroglossal cyst
- Lymphadenopathy secondary to another cancer (e.g. Virchow’s node & gastric cancer) or infection
Hoarseness
Other possible causes of hoarseness include:
- Laryngitis
- Laryngeal cancer
- Post-operative complication (e.g. following neck surgery)
Shortness of breath
Other possible causes of shortness of breath include:
- Chest infection
- Exacerbation of asthma or COPD
- Pleural effusion
- Pulmonary embolism
- Cardiac causes (e.g. myocardial infarction)
Investigations
Bedside investigations
Relevant bedside investigations include:
- ECG: endocrine disorders of the thyroid gland can cause arrhythmias (e.g. hyperthyroidism and atrial fibrillation)
- Urinalysis: the presence of urinary catecholamines may indicate a phaeochromocytoma or paraganglioma, which may indicate a diagnosis of MEN
Laboratory investigations
Relevant laboratory investigations include:
- Thyroid function tests: thyroid cancer is usually associated with a euthyroid state; however, advanced cancers can cause hypothyroidism (due to the destruction of healthy thyroid tissue) or hyperthyroidism (due to the presence of more active cells)
- Thyroid autoantibodies
- Plasma calcitonin and carcinoembryonic antigen (CEA): if suspicious for MEN
Genetic testing may be indicated in the presence of a strong family history or with a diagnosis of medullary thyroid cancer (due to its association with MEN)
Imaging
Relevant imaging investigations include:
- Ultrasound: all patients with a thyroid lump require an ultrasound scan. Radiological features of the lump are utilised, as part of the British Thyroid Association ‘U’ classification, to determine the risk of malignancy and whether fine needle aspiration (FNA) is required.
- Cross-sectional imaging (MRI/CT): performed for retrosternal disease or if suspicious of metastatic disease
Fine needle aspiration cytology (FNAC)
Fine needle aspiration involves aspirating a thyroid tissue sample under ultrasound guidance. FNA cytology results are graded using the Thy classification.5
Table 1. Fine needle aspiration cytology score (Thy classification) and clinical interpretation.
| FNAC score | Interpretation | Management |
| Thy1 | Non-diagnostic | Repeat FNAC |
| Thy2 | Benign | Reassuring if this aligns with the ultrasound findings, no further action may be required |
| Thy3 | Equivocal | Repeat FNAC or diagnostic hemithyroidectomy (removing half the thyroid gland containing the nodule to reach a tissue diagnosis) |
| Thy4 | Suspicious for malignancy | Diagnostic hemithyroidectomy |
| Thy5 | Malignant | Managed according to tumour type and MDT outcome |
Additional investigations
Additional relevant investigations may include:
- Flow-volume loop studies: for assessment of upper airway obstruction
Diagnosis
The diagnosis of thyroid cancer is made with the above investigations. The outcome of imaging and FNAC guides the management of thyroid cancer.
Staging
Thyroid cancer staging is used during MDT discussion to prognosticate and decide on appropriate management. This is calculated with findings from cross-sectional imaging. Like most cancers, thyroid cancer uses the TNM staging classification.1
| TMN | Classification | |
| T | Tx | Tumour cannot be assessed |
| T0 | No tumour | |
| T1a T1b |
Inside the thyroid gland, <1cm Inside the thyroid gland, 1-2cm |
|
| T2 | Inside thyroid, 2-4cm | |
| T3a T3b |
Inside thyroid, >4cm Extra-thyroid spread to strap muscles, any size |
|
| T4a T4b |
Soft tissue invasion – trachea, larynx, oesophagus Neck vessel invasion or spinal invasion |
|
| N | Nx | No information about lymph node spread. |
| N0 | No lymph node spread | |
| N1a
N1b |
Spread to pretracheal, paratracheal, prelaryngeal lymph or superior mediastinal nodes Spread to cervical or retropharyngeal nodes |
|
| M | M0 | No distant metastatic spread |
| M1 | Distant metastatic spread present |
Management
Referral
If a patient presents with a suspected thyroid lump or goitre and acute airway compromise, they should be reviewed urgently in the emergency department.
NICE advises considering a 2-week wait (urgent suspected cancer) referral for all patients with an unexplained thyroid lump, especially if they have red flag features:
- Unexplained hoarseness or voice changes
- Associated lymphadenopathy
- Sudden onset of an expanding painless thyroid mass
- Any other red flags of malignancy
- Compressive symptoms of dysphagia, or breathlessness
Surgical management
The primary treatment modality for thyroid cancer is surgery. There is a role for adjuvant therapy in certain cases.
A diagnostic hemithyroidectomy is performed when the FNAC is suspicious but not diagnostic. Once the diagnosis of malignancy is confirmed, suitable patients will be offered a completion thyroidectomy +/- neck dissection.

Patients with differentiated thyroid cancer may be offered radioactive remnant ablation (RAA). This radioactive treatment destroys residual cells in the thyroid bed that may still be present. The use of this in medullary or anaplastic thyroid cancer is less proven.
Anaplastic thyroid cancer is generally at an advanced stage at diagnosis, and this limits treatment options. Patients may be offered surgery with chemoradiotherapy or immunotherapy, depending on the MDT decision.
Patients who have undergone total thyroidectomy will require life-long thyroxine replacement. If the parathyroids have been removed, patients may also require calcium replacement.
Serum thyroglobulin is a marker used to monitor for signs of disease recurrence. This protein is only produced by follicular cells. When raised, it is suspicious for disease recurrence and should prompt further investigation.
Complications
Complications related to cancer
Complications of thyroid cancer can include:
- Shortness of breath
- Hoarseness
- Upper airway obstruction
- Dysphagia
- Odynophagia
- Metastasis
- Death
Complications of surgical management
Complications related to surgical management of thyroid cancer include:
- Bleeding: expanding neck haematoma is a surgical emergency
- Infection
- Recurrent laryngeal nerve damage: hoarseness or stridor if bilaterally
- The need for lifelong thyroid hormone replacement and monitoring of thyroid function tests
- The need for calcium/vitamin D replacement
- The need for further procedures: completion thyroidectomy, adjuvant RAA
Key points
- Thyroid cancer is a malignancy that affects the thyroid gland, an endocrine organ responsible for regulating metabolism
- Thyroid cancers are categorised based on their morphology; the most common subtype is papillary thyroid cancer (90% of cases), which is associated with radiation exposure
- Risk factors for thyroid cancer include female sex, obesity, benign thyroid disease, radiation exposure, certain genetic disorders, and systemic lupus erythematosus (SLE)
- Symptoms of thyroid cancer include neck lump (most common presentation), hoarse voice, dysphagia, odynophagia, dyspnoea, stridor, weight loss, anorexia, lethargy, fatigue, diarrhoea, and bone pain (in case of metastatic disease)
- All patients require ultrasound imaging of the neck, with FNA cytology for suspicious neck lumps
- Surgery is the mainstay of treatment for thyroid cancer, and adjuvant radioactive ablation is used in certain situations
- Complications of thyroid surgery include the need for lifelong thyroid hormone replacement and injury to the recurrent laryngeal nerve
Reviewer
Miss Sarah Ellis
ENT ST3
Editor
Dr Chris Jefferies
References
- Cancer Research UK. July 2023. Available from: [LINK]
- StatPearls. Anatomy, Head and Neck. July 2022. Available from: [LINK]
- Surgeon’s Approach to the Thyroid Gland: Surgical Anatomy and the Importance of Technique. R Bliss et al. World J of Surg. 2000.
- Katoh, H., Yamashita, K., Enomoto, T., & Watanabe, M. (2015). Classification and general considerations of thyroid cancer. Ann Clin Pathol, 3(1), 1045.
- Guidance on the reporting of thyroid cytology specimens. Royal College of Pathologists. 2016. Available from: [LINK]
Image references
- Figure 1. CFCF. Diagrammatic view of thyroid gland. License: [CC BY-SA]
- Figure 2. Marco Biffoni. Thyroid gland tumour. License: [CC BY-SA]




